Trichomonas vaginalis
| Trichomonas vaginalis | |
|---|---|

| |
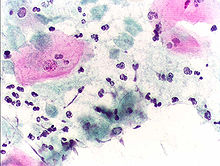
| Giemsa-stained culture of T. vaginalis | |
| Scientific classification | |
| Domain: | |
| (unranked): | |
| Phylum: | |
| Class: | |
| Order: | |
| Genus: | |
| Species: | T. vaginalis
|
| Binomial name | |
| Trichomonas vaginalis (Donné 1836)
| |
Trichomonas vaginalis, an anaerobic, parasitic flagellated protozoan, is the causative agent of trichomoniasis, and is the most common pathogenic protozoan infection of humans in industrialized countries.[1] The WHO has estimated that 180 million cases of infection are acquired annually worldwide. The estimates for North America alone are between 5 and 8 million new infections each year, with an estimated rate of asymptomatic cases as high as 50%.[2]
Protein function
T. vaginalis has many enzymes that catalyze many chemical reactions making the organism relevant to the study of protein function. T. vaginalis lacks mitochondria and other necessary enzymes and cytochromes to conduct oxidative phosphorylation. T. vaginalis obtains nutrients by transport through the cell membrane and by phagocytosis. The organism is able to maintain energy requirements by the use of a small amount of enzymes to provide energy via glycolysis of glucose to glycerol and succinate in the cytoplasm, followed by further conversion of pyruvate and malate to hydrogen and acetate in an organelle called the hydrogenosome.[3]
Morphology
The T. vaginalis trophozoite is oval as well as flagellated. Five flagella arise near the cytosome; four of these immediately extend outside the cell together, while the fifth flagellum wraps backwards along the surface of the organism. The functionality of the fifth flagellum is not known. In addition, a conspicuous barb-like axostyle projects opposite the four-flagella bundle; the axostyle may be used for attachment to surfaces and may also cause the tissue damage noted in trichomoniasis infections.[4]
While T. vaginalis does not have a cyst form, organisms can survive for up to 24 hours in urine, semen, or even water samples. Combined with an ability to persist on fomites with a moist surface for 1 to 2 hours, T. vaginalis is among the most durable protozoan trophozites.
Clinical
Trichomoniasis is a sexually transmitted disease which can occur in females (males rarely exhibit symptoms of a T. vaginalis infection) if the normal acidity of the vagina is shifted from a healthy, semi-acidic pH (3.8 - 4.2) to a much more basic one (5 - 6) that is conducive to T. vaginalis growth. Some of the symptoms of T. vaginalis include: preterm delivery, low birth weight, and increased mortality as well as predisposing to HIV infection, AIDS, and cervical cancer.[5] T. vaginalis has also been reported in the urinary tract, fallopian tubes, and pelvis and can cause pneumonia, bronchitis, and oral lesions. Other symptoms include inflammation with increasing number of organisms, greenish-yellow frothy vaginal secretions and itching. Condoms are effective at preventing infection.
Classically, with a pap smear, infected individuals have a transparent "halo" around their superficial cell nucleus. It is also is rarely detected by studying discharge or with a pap smear because of their low sensitivity. T. vaginalis was traditionally diagnosed via a wet mount, in which "corkscrew" motility was observed. Currently, the most common method of diagnosis is via overnight culture,[6][7] with a sensitivity range of 75-95%.[8] Newer methods, such as rapid antigen testing and transcription-mediated amplification, have even greater sensitivity, but are not in widespread use.[8] The presence of T. vaginalis can also be diagnosed by PCR, using the primers L23861 Fw and Rev.[9]
Infection is treated and cured with metronidazole or tinidazole, and should be prescribed to any sexual partner(s) as well because they may potentially be asymptomatic carriers.[10]
Genome Sequencing and Statistics
The T. vaginalis genome was found to be approximately 160 megabases in size[11] – ten times larger than predicted from earlier gel-based chromosome sizing [12] (The human genome is ~3.5 gigabases by comparison.[13]) As much as two-thirds of the T. vaginalis sequence consists of repetitive and transposable elements, reflecting a massive, evolutionarily-recent expansion of the genome. The total number of predicted protein-coding genes is ~98,000, which includes ~38,000 'repeat' genes (virus-like, transposon-like, retrotransposon-like, and unclassified repeats, all with high copy number and low polymorphism). Approximately 26,000 of the protein-coding genes have been classed as 'evidence-supported' (similar either to known proteins, or to ESTs), while the remainder have no known function. These extraordinary genome statistics are likely to change downward as the genome sequence, currently very fragmented due to the difficulty of ordering repetitive DNA, is assembled into chromosomes, and as more transcription data (ESTs, microarrays) accumulate. But it appears that the gene number of the single-celled parasite T. vaginalis is, at minimum, on par with that of its host H. sapiens.
In late 2007 TrichDB.org was launched as a free, public genomic data repository and retrieval service devoted to genome-scale trichomonad data. The site currently contains all of the T. vaginalis sequence project data, several EST libraries, and tools for data mining and display. TrichDB is part of the NIH/NIAID-funded EupathDB functional genomics database project.[14]
References
- ^ Soper D (2004). "Trichomoniasis: under control or undercontrolled?". American journal of obstetrics and gynecology. 190 (1): 281–90. doi:10.1016/j.ajog.2003.08.023. PMID 14749674.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Hook EW (1999). "Trichomonas vaginalis--no longer a minor STD". Sexually transmitted diseases. 26 (7): 388–9. PMID 10458631.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Upcroft P, Upcroft JA (2001). "Drug targets and mechanisms of resistance in the anaerobic protozoa". Clinical microbiology reviews. 14 (1): 150–64. doi:10.1128/CMR.14.1.150-164.2001. PMC 88967. PMID 11148007.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed. ed.). McGraw Hill. ISBN 0838585299.
{{cite book}}:|author=has generic name (help);|edition=has extra text (help) - ^ Schwebke JR, Burgess D (2004). "Trichomoniasis". Clinical microbiology reviews. 17 (4): 794–803, table of contents. doi:10.1128/CMR.17.4.794-803.2004. PMC 523559. PMID 15489349.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Ohlemeyer CL, Hornberger LL, Lynch DA, Swierkosz EM (1998). "Diagnosis of Trichomonas vaginalis in adolescent females: InPouch TV culture versus wet-mount microscopy". The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 22 (3): 205–8. PMID 9502007.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Sood S; et al. (2007). "InPouch TV culture for detection of Trichomonas vaginalis". Indian J Med Res. 125: 567–571. PMID 17598943.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ a b Huppert JS (Jul 15). "Rapid antigen testing compares favorably with transcription-mediated amplification assay for the detection of Trichomonas vaginalis in young women". Clinical Infectious Diseases. 45 (2): 194–198. doi:10.1086/518851. PMID 17578778.
{{cite journal}}: Check date values in:|date=and|year=/|date=mismatch (help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Schirm J, Bos PA, Roozeboom-Roelfsema IK, Luijt DS, Möller LV (2007). "Trichomonas vaginalis detection using real-time TaqMan PCR". Journal of microbiological methods. 68 (2): 243–7. doi:10.1016/j.mimet.2006.08.002. PMID 17005275.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Cudmore SL, Delgaty KL, Hayward-McClelland SF, Petrin DP, Garber GE (2004). "Treatment of infections caused by metronidazole-resistant Trichomonas vaginalis". Clinical microbiology reviews. 17 (4): 783–93, table of contents. doi:10.1128/CMR.17.4.783-793.2004. PMC 523556. PMID 15489348.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Carlton JM, Hirt RP, Silva JC; et al. (2007). "Draft genome sequence of the sexually transmitted pathogen Trichomonas vaginalis". Science (New York, N.Y.). 315 (5809): 207–12. doi:10.1126/science.1132894. PMC 2080659. PMID 17218520.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Lehker MW, Alderete JF (1999). "Resolution of six chromosomes of Trichomonas vaginalis and conservation of size and number among isolates". Journal of Parasitology. 85 (5): 976–979. PMID 10577741.
- ^ Zimmer, C. (2007). "Jurassic Genome". Science. 315: 1358–1359. doi:10.1126/science.315.5817.1358. PMID 17347424.
- ^ Aurrecoechea C, Brestelli J, Brunk BP; et al. (2008). "GiardiaDB and TrichDB: integrated genomic resources for the eukaryotic protist pathogens Giardia lamblia and Trichomonas vaginalis". Nucleic Acids Research. PMID 18824479.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link)
External links
- TIGR's Trichomonas vaginalis genome sequencing project.
- TrichDB: the Trichomonas vaginalis genome sequencing project
- NIH site on trichomoniasis.
- Taxonomy
- STI: What's trichomonas a website for teenagers
