Memory disorder: Difference between revisions
Psy3330 W10 (talk | contribs) No edit summary |
Psy3330 W10 (talk | contribs) mNo edit summary |
||
| Line 118: | Line 118: | ||
{{memory}} |
{{memory}} |
||
==See also== |
|||
| Line 124: | Line 123: | ||
[[Category:Memory disorders|*]] |
[[Category:Memory disorders|*]] |
||
{{Disease-stub}} |
|||
[[ja:記憶障害]] |
[[ja:記憶障害]] |
||
Revision as of 20:35, 24 March 2010
Memory can be defined as an organism's ability to store, retain, and recall information. Disorders of memory can range from mild to severe, yet are all a result of damage to neuroanatomical structures; either in part or in full. This damage hinders the storage, retention and recollection of memories. Memory disorders can be progressive, including Alzheimer's disease, or they can be immediate including disorders resulting from head injury.
Memory Disorders by Alphabetical Order
Agnosia
Agnosia is the inability to recognize certain objects persons or sounds, yet there are many more specific diagnoses of agnosia. Agnosia is typically caused by damage to the brain (most commonly in the occipital or parietal lobes) or from a neurological disorder. Treatments vary depending on the location and cause of the damage. Recovery is possible depending on the severity of the disorder and the severity of the damage to the brain.[1] Some examples of specific types of Agnosia include: Visual Agnosia, Auditory Agnosia, Prosopagnosia, Somatosensory agnosia, Simultanagnosia, Apraxia, Associative Agnosia, etc.
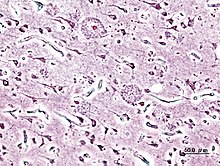
Alzheimer's Disease
Alzheimer's disease (AD) is a progressive, degenerative and fatal brain disease, in which cell to cell connections in the brain are lost. As a result, the death of brain cells occur, therefore giving Alzheimer's disease the title as the most common form of dementia.[2] In the entire world, approximately 1-5% of the population is affected by Alzheimer's disease.[3] It is estimated that 500,000 Canadians currently suffer from Alzheimer’s disease or a related dementia. It is the most significant cause of disability among individuals aged 65 and above.[2] Women are disproportionately the victims of Alzheimer’s disease, with evidence suggesting that women with AD display more severe cognitive impairment relative to age-matched males with AD, as well as a more rapid rate of cognitive decline.[4]
-
PET scan of a healthy brain - Image courtesy of US National Institute on Aging Alzheimer's Disease Education and Referral Center
-
PET scan of brain with AD - Image courtesy of US National Institute on Aging Alzheimer's Disease Education and Referral Center
Amnesia
Amnesia is an abnormal mental state in which memory and learning are affected out of all proportion to other cognitive functions in an otherwise alert and responsive patient.[5] There are two forms of amnesia: Anterograde amnesia and retrograde amnesia, that show hippocampal or medial temporal lobe damage. Anterograde amnesics show difficulty in the learning and retention of information encountered after brain damage. Retrograde Amnesics generally have memories spared about personal experiences or context independent semantic information.[6]
Brain Injury

Traumatic brain injury often occurs from damages to the brain caused by an outside force, and may lead to cases of amnesia depending on the severity of the injury[8]. Head injury can give rise to either transient or persisting amnesia. Occasionally, post-traumatic amnesia (PTA) may exist without any retrograde amnesia (RA), but this is often more common in cases of penetrating lesions. Damage to the frontal or anterior temporal regions have been described to be associated with disproportionate RA. Studies have illustrated that during PTA, head injury patients showed accelerated forgetting of learned information. On the other hand, after PTA, forgetting rates were normal.[8]
In some cases, individuals have reported having a particularly vivid memory for images or sounds occurring immediately before the injury, on regaining consciousness, or during a lucid interval between the injury and the onset of PTA. As a result, recent controversy has emerged about whether severe head injury and amnesia exclude the possibility of post-traumatic stress disorder (PTSD) symptoms. In a study carried out by McMillan (1996), patients reported ‘windows’ of experience, in which emotional disturbance was sufficient to cause PTSD. These 'windows' involved recall of events close to impact (when RA was brief), of distressing events soon after the accident (when PTA was short), or of 'islands' of memory (e.g. hearing the screaming of others).[9][10]
Brain injuries can also be the result of a stroke as the resulting lack of oxygen can cause damage to the location of the cerebrovascular accident (CVA). The effects of a CVA in the left and right hemispheres of the brain include short-term memory impairment, and difficulty acquiring and retaining new information.[11]
Dementia
Dementia refers to a large class of disorders characterized by the progressive deterioration of thinking ability and memory as the brain becomes damaged. Dementia can be categorized as reversible (e.g. thyroid disease) or irreversible (e.g. Alzheimer's disease).[12] Currently, there are more than 35 million people with dementia worldwide. It is estimated that within 20 years, worldwide prevalence will increase two-fold. By 2050, this number is expected to increase to 115 million. Overall, dementia incidence is similar for men and women. However, after 90 years of age dementia incidence declines in men but not in women.[13]
Hyperthymestic Syndrome
Hyperthymestic Syndrome causes an individual to have an extremely detailed autobiographical memory. Patients with this disorder are able to recall events from every day of their lives (with the exception of memories before age five and days that were uneventful). This disorder is very rare with only a few confirmed cases.[14]
Huntington’s Disease
Huntington's Disease is an inherited progressive disorder of the brain that leads to uncontrolled movements, emotional instability, and loss of intellectual faculties."[15] Because of the inheritability of Huntinton's each child born to a parent with Huntington's has a 50% chance of inheriting the disease, leading to a prevalence of almost 1 in 10,000 Canadians (0.01%).[16] The first signs of Huntington's Disease are generally subtle; suffers commonly note tics and twitching as well as unexplained fluctuations of mood. Clumsiness, depression and irritability are noted. What begins as a slurring and slowing of speech eventually leads to difficulty communicating and confinement to a wheelchair or bed.[15]
Parkinson’s Disease
Parkinson’s disease (PD) is a neurodegenerative disease. Movement is normally controlled by dopamine; a chemical that carries signals between the nerves in the brain. When cells that normally produce dopamine die off the symptoms of Parkinson’s appear. The most common symptoms include: tremors, slowness, stiffness, impaired balance, rigidity of the muscles, and fatigue. As the disease progresses, non-motor symptoms may also appear, such as depression, difficulty swallowing, sexual problems or cognitive changes.[17]
According to studies done in London and in Sicily, 1 in 1000 elderly citizens will be diagnosed with Parkinson's[18], although this can vary regionally and affect a large range of age groups.[19]
Cognitive impairment is common in PD. Specific parkinsonian symptoms, bradykinesia and rigidity, have been shown to be associated with decline of cognitive function. The underlying neuropathological disturbance in PD involves selective deterioration of subcortical structures, and the executive dysfunction in PD, especially in processes that involve working memory. This has been shown to be related to decreased activation in the basal ganglia and frontal cortex. Elgh, Domellof, Linder, Edstrom, Stenlund, & Forsgren (2009) studied cognitive function in early Parkinson’s disease and found that PD patients performed significantly worse than healthy controls in attention, episodic memory, category fluency, psychomotor function, visuospatial function and in several measures of executive function. Patients also exhibited greater difficulty with free recall that required a preserved executive function than with cued recall and recognition in tests of episodic memory.[20]
Wernicke-Korsakoff’s Syndrome
Wernicke-Korsakoff syndrome (WKS) is a severe neurological disorder caused by thiamine (vitamin B1) deficiency, and is usually associated with chronic excessive alcohol consumption. It is characterized clinically by oculomotor abnormalities, cerebellar dysfunction and an altered mental state. Korsakoff's syndrome is also characterized by profound amnesia, disorientation and frequent confabulation (making up or inventing information to compensate for poor memory).[21][22] A survey published in 1995 indicated that there was no connection to the national average amount of alcohol ingested by a country in correlation to a range of prevalence within 0 and 2.5%.[23]
Symptoms of Wernicke-Korsakoff Syndrome include confusion, amnesia, and impaired short-term memory. WKS also tends to impair the person’s ability to learn new information or tasks. In addition, individuals often appear apathetic and inattentive and some may experience agitation. WKS symptoms may be long-lasting or permanent and its distinction is separate from acute affects of alcohol consumption and from periods of alcohol withdrawal.[21]
Case Studies
A.J. (patient)
A.J. suffered from a rare memory disorder called hyperthymestic syndrome. She had an inability to forget. Her autobiographical memory was extremely accurate to the point that she remembered every day of her life in detail (with some exceptions). She was unable to control what she remembered or what she forgot. [14]
Clive Wearing
Clive Wearing suffered from anterograde amnesia after a rare case of Herpes Simplex Virus I (HSV-I)which targeted and attacked the spinal column and brain. The virus led to a case of encephalitis which caused the brain damage of his hippocampus, resulting in his amnesia. [24]
HM (patient)
H.M. suffered from epileptic seizures and had his medial temporal lobes surgical removed to prevent or decrease the occurrence of the seizures. After the removal of H.M.'s medial temporal lobes, he suffered from anterograde amnesia as well as moderate retrograde amnesia. H.M. was still able to retain procedural memory after the surgery. [25] [26]
KC (patient)
"The extent of damage to K.C.’s medial temporal lobes, particularly to his hippocampus and parahippocampal gyrus, and associated diencephalic and basal forebrain structures, is in line with his profound impairment on all explicit tests of new learning and memory. There is some uncertainty as to whether this pattern of neurological damage also accounts for his severe remote autobiographical memory loss while sparing his remote spatial memory."[6]
Memory Disorders and Aging
Normal aging, although not responsible for causing memory disorders, is associated with a decline in cognitive and neural systems including memory (long-term and working memory). Many factors such as genetics and neural degeneration have a part in causing memory disorders. In order to diagnose Alzheimer’s disease and dementia early, researchers are trying to find biological markers that can predict these diseases in younger adults. One such marker is a beta-amyloid deposit which is a protein that deposits on the brain as we age. Although 20-33% of healthy elderly adults have these deposits, they are increased in elderly with diagnosed Alzheimer’s disease and dementia.[27]
One study examined dementia severity in elderly schizophrenic patients diagnosed with Alzheimer’s disease and dementia versus elderly schizophrenic patients without any neurodegenerative disorders. In most cases, if schizophrenia is diagnosed, Alzheimer’s disease or some form of dementia in varying levels of severity is also diagnosed. It was found that increased hippocampal neurofibrillary tangles and higher neuritic plaque density (in the superior temporal gyrus, orbitofrontal gyrus, and the inferior parietal cortex) were associated with increased severity of dementia. Along with these biological factors, when the patient also had the apolipoprotein E (ApoE4) allele (a known genetic risk factor for Alzheimer’s disease), the neuritic plaques increased although the hippocampal neurofibrillary tangles did not. It showed an increased genetic susceptibility to more severe dementia with Alzheimer’s disease than without the genetic marker.[28]
As seen in the examples above, although memory does degenerate with age, it is not always classified as a memory disorder. The difference in memory between normal aging and a memory disorder is the amount of beta-amyloid deposits, hippocampal neurofibrillary tangles, or neuritic plaques in the cortex. If there is an increased amount, memory connections become blocked, memory functions decrease much more than what is normal for that age and a memory disorder is diagnosed.[28][27]
The cholinergic hypothesis of geriatric memory dysfunction is an older hypothesis that was considered before beta-amyloid deposits, neurofibrillary tangles, or neuritic plaques. It states that by blocking the cholinergic mechanisms in control subjects you can examine the relationship between cholinergic dysfunction and normal aging and memory disorders because this system when dysfunctional creates memory deficits.[29]
Cultural Perspectives
The pervasiveness of mental health illnesses can be illustrated by looking at the size of the Diagnostic and Statistical Manual IV-TR (DSM IV-TR). Epidemiological studies have shown an increase in mental health cases in Canada alone, as well as globally. In 2050, there could be an epidemic for neurological diseases. [30] With an every growing baby-boom population, and the prevalence of mental illness increasing, an increase in demand for better mental health care is relevant.
Western culture’s gauge of mental illness is determinate on level of dangerousness, competence, and responsibility. [31] This has led to many individuals being refused jobs,[32][33][34][35], are less likely to lease them apartments[36][37][38], and more likely to falsely press criminal charges against them [39][40] While prejudiced views may have started out with a kernel of truth, the level of services available to an ever aging and memory-impaired demographic, will need to increase as well.
With such a stigmatization on memory disorders, and in mental illnesses in general, it can be especially hard for those providing aid for those individuals. Some individuals “are unable to acquire or retain new information, making it difficult or impossible to meet social, family and work-related obligations.”[41] Because of this, there is a large responsibility placed on caregivers (usually children)[42] to uphold economic and emotional upkeeps. While there are services available for these members, very few take the opportunity of these services.[43]
In Asian collectivist cultures focus on the social interactions between members of society. Every individual in the society has a certain role to be fulfilled, and it is deemed socially acceptable to uphold these roles. Furthermore, there is a focus on a balance of body, mind, and spirit. As a result, there is a large descrepency between what should be deemed acceptable treatments for memory disorders that focus on interpersonal relationships and adjustments to others' expectations rather than a Western-led treatment schedule.
One is deemed to be mentally if there is an imbalance of hot-cold/wet-dry, and the proper functioning of the nerves, heart, liver, lungs, kidneys, and spleen.[44] In an event of an imbalance, it can sometimes been seen as a point of beauty as "one is the recipient of others' concern and sympathy."[44]
Popular Culture
In popular media, the world of those with memory disorders is often subject to ridicule and embarrassment. Characters with memory disorders have helped to move literature and media along by allowing for either suspense to be created through retrograde or traumatic amnesia as seen in Alfred Hitchcock’s Spellbound. It can also provide comic relief if one introduces a character who has short-term memory impairments. If humour is defined by the release of dramatic tension, then the humour is largely based on society’s perceptions on those with memory deficits.
Some examples from Movies and television shows that often depict characters suffering from memory disorders include:
- Denny Crane, a character from the television show Boston Legal shows cognitive impairment that could indicative to Alzheimer’s disease.
- Dr. Philip Brainard a character in the movie The Absent-Minded Professor displays mild memory impairment.
- The character Dorey from the movie Finding Nemo shows severe short term memory loss. [35]
- The celebrity and actor Michael J. Fox has been diagnosed with Parkinson’s Disease. [36]
- Iris Murdoch- British writer and philosopher who developed Alzheimer's disease and portrayed by Kate Winslet in the film Iris in 2001.
- U.S. President Ronald Reagan developed Alzheimer's disease.
- The Notebook (2004) the film based on the novel by Nicholas Sparks(1996) a character, Allie Hamilton played by Rachel McAdams that developed Alzheimer's disease.
- Away from Her 2006 film - Alzheimer's disease
Caregiver Syndrome
The health of caregivers of the mentally ill is often overlooked. Caregivers are often forced to give up their jobs and work full time at caring for their ill family member. "These “family caregivers” do work that is complex, physically challenging and critical to a patient’s overall well-being, like dressing wounds, dispensing medication, and feeding, bathing and dressing those who can no longer do so themselves." [45] Family caregivers are more prone to stress related disorders and increased morbidity. "Family caregivers of patients with dementia experience increased physical and psychological morbidity and may develop hyperlipidaemia and insufficiency of the cellular immune system." [46] This syndrome is an indirect result of memory disorders. It is difficult to decrease the prevalence of this disorder because the assistance of doctors and nurses can only go so far. The help of family caregivers is necessary and important in maintaining the well being of the mentally ill.
See Also
References
- ^ National Institute of Neurological Disorders and Stroke. (2007). NINDS Agnosia Information Page. Retrieved on March 8, 2010 from: http://www.ninds.nih.gov/disorders/agnosia/agnosia.htm
- ^ a b Alzheimer’s Disease Statistics. (2005). Alzheimer’s Society of Canada. Retrieved January 27, 2010, from http://alzheimer.ca/english/disease/stats-intro.htm. Cite error: The named reference "alz" was defined multiple times with different content (see the help page).
- ^ World Health Organization. (2001). The world health report 2001 - Mental Health: New Understanding, New Hope. Retrieved March 11, 2010, from World Health Organization International: http://www.who.int/entity/whr/2001/en/whr01_en.pdf
- ^ Dunkin, J.J. (2009). The Neuropsychology of Women. Springer New York, 209-223
- ^ Kopelman, M. D., (2002). Disorders of memory. Brain: A Journal of Neurology. 125(10), 2152-2190. Retrieved from http://journals1.scholarsportal.info.subzero.lib.uoguelph.ca/tmp/2503750871247290410.pdf
- ^ a b Rosenbaum, R.S., Kohler, S., Schacter, D.L., Moscovitch, M., & Westmacott, R. (2005). The Case of k.c.: contributions of a memory-impaired person to memory theory. Neuropsychologia, 43. Retrieved from http://journals1.scholarsportal.info.subzero.lib.uoguelph.ca/tmp/14955255414366644068.pdf
- ^ Centers for Disease Control & Prevention. (2006, January). January 2006 Update: Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Retrieved March 11, 2010, from Centers for Disease Control & Prevention: http://www.cdc.gov/ncipc/pub-res/TBI_in_US_04/CausesTBIUpdate.pdf
- ^ a b The Brain Injury Association of Canada. (2010). A – Introduction to Traumatic Brain Injury. Retrieved March 8, 2010, from http://biac-aclc.ca/en/2010/02/01/a-introduction-to-traumatic-brain-injury/
- ^ McMillan, T.M. (1996). Post-traumatic stress disorder following minor and severe closed head injury: 10 patients. Brain Injury. 10(10), 749-758.
- ^ Kopelman, M. D., (2002). Disorders of memory. Brain: A Journal of Neurology. 125(10), 2152-2190. Retrieved from http://journals1.scholarsportal.info.subzero.lib.uoguelph.ca/tmp/2503750871247290410.pdf
- ^ Heart and Stroke Foundation of Ontario. (2008, August). Effects of a Stroke. Retrieved March 11, 2010, from Heart and Stroke Foundation of Ontario: http://www.heartandstroke.on.ca/site/c.pvI3IeNWJwE/b.3581869/k.8BD1/Stroke__Effects_of_a_stroke.htm
- ^ Rising Tide: The Impact of Dementia on Canadian Society. (2010). Alzheimer’s Society of Canada. Retrieved January 27, 2010, from http://www.alzheimer.ca/docs/RisingTide/Rising%20Tide_Full%20Report_Eng_FINAL_Secured%20version.pdf.
- ^ Ruitenberg, A., Ott, A., van Swieten, J.C., Hofman, A., Breteler, M.M. (2001). Incidence of dementia: does gender make a difference?. Neurobiology of Aging. 22(4), 575-580.
- ^ a b Treffert, Darold, MD. (2010). Hyperthymestic Syndrome: Extraordinary Memory for Daily Life Events. Do we all possess a continuous tape of our lives?. Wisconsin Medical Society. Retrieved on March 8, 2010 from: http://www.wisconsinmedicalsociety.org/savant_syndrome/savant_articles/hyperthymestic_syndrome
- ^ a b Schoenstadt, A. (2006). Huntington’s Disease Statistics. Retrieved January 27, 2010, from http://nervous-system.emedtv.com/huntington%27s-disease/huntington%27s-disease-statistics.html. Cite error: The named reference "stat" was defined multiple times with different content (see the help page).
- ^ Huntington Society of Canada. (n.d.). Huntington Society of Canada. Retrieved March 11, 2010, from Hungtinton: http://www.huntingtonsociety.ca/english/content/?page=91
- ^ Parkinson Society Canada. (2010). What is Parkinson’s?. Retrieved March 8, 2010, from http://www.parkinson.ca/site/c.kgLNIWODKpF/b.5184077/k.CDD1/What_is_Parkinsons.htm
- ^ Nilsen, O., Vossius, C., & Larsen, J. (2010). Acta Neurol Scand, 38-43.
- ^ Michael J. Fox Foundation for Parkinson's Research. (2008, October 10). Living with Parkinson's: Parkinson's 101. Retrieved March 11, 2010, from Michael J. Fox Foundation for Parkinson's Research: http://www.michaeljfox.org/living_aboutParkinsons_parkinsons101.cfm#q1
- ^ Elgh, E., Domellof, M., Linder, J., Edstrom, M., Stenlund, H., & Forsgren, L. (2009). Cognitive function in early Parkinson’s disease: a population-based study. European Journal of Neurology. 16(12), 1278-1284.
- ^ a b Family Caregiver Analysis. (2010). Wernicke-Korsakoff Syndrome. Retrieved on March 8, 2010, from http://www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=580 Cite error: The named reference "FCA" was defined multiple times with different content (see the help page).
- ^ Moriyama, Y., Mimura, M., Kato, M. & Kashim, H. (2006). Primary alcoholic dementia and alcohol-related dementia. Psychogeriatrics, 6(3), 114-118. Retrieved from http://journals1.scholarsportal.info.subzero.lib.uoguelph.ca/tmp/6146926294860324774.pdf
- ^ Xiong, G. L., & Daubert, G. P. (2009, November 23). Wernicke-Korsakoff Syndrome. Retrieved March 11, 2010, from E-Medicine: http://emedicine.medscape.com/article/288379-overview
- ^ France, L. (2005). The Death of yesterday. The Observer, Retrieved from http://www.guardian.co.uk/books/2005/jan/23/biography.features3
- ^ Becker, A.L. (2009). Researchers to study pieces of unique brain. Hartford Courant, Retrieved from http://www.courant.com/health/hc-hm-brain-internet-1129.artnov29,0,976422,full.story
- ^ ^ Carey, Benedict (2010-03-06). "H. M., an Unforgettable Amnesiac, Dies at 82". The New York Times. http://www.nytimes.com/2008/12/05/us/05hm.html. Retrieved 2008-12-05.
- ^ a b Rodrigue, K.M., Kennedy, K.M., & Park D.C. (2009). Beta-Amyloid Deposition and the Aging Brain. Neuropsychological Review. Vol 19 (4) 436-450. Retrieved on March 6, 2010 from: http://www.springerlink.com/content/u31812104432q6g0/
- ^ a b Rapp, M.A. et al. (2009). Cortical neuritic plaques and hippocampal neurofibrillary tangles are related to dementia severity in elderly schizophrenia patients. Schizophrenia Research. 116, 90-96. Retrieved on March 6, 2010 from: http://journals1.scholarsportal.info.subzero.lib.uoguelph.ca/tmp/6246684683708035939.pdf
- ^ Bartus, R., Dean, R., Beer, B., & Lippa, A. (1982). The Cholinergic Hypothesis for Geriatric Memory Dysfunction. American Association for the Advancement of Science. Vol 212, 408-415. Retrieved from: http://www.sciencemag.org/cgi/content/abstract/sci;217/4558/408
- ^ [1] TEDTalks. (2008, February). Gregory Petsko on the coming neurological epidemic. Retrieved Mar 5, 2010, from TedTalks.com.
- ^ Corrigan, P. (1998) The impact of stigma on severe mental illness. Cognitive and Behavioural Practice, 5, 201-222.
- ^ Olshanksy, S., Grobs, S. & Ekdahl, M. (1960) Survey of employment experience of patients discharged from three mental hospitals during the priod of 1951-1953. Mental Hygiene, 44, 510-521
- ^ Farina, A. & Felner, R. (1973) Employment interviewer reactions to former mental patients. Journal of Abnormal Psychology. 82, 268-272
- ^ Borderireri, J. & Drehmer, D. (1986) Hiring decisions for disabled workers: looking at the cause. Journal of Applied Social Psychology, 16, 197-208
- ^ Link, B. (1987) Understanding labelling effects in the area of mental disorders: an assessment of the effects of the expectations of rejection. American Sociological Review, 52, 96-112.
- ^ Page, S. (1977) Effects of the mental illness label in attempts to obtain accommodation. Canadian Journal of Behavioural Sciences, 9, 85-90.
- ^ Page, S. (1983) Psychiatric stigma: two studies of behaviour when the chips are down. Canadian Journal of Mental Health, 2, 13-19.
- ^ Page S. (1995) Effects of the mental illness label in 1993: acceptance and rejection in the community. Journal of Health and Social Policy, 7, 61-68.
- ^ Sosowsky, L. (1980) Explaining the increased arrest rate among mental patients: a cautionary note. American Journal of Psychiatry, 137, 1602-1604.
- ^ Steadman, H. (1981) Critically reassessing the accuracy of public perceptions of the dangerousness of the mentally ill. Journal of Health and Social Behaviour, 22, 310-316.
- ^ Svoboda, E. & Richards, B. (2009) Compensating for anterograde amnesia: A new training method that capitalizes on emerging smartphone technologies. Journal of the International Neuropsychological Society, 15, 629-638.
- ^ [2] Haaze, T. (2005) Early-Onset Dementia: The Needs of Younger People with Dementia in Ireland.
- ^ Korczyn, A. D., Stein-Shvachman, I., & Werner, P. (2009). Early onset dementia: clinical and social aspects. International Psychogeriatrics, 631-636.
- ^ a b Kuo, C.L. & Kavanagh, Kathryn. (1994) Chinese Perspectives on Culture and Mental Health. Issues in Mental Health Nursing, 15, 551-567.
- ^ Chen, P.W. (2010, January 21). Offering Care for the Caregiver. The New York Times. Retrieved (2010, January 27) from http://www.nytimes.com/2010/01/22/health/21chen.html
- ^ Papastavrou, E., Kalokerinou, A., Papacostas, S.S., Tsangari, H., & Sourtzi, P. (2007). Caring for a relative with dementia: family caregiver burden. Medline, 58(5), Retrieved from http://journals1.scholarsportal.info.subzero.lib.uoguelph.ca/tmp/7749540681872195918.pdf


