Acinetobacter baumannii: Difference between revisions
m fixed weird typo |
|||
| Line 25: | Line 25: | ||
url =http://www1.wfubmc.edu/medicalcenter/pp/ID/04/040419a.ppt# | |
url =http://www1.wfubmc.edu/medicalcenter/pp/ID/04/040419a.ppt# | |
||
accessdate= 2007-10-03}}</ref> |
accessdate= 2007-10-03}}</ref> |
||
:p |
|||
== Transmission and Prevalence == |
== Transmission and Prevalence == |
||
Revision as of 21:52, 6 October 2008
| Acinetobacter baumannii | |
|---|---|
| |
| Acinetobacter baumannii | |
| Scientific classification | |
| Kingdom: | |
| Phylum: | |
| Class: | |
| Order: | |
| Family: | |
| Genus: | |
| Species: | A. baumannii
|
| Binomial name | |
| Acinetobacter baumannii | |
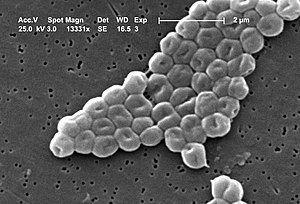
Acinetobacter baumannii is a species of pathogenic bacteria called aerobic gram-negative bacillus and is naturally sensitive to relatively few antibiotics. A.baumannii forms opportunistic infections.[1] There have been many reports of A. baumannii infections among American soldiers wounded in Iraq.[2] Multi-drug resistant Acinetobacter baumannii' is abbreviated as MDRAB. Multidrug-resistant Acinetobacter is not a new phenomenon, but A baumannii has always been inherently resistant to multiple antibiotics.
Biology
- See also the main article on the Acinetobacter genus
Acinetobacter baumannii is the most relevant human pathogen within the Acinetobacter genus. Most A. baumannii isolates are multiresistant, containing in their genome small, isolated islands of alien (meaning transmitted genetically from other organisms) DNA and other cytological and genetic material; this has led to more virulence.[1] Acinetobacter have no flagellum; the name is Greek for 'motionless'.[3]
Transmission and Prevalence
Acinetobacter enters into the body through open wounds, catheters, and breathing tubes. It usually infects those with compromised immune systems, such as the wounded, the elderly, children or those with immune diseases. Colonization poses no threat to people who aren't already ill, but colonized health care workers and hospital visitors can carry the bacteria into neighboring wards and other medical facilities.[4] The number of nosocomial infections (hospital-acquired infections) caused by A. baumannii has increased in recent years.[5]
The first military outbreaks of severe A. Baumannii infections occurred in April, 2003 in American soldiers returning from Iraq. Early reports attributed the infections to the Iraqi soil. Later testing demonstrated widespread contamination of field hospitals as the most plausible vector.[6]
Virulence and Pathogenicity
This opportunistic pathogen causes a wide variety of serious infections in humans, mostly in compromised patients. Recently, A. baumannii has emerged as an important pathogen among wounded soldiers, threatening civilian and military patients.
Nosocomial A. baumannii bacteremia may cause severe clinical disease that is associated with a high mortality rate of up to 75%.[7] This opportunistic pathogen expresses a myriad of factors that could play a role in human pathogenesis. Among these factors are the attachment to and persistence on solid surfaces, the acquisition of essential nutrients such as iron, the adhesion to epithelial cells and their subsequent killing by apoptosis, and the production and/or secretion of enzymes and toxic products that damage host tissues. However, very little is known about the molecular nature of most of these processes and factors and almost nothing has been shown with regard to their role in bacterial virulence and the pathogenesis of serious infectious diseases. Fortunately, some of these gaps can now be filled by testing appropriate isogenic derivatives in relevant animal models that mimic the infections in humans, particularly the outcome of deadly pneumonia. Such an approach should provide new and relevant information on the virulence traits of this normally underestimated bacterial human pathogen.[1]
Control and Treatment of Infections
Multi-resistant A. baumannii infections are currently treated with imipenem and an older class of drugs known as polymyxins. These, along with stricter infection-control measures, such as monitored hand washing, have lowered infection rates in some military hospitals.[6]
MDRAB infections are difficult and costly to treat. A study at a public teaching hospital found that the mean total hospital cost of patients who acquired MDRAB was $98,575 higher than that of control patients who had identical burn severity of illness indices.[8]
References
- ^ a b c Gerischer U (editor). (2009). Acinetobacter Molecular Biology (1st ed. ed.). Caister Academic Press. ISBN 978-1-904455-20-2 .
{{cite book}}:|author=has generic name (help);|edition=has extra text (help) Cite error: The named reference "Gerischer" was defined multiple times with different content (see the help page). - ^ "Acinetobacter baumannii in Iraq". Retrieved 2007-02-15.
- ^ Asif Zia (2004-04-19). "Infectious Disease Case Conference". Wake Forest University. Retrieved 2007-10-03.
- ^ Steve Silberman (2007). "The Invisible Enemy". Wired. Retrieved 2007-02-15.
{{cite news}}: Unknown parameter|month=ignored (help) - ^ The Coalition of the Contaminated. "Mapping Acinetobacter baumannii from Iraq to Civilian Hospitals". Retrieved 2007-10-03.
- ^ a b Jia-Rui Chong (2007-10-01). "The path of war sets doctors on the warpath of disease". Napa Valley Register. Retrieved 2007-10-03.
- ^ Cisneros J, Reyes M, Pachón J, Becerril B, Caballero F, García-Garmendía J, Ortiz C, Cobacho A (1996). "Bacteremia due to Acinetobacter baumannii: epidemiology, clinical findings, and prognostic features". Clin Infect Dis. 22 (6): 1026–32. PMID 8783704.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link) - ^ Wilson, Stephen (2004). "Direct costs of multidrug-resistant Acinetobacter baumannii in the burn unit of a public teaching hospital". 32 (6): 42–344. Retrieved 2007-10-03.
{{cite journal}}: Cite journal requires|journal=(help); Text "American Journal of Infection Control" ignored (help)
