Gulf War syndrome
| Gulf War syndrome |
|---|
Gulf War syndrome (GWS) or Gulf War illness (GWI) is a chronic multisymptom disorder affecting veterans and civilians after the 1991 Gulf War.[1][2][3] A wide range of acute and chronic symptoms have included fatigue, musculoskeletal pain, cognitive problems, skin rashes and diarrhea.[4] Approximately 250,000[5] of the 697,000 veterans who served in the 1991 Gulf War are afflicted with enduring chronic multi-symptom illness, a condition with serious consequences.[6] From 1995 to 2005, the health of combat veterans worsened in comparison with nondeployed veterans, with the onset of more new chronic diseases, functional impairment, repeated clinic visits and hospitalizations, chronic fatigue syndrome-like illness, posttraumatic stress disorder, and greater persistence of adverse health incidents.[7]
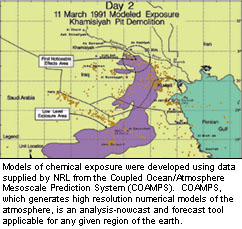
Those who were near conflicts during or downwind of chemical weapons depot demolition, had exposure to toxic chemicals which are currently believed to be the cause of the illness. Several specific causes have been investigated, including pyridostigmine bromide (PB) nerve gas antidote (NAPP) pills, organophosphate military strength pesticides, chemical weapons, and depleted uranium. Causes which have been ruled out include post traumatic stress disorder, anthrax vaccinations,[6] and smoke from oil well fires, though these exposures may have led to various illnesses and symptoms in a limited number of Gulf War veterans. PB or NAPP antidote pills given to protect troops from nerve agents and military strength insecticides used during deployment have currently been most closely linked to Gulf War veterans' chronic multi-symptom illness. Exposure to the destruction of the Khamisiyah weapons depot, where large quantities of Iraqi chemical munitions containing sarin and cyclosarin nerve agents was stored, is negatively correlated with motor speed.[8] Exposure to depleted uranium is unlikely to be a primary cause of Gulf War Illness.[6]
Methods of preventing or treating Gulf War syndrome vary. While the treatment of sarin exposure has been studied,[9] other acetylcholinesterase inhibitors such as pyridostigmine bromide and organophosphate insecticides may or may not involve similar management.
Classification
Medical ailments associated with Gulf War Syndrome have been recognized by both the Department of Defense and the Department of Veterans Affairs.[1] Since so little concrete information was known about this condition the Veterans administrations originally classified individuals with related ailments believed to be connected to their service in the Persian Gulf a special non-ICD-9 code DX111, as well as ICD-9 code V65.5.[10]
Signs and symptoms

According to an April 2010 U.S. Department of Veterans Affairs (VA) sponsored study conducted by the Institute of Medicine (IOM), part of the U.S. National Academy of Sciences, 250,000[5] of the 696,842 U.S. servicemen and women in the 1991 Gulf War continue to suffer from chronic multi-symptom illness, popularly known as "Gulf War Illness" or "Gulf War Syndrome." The IOM found that the chronic multi-symptom illness continues to affect these veterans nearly 20 years after the war, and, "the excess of unexplained medical symptoms reported by deployed [1991] Gulf war veterans cannot be reliably ascribed to any known psychiatric disorder."[11]
According to the IOM, "It is clear that a significant portion of the soldiers deployed to the Gulf War have experienced troubling constellations of symptoms that are difficult to categorize," said committee chair Stephen L. Hauser, professor and chair, department of neurology, University of California, San Francisco (UCSF). "Unfortunately, symptoms that cannot be easily quantified are sometimes incorrectly dismissed as insignificant and receive inadequate attention and funding by the medical and scientific establishment. Veterans who continue to suffer from these symptoms deserve the very best that modern science and medicine can offer to speed the development of effective treatments, cures, and—we hope—prevention. Our report suggests a path forward to accomplish this goal, and we believe that through a concerted national effort and rigorous scientific input, answers can be found."[5]
With the issuance of this report, the IOM pointed the way forward. There is a pressing need to answer lingering questions, such as why some veterans suffer a range of symptoms whereas others experience specific, isolated health problems or no ill health, and why some veterans who were not on the ground during the conflict or who arrived after combat ended have multisymptom illness, while others who served on the ground during the height of the battle have experienced few or no symptoms. The dearth of data on veterans' pre-deployment and immediate post-deployment health status and lack of measurement and monitoring of the various substances to which veterans may have been exposed make it difficult—and in many cases impossible—to reconstruct what happened to service members during their deployments nearly 20 years after the fact, the committee noted.[5]
The report calls for a substantial commitment to improve identification and treatment of multisymptom illness in Gulf War veterans. The path forward should include continued monitoring of Gulf War veterans and development of better medical care for those with persistent, unexplained symptoms. Researchers should undertake studies comparing genetic variations and other differences in veterans experiencing multisymptom illness and asymptomatic veterans. It is likely that multisymptom illness results from the interactions between environmental exposures and genes, and genetics may predispose some individuals to illness, the committee noted. There are sufficient numbers of veterans to conduct meaningful comparisons given that nearly 700,000 U.S. personnel were deployed to the region and more than 250,000 of them suffer from persistent, unexplained symptoms. A consortium involving the U.S. Department of Veterans Affairs, U.S. Department of Defense, and National Institutes of Health could coordinate this effort and contribute the necessary resources.[5]
The IOM also found that service in the 1991 Gulf War is a cause of post-traumatic stress disorder (PTSD) in some veterans and is also associated with gastrointestinal disorders such as irritable bowel syndrome; substance abuse, particularly alcoholism; and psychiatric problems such as anxiety disorder. And, IOM's report shows there is some evidence that service during the 1991 Gulf War is linked to fibromyalgia and chronic widespread pain, amyotrophic lateral sclerosis (ALS, also known as Lou Gehrig's disease), sexual difficulties, and death due to causes such as car accidents in the early years after deployment, but the data are limited, said the committee that wrote the report.[5]
Older research shows that the U.S. and the UK, with the highest rates of excess illness, are distinguished from the other nations by higher rates of pesticide use, use of anthrax vaccine, and somewhat higher rates of exposures to oil fire smoke and reported chemical alerts. France, with possibly the lowest illness rates, had lower rates of pesticide use, and no use of anthrax vaccine.[12] French troops also served to the North and West of all other combat troops, away and upwind of major combat engagements.[13]
| Symptom | U.S. | UK | Australia | Denmark |
|---|---|---|---|---|
| Fatigue | 23% | 23% | 10% | 16% |
| Headache | 17% | 18% | 7% | 13% |
| Memory problems | 32% | 28% | 12% | 23% |
| Muscle/joint pain | 18% | 17% | 5% | 2% (<2%) |
| Diarrhea | 16% | 9% | 13% | |
| Dyspepsia/indigestion | 12% | 5% | 9% | |
| Neurological problems | 16% | 8% | 12% | |
| Terminal tumors | 33% | 9% | 11% |
| Condition | U.S. | UK | Canada | Australia |
|---|---|---|---|---|
| Skin conditions | 20–21% | 21% | 4–7% | 4% |
| Arthritis/joint problems | 6–11% | 10% | (-1)–3% | 2% |
| Gastro-intestinal (GI) problems | 15% | 5–7% | 1% | |
| Respiratory problem | 4–7% | 2% | 2–5% | 1% |
| Chronic fatigue syndrome | 1–4% | 3% | 0% | |
| Post-traumatic stress disorder | 2–6% | 9% | 6% | 3% |
| Chronic multi-symptom illness | 13–25% | 26% |
Although Gulf War illness is the most prominent condition affecting Gulf War veterans, it is just one health issue to be addressed in the larger context of the health of Gulf War veterans. Other Gulf War-related health issues of importance include rates of diagnosable medical conditions and post-war mortality among Gulf War veterans, and questions related to the risk of birth defects and other health problems in veterans’ family members.
Results from two studies, using different methods in different groups of symptomatic veterans, indicate that Gulf War illness is associated with a low-level, persistent immune activation, reflected in elevated levels of the cytokines IL-2, IFN-γ and IL-10. In addition, several studies have reported that NK cell numbers and/or cytotoxic activity are significantly reduced in veterans with Gulf War illness.[16]
Birth defects
This section's factual accuracy is disputed. (May 2012) |
Two studies of Gulf war veterans found increases in self-reported birth defects of veterans's children, though this association was weakened when the analysis was restricted to confirmed conditions, and the authors expressed a concern over recall bias.[17] There were no increases in birth defects found in the children of Australian[18] or French troops.[19] A 2006 review of studies of international coalition troops' children concluded there was no consistent evidence linking Gulf War deployment to major birth defects conceived after the war, despite a variety of methodologies and data sources being used. Despite this, the ability to detect increases in rare birth defects, defects in the children of female veterans, or the problems created by relying on self-reporting meant there were still "notable limitations" on the studies conclusions.[20]
A 2008 report published by the United States Veteran's Affairs Administration on GWS concluded that though there were suggestions of increased birth defects in veterans, the ability to link service to specific birth defects was limited and "overall rates are still within the normal range found in the general population".[6]
Causes
The United States Congress mandated the National Academies of Science Institute of Medicine to provide nine reports on Gulf War Syndrome since 1998.[21] Aside from the many physical and psychological issues involving any war zone deployment, Gulf War veterans were exposed to a unique mix of hazards not previously experienced during wartime. These included pyridostigmine bromide pills given to protect troops from the effects of nerve agents, depleted uranium munitions, and anthrax and botulinum vaccines. The oil and smoke that spewed for months from hundreds of burning oil wells presented another exposure hazard not previously encountered in a warzone. Military personnel also had to cope with swarms of insects, requiring the widespread use of pesticides.
United States Veterans Affairs Secretary Anthony Principi's panel found that pre-2005 studies suggested the veterans' illnesses are neurological and apparently are linked to exposure to neurotoxins, such as the nerve gas sarin, the anti-nerve gas drug pyridostigmine bromide, and pesticides that affect the nervous system. The review committee concluded that "Research studies conducted since the war have consistently indicated that psychiatric illness, combat experience or other deployment-related stressors do not explain Gulf War veterans illnesses in the large majority of ill veterans," the review committee said.[22]
Pyridostigmine bromide nerve gas antidote
The US military issued pyridostigmine bromide (PB) pills to protect against exposure to nerve gas agents such as sarin and soman. PB was used to pretreat nerve agent poisoning; it is not a vaccine however. Taken before exposure to nerve agents, PB was thought to increase the efficacy of nerve agent antidotes. PB had been used since 1955 for patients suffering from myasthenia gravis with doses up to 1,500 mg a day, far in excess of the 90 mg given to soldiers, and was considered safe by the FDA at either level for indefinite use and its use to pretreat nerve agent exposure had recently been approved.[23]
About half of U.S. Gulf War veterans report using PB during deployment, with greatest use among Army personnel. Concerns have been raised about the possibility of increased health problems from PB when it is combined with other risk factors.[citation needed]
Given both the large body of epidemiological data on myasthenia gravis patients and follow up studies done on veterans it was concluded that while it was unlikely that health effects reported today by Gulf War veterans are the result of exposure solely to PB, use of PB was causally associated with illness.[6]
Organophosphate pesticides
The use of organophosphate pesticides and insect repellants during the first Gulf War is credited with keeping rates of pest-borne diseases low. Pesticide use is one of only two exposures consistently identified by Gulf War epidemiologic studies to be significantly associated with Gulf War illness.[24] Multisymptom illness profiles similar to Gulf War illness have been associated with low-level pesticide exposures in other human populations. In addition, Gulf War studies have identified dose-response effects, indicating that greater pesticide use is more strongly associated with Gulf War illness than more limited use.[25] Pesticide use during the Gulf War has also been associated with neurocognitive deficits and neuroendocrine alterations in Gulf War veterans in clinical studies conducted following the end of the war. The 2008 report concluded that “all available sources of evidence combine to support a consistent and compelling case that pesticide use during the Gulf War is causally associated with Gulf War illness.”[6]
Sarin nerve agent
Many of the symptoms of Gulf War syndrome are similar to the symptoms of organophosphate, mustard gas, and nerve gas poisoning.[26][27] Gulf War veterans were exposed to a number of sources of these compounds, including nerve gas and pesticides.[28]
Chemical detection units from the Czech Republic, France, and Britain confirmed chemical agents. French detection units detected chemical agents. Both Czech and French forces reported detections immediately to U.S. forces. U.S. forces detected, confirmed, and reported chemical agents; and U.S. soldiers were awarded medals for detecting chemical agents. The Riegle Report said that chemical alarms went off 18,000 times during the Gulf War. After the air war started on January 16, 1991, coalition forces were chronically exposed to low but nonlethal levels of chemical and biological agents released primarily by direct Iraqi attack via missiles, rockets, artillery, or aircraft munitions and by fallout from allied bombings of Iraqi chemical warfare munitions facilities.[29]
In 1997, the US Government released an unclassified report that stated, "The US Intelligence Community (IC) has assessed that Iraq did not use chemical weapons during the Gulf War. However, based on a comprehensive review of intelligence information and relevant information made available by the United Nations Special Commission (UNSCOM), we conclude that chemical warfare (CW) agent was released as a result of US postwar demolition of rockets with chemical warheads at several sites including Khamisiyah". Over 125,000 U.S. troops and 9,000 UK troops were exposed to nerve gas and mustard gas when the Iraqi depot in Khamisiyah was destroyed.[30]
Recent studies have confirmed earlier suspicions that exposure to sarin, in combination with other contaminants such as pesticides and PB were related to reports of veteran illness. Estimates range from 100,000 to 300,000 individuals exposed to nerve agents[31]
Depleted uranium
Depleted uranium (DU) was widely used in tank kinetic energy penetrator and autocannon rounds for the first time in the Gulf War. DU is a dense, weakly radioactive metal. Munitions made from it often burn when they impact a hard target, producing toxic combustion products. Roughly 320 tons of DU were used during the February, 1991 conflict.[32] After military personnel began reporting unexplained health problems in the aftermath of the Gulf War, questions were raised about the health effect of exposure to depleted uranium.
The use of DU in munitions is controversial because of questions about potential long-term health effects.[33] Normal functioning of the kidney, brain, liver, heart, and numerous other systems can be affected by uranium exposure, because in addition to being weakly radioactive, uranium is a toxic metal.[34]
Early studies of depleted uranium aerosol exposure assumed that uranium combustion product particles would quickly settle out of the air[35] and thus could not affect populations more than a few kilometers from target areas,[36] and that such particles, if inhaled, would remain undissolved in the lung for a great length of time and thus could be detected in urine.[37] Uranyl ion contamination has been found on and around depleted uranium targets.[38]
In the Balkans war zone where depleted uranium was also used, an absence of problems is seen by some as evidence of DU munitions' safety. "Independent investigations by the World Health Organization, European Commission, European Parliament, United Nations Environment Programme, United Kingdom Royal Society, and the Health Council of the Netherlands all discounted any association between depleted uranium and leukemia or other medical problems."[32] In Italy, controversy over the health risks associated with the use of DU continues, with a Senate investigation committee was due to release its report into 'Balkan Syndrome' by the end of 2007.[39] Since then, there has been a resurgence of interest in the health effects of depleted uranium, especially since it has recently been linked with neurotoxicity.[40]
The aerosol produced during impact and combustion of depleted uranium munitions can potentially contaminate wide areas around the impact sites or can be inhaled by civilians and military personnel.[41] A 2008 review by the U.S. Department of Veterans Affairs found that while low-level exposure to DU was widespread during the Gulf War, the persistent effects of low-dose exposures have only been minimally assessed. They found no association between DU exposure and multisymptom illness, concluding that "exposure to DU munitions is not likely a primary cause of Gulf War illness". However questions remain about the long-term effects of higher-dose exposure to DU.[6]

Ruled out
Several potential causes beyond vaccinations, stress, and oil well fires—explained in more detail below—have been ruled out. Other ruled-out potential causes include Scud missile fuel and infectious diseases. Limited evidence from several sources suggests that an association with the combined effects of multiple neurotoxicant exposures and receipt of multiple vaccines can not be ruled out.[42][full citation needed]
Anthrax vaccine
Iraq had loaded anthrax, botulinum toxin, and aflatoxin into missiles and artillery shells in preparing for the Gulf War and that[clarification needed][vague] these munitions were deployed to four locations in Iraq.[43] During Operation Desert Storm, 41% of U.S. combat soldiers and 75% of UK combat soldiers were vaccinated against anthrax.[44] Reactions included local skin irritation, some lasting for weeks or months.[45] While the Food and Drug Administration (FDA) approved the vaccine, it never went through large scale clinical trials, unlike most other vaccines in the United States.[46] While recent studies have demonstrated the vaccine’s is highly reactogenic,[47] there is no clear evidence or epidemiological studies on Gulf War veterans linking the vaccine to Gulf War Syndrome. Combining this with the lack of symptoms from current deployments of individuals who have received the vaccine led the Committee on Gulf War Veterans’ Illnesses to conclude that the vaccine is not a likely cause of Gulf War illness for most ill veterans.[6]
Combat stress
Research studies conducted since the war have consistently indicated that psychiatric illness, combat experience or other deployment-related stressors do not explain Gulf War veterans illnesses in the large majority of ill veterans, according to a U.S. Department of Veterans Affairs (VA) review committee.
An April 2010 Institute of Medicine review found, "the excess of unexplained medical symptoms reported by deployed [1991] Gulf war veterans cannot be reliably ascribed to any known psychiatric disorder."[11]
Oil well fires
During the war, many oil wells were set on fire in Kuwait by the retreating Iraqi army, and the smoke from those fires was inhaled by large numbers of soldiers, many of whom suffered acute pulmonary and other chronic effects, including asthma and bronchitis. However, firefighters who were assigned to the oil well fires and encountered the smoke, but who did not take part in combat, have not had GWI symptoms.[48]
Diagnosis
This section needs expansion. You can help by adding to it. (January 2010) |
Multisymptom illness is more prevalent in Gulf War I veterans than veterans of previous conflicts, but the pattern of comorbidities is similar for actively deployed and nondeployed military personnel.[49] Management of potentially comorbid toxic exposures requires awareness of the toxins involved.[9] Exposure to the destruction of the Khamisiyah weapons depot, where large quantities of the chemical weapon sarin was stored, is negatively correlated with motor speed.[8] Epidemiological evidence is consistent with increased risk of birth defects in the offspring of persons exposed to depleted uranium.[50]
Management
Nerve agent antidote and insect repellent
In 2008, a paper published in the Proceedings of the National Academy of Sciences suggested that excess illnesses in Gulf War veterans could be explained in part by their exposure to organophosphate and carbamate acetylcholinesterase inhibitors.[31] A federal report released in November, 2008, agreed, stating that exposure to two substances "are causally associated with Gulf War illness":[51]
- pyridostigmine bromide, an acetylcholinesterase inhibitor intended to protect against nerve agents,[52] and
- pesticides and insect repellents (often acetylcholinesterase inhibitors)
This section needs expansion. You can help by adding to it. (December 2009) |
Sarin
Exposure to sarin, a nerve gas, is a possible comorbidity. Chemical weapons classified as nerve agents are also strong acetylcholinesterase inhibitors. A 2004 review discusses symptoms, signs, and treatment of nerve agent exposure.[9]
Epidemiologic research
Epidemiologic studies have been performed evaluating many suspected etiologic factors for Gulf War illness as seen in veteran populations. Below is a summary of epidemiologic studies of veterans displaying multisymptom illness and their exposure to suspect conditions from the 2008 U.S. Veterans Administration report.[53]
A fuller understanding of immune function in ill Gulf War veterans is needed, particularly in veteran subgroups with different clinical characteristics and exposure histories. It is also important to determine the extent to which identified immune perturbations may be associated with altered neurological and endocrine processes that are associated with immune regulation.[16] No study that have evaluated birth outcomes and birth defects among Gulf War veterans and their children has assessed whether there is any connection between reproductive outcomes and uranium exposure in the Gulf War.[54] Very limited cancer data have been reported for U.S. Gulf War veterans in general, and no published research on cases occurring after 1999. Because of the extended latency periods associated with most cancers, it is important that cancer information be brought up to date and that cancer rates be assessed in Gulf War veterans on an ongoing basis. In addition, cancer rates should be evaluated in relation to identifiable exposure and location subgroups.[55]
| Epidemiologic Studies of Gulf War Veterans: Association of Deployment Exposures With Multisymptom Illness[56] | |||||||
|---|---|---|---|---|---|---|---|
| Preliminary Analysis (no controls for exposure) | Adjusted Analysis (controlling for effects of exposure) | Clinical Evaluations | |||||
| GWV population in which association was assessed | GWV population in which association was statistically significant | GWV population in which association was assessed | GWV population in which association was statistically significant | Dose response effect identified? | |||
| Pyridostigmine bromide | 10 | 9 | 6 | 6 | ✓ | Associated with neurocognitive and HPA differences in GW vets | |
| Pesticides | 10 | 10 | 6 | 5 | ✓ | Associated with neurocognitive and HPA differences in GW vets | |
| Physiological Stressors | 14 | 13 | 7 | 1 | |||
| Chemical Weapons | 16 | 13 | 5 | 3 | Associated with neurocognitive and HPA differences in GW vets | ||
| Oil Well Fires | 9 | 8 | 4 | 2 | ✓ | ||
| Number of Vaccines | 2 | 2 | 1 | 1 | ✓ | ||
| Anthrax Vaccine | 5 | 5 | 2 | 1 | |||
| Tent Heater Exhaust | 5 | 4 | 2 | 1 | |||
| Sand/Particulates | 3 | 3 | 3 | 1 | |||
| Depleted Uranium | 5 | 3 | 1 | 0 | |||
Controversy
Similar syndromes have been seen as an after effect of other conflicts — for example, 'shell shock' after World War I, and post-traumatic stress disorder (PTSD) after the Vietnam War. A review of the medical records of 15,000 American Civil War soldiers showed that "those who lost at least 5% of their company had a 51% increased risk of later development of cardiac, gastrointestinal, or nervous disease."[57]
A November 1996 article in the New England Journal of Medicine found no difference in death rates, hospitalization rates or self-reported symptoms between Persian Gulf veterans and non-Persian Gulf veterans. This article was a compilation of dozens of individual studies involving tens of thousands of veterans. The study did find a statistically significant elevation in the number of traffic accidents suffered by Gulf War veterans.[58] An April, 1998 article in Emerging Infectious Diseases similarly found no increased rate of hospitalization and better health overall for veterans of the Persian Gulf War vs. Veterans who stayed home.[59]
Despite these studies, on November 17, 2008 a congressionally appointed committee called the Research Advisory Committee on Gulf War Veterans' Illnesses, staffed with independent scientists and veterans appointed by the Department of Veterans Affairs, announced that the syndrome is a distinct physical condition. The committee recommended that Congress increase funding for research on Gulf War veterans' health to at least $60 million per year.[51] In January 2006, a study led by Melvin Blanchard and published by the Journal of Epidemiology, part of the "National Health Survey of Gulf War-Era Veterans and Their Families", stated that veterans deployed in the Persian Gulf War had nearly twice the prevalence of chronic multisymptom illness, a cluster of symptoms similar to a set of conditions often called Gulf War Syndrome.[60]
See also
References
- ^ a b "Gulf War Veterans' Illnesses: Illnesses Associated with Gulf War Service". United States Department of Veterans Affairs. nd. Retrieved 2012-05-09.
- ^ Iversen A, Chalder T, Wessely S (2007). "Gulf War Illness: lessons from medically unexplained symptoms". Clin Psychol Rev. 27 (7): 842–54. doi:10.1016/j.cpr.2007.07.006. PMID 17707114.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gronseth GS (2005). "Gulf war syndrome: a toxic exposure? A systematic review". Neurol Clin. 23 (2): 523–40. doi:10.1016/j.ncl.2004.12.011. PMID 15757795.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ "Gulf War Syndrome". University of Virginia. Archived from the original on 2008-10-11.
- ^ a b c d e f Stencel, C (2010-04-09). "Gulf War Service Linked to Post-Traumatic Stress Disorder, Multisymptom Illness, Other Health Problems, But Causes Are Unclear". National Academy of Sciences. Retrieved 2012-05-09.
- ^ a b c d e f g h Research Advisory Committee on Gulf War Veterans’ Illnesses (2008-11-01). "Gulf War Illness and the Health of Gulf War Veterans: Scientific Findings and Recommendations" (pdf). U.S. Department of Veterans Affairs. Retrieved 2012-05-09.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21795757, please use {{cite journal}} with
|pmid= 21795757instead. - ^ a b Toomey, R; Alpern, R; Vasterling, JJ; Baker, DG; Reda, DJ; Lyons, MJ; Henderson, WG; Kang, HK; Eisen, SA (2009). "Neuropsychological functioning of U.S. Gulf War veterans 10 years after the war". Journal of the International Neuropsychological Society: JINS. 15 (5): 717–29. doi:10.1017/S1355617709990294. PMID 19640317.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ a b c Schecter, WP (2004). "Cholinergic symptoms due to nerve agent attack: a strategy for management". Anesthesiol Clin North America. 22 (3): 579–90. doi:10.1016/j.atc.2004.04.005. PMID 15325720.
- ^ Department of Veterans Affairs Veterans Health Initiative (2002). "A Guide to Gulf War Veterans' Health" (PDF). Archived from the original (PDF) on 2006-09-26.
- ^ a b Committee on Gulf War and Health: Health Effects of Serving in the Gulf War. Gulf War and Health, Volume 8 - Update of Health Effects of Serving in the Gulf War. National Academies Press. pp. 109.
- ^ RAC-GWVI Minutes 2005, p. 78
- ^ RAC-GWVI Minutes 2005, p. 68
- ^ RAC-GWVI Minutes 2005, p. 70, This table applies only to coalition forces involved in combat.
- ^ RAC-GWVI Minutes 2005, p. 71
- ^ a b RAC-GWVI Report 2008, p. 262 (PDF p. 270)
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15075150, please use {{cite journal}} with
|pmid= 15075150instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17504542, please use {{cite journal}} with
|pmid=17504542instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18442369, please use {{cite journal}} with
|pmid=18442369instead. - ^ Cite error: The named reference
DoyleReviewwas invoked but never defined (see the help page). - ^ VA Press Release
- ^ Research Advisory Committee on Gulf War Veterans’ Illnesses (2004-09-01). "Research Advisory Committee on Gulf War Veterans' Illnesses 2004 Report" (pdf). United States Department of Veterans Affairs. Retrieved 2012-05-09.
{{cite web}}: Text "Scientific Progress in Understanding Gulf War Veterans’ Illnesses: Report and Recommendations" ignored (help) - ^ "Pyridostigmine bromide use in the First Gulf War". PBS Frontline. 1996-12-01. Retrieved 2012-05-09.
- ^ Office of the Special Assistant to the Undersecretary of Defense (Personnel and Readiness) for Gulf War Illnesses Medical Readiness and Military Deployments (2003-04-17). Environmental Exposure Report: Pesticides Final Report. Washington, D.C.: United States Department of Defense.
- ^ Krengel, M (2008-08-01). Neuropsychological Functioning in Gulf War Veterans Exposed to Pesticides and Pyridostigmine Bromide. Fort Detrick, MD: U.S. Army Medical Research and Materiel Command. Retrieved 2012-05-09.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) W81XWH-04-1-0118 - ^ Friis, Robert H. (2004). Epidemiology for Public Health Practice. Jones & Bartlett Publishers. ISBN 0-7637-3170-6.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Spektor, Dalia M. (1998). A Review of the Scientific Literature as it Pertains to Gulf War Illnesses. RAND Corporation. ISBN 0-8330-2680-1.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Campaigners hail 'nerve gas link' to Gulf War Syndrome". Edinburgh: News.scotsman.com. November 13, 2004. Retrieved November 24, 2009.
- ^ Riegle, DW (1994-02-09), U.S. Chemical and Biological Warfare-Related Dual Use Exports to Iraq and their Possible Impact on the Health Consequences of the Gulf War, Wikisource, retrieved 2012-05-09
- ^ Persian Gulf War Illnesses Task Force (1997-04-09). "Khamisiyah: A Historical Perspective on Related Intelligence". Federation of American Scientists. Retrieved 2012-05-09.
- ^ a b Golomb BA (2008). "Acetylcholinesterase inhibitors and Gulf War illnesses". Proc. Natl. Acad. Sci. U.S.A. 105 (11): 4295–300. doi:10.1073/pnas.0711986105. PMC 2393741. PMID 18332428.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b "Depleted Uranium". GlobalSecurity.org. nd. Retrieved 2012-05-09.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17508699 , please use {{cite journal}} with
|pmid= 17508699instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15205046, please use {{cite journal}} with
|pmid= 15205046instead. - ^ "Depleted Uranium in the Gulf (II) TAB L - Research Report Summaries". Archived from the original on 10 January 2007.
- ^ Mitsakou C, Eleftheriadis K, Housiadas C, Lazaridis M (2003). "Modeling of the dispersion of depleted uranium aerosol". Health Phys. 84 (4): 538–44. doi:10.1097/00004032-200304000-00014. PMID 12705453.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Horan P, Dietz L, Durakovic A (2002). "The quantitative analysis of depleted uranium isotopes in British, Canadian, and U.S. Gulf War veterans". Mil Med. 167 (8): 620–7. PMID 12188230.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Salbu B, Janssens K, Lind O, Proost K, Gijsels L, Danesi P (2005). "Oxidation states of uranium in depleted uranium particles from Kuwait". J Environ Radioact. 78 (2): 125–35. doi:10.1016/j.jenvrad.2004.04.001. PMID 15511555.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Anes Alic (October 29, 2007). "Depleted uranium, depleted health concerns". ISN Security Watch.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16679544 , please use {{cite journal}} with
|pmid= 16679544instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 12705453, please use {{cite journal}} with
|pmid= 12705453instead. - ^ Veterans Administration (November, 2009) p. 11 (PDF page 21)
- ^ Cordesman, AH (1999). Iraq and the War of Sanctions: Conventional Threats and Weapons of Mass Destruction. Greenwood Publishing Group. ISBN 978-0-275-96528-0.
- ^ RAC-GWVI Minutes 2005, p. 73
- ^ Chan, KC (2000-10-11). "GAO-01-92T Anthrax Vaccine: Preliminary Results of GAO's Survey of Guard/Reserve Pilots and Aircrew Members" (pdf). Government Accountability Office. Retrieved 2012-05-09.
- ^ Burdeau, C (2001-05-16). "Expert: Anthrax vaccine not proven". The Clarion-Ledger.
- ^ McNeil MM, Chiang IS, Wheeling JT, Zhang Y (2007). "Short-term reactogenicity and gender effect of anthrax vaccine: analysis of a 1967–1972 study and review of the 1955–2005 medical literature". Pharmacoepidemiol Drug Saf. 16 (3): 259–74. doi:10.1002/pds.1359. PMID 17245803.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ RAC-GWVI Minutes 2005, pp. 148, 154, 156
- ^ Kelsall, H. L.; McKenzie, DP; Sim, MR; Leder, K; Forbes, AB; Dwyer, T (2009). "Physical, psychological, and functional comorbidities of multisymptom illness in Australian male veterans of the 1991 Gulf War". Am J Epidemiol. 170 (8): 1048–56. doi:10.1093/aje/kwp238. PMID 19762370.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16124873, please use {{cite journal}} with
|pmid= 16124873instead. - ^ a b Silverleib, A (2008-12-09). "Gulf War illness is real, new federal report says". CNN. Retrieved 2012-05-09.
- ^ RAC-GWVI Minutes 2005
- ^ RAC-GWVI Report 2008, pp. 220–1
- ^ RAC-GWVI Report 2008, p. 96 (PDF p. 105)
- ^ RAC-GWVI Report 2008, p. 45 (PDF p. 55)
- ^ RAC-GWVI Report 2008, p. 222
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1126/science.291.5505.812, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1126/science.291.5505.812instead. - ^ Campion EW (1996). "Disease and suspicion after the Persian Gulf War". N. Engl. J. Med. 335 (20): 1525–7. doi:10.1056/NEJM199611143352010. PMID 8890106.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Knoke JD, Gray GC (1998). "Hospitalizations for unexplained illnesses among U.S. veterans of the Persian Gulf War". Emerging Infect. Dis. 4 (2): 211–9. doi:10.3201/eid0402.980208. PMC 2640148. PMID 9621191.
- ^ Purdy, MC (2006-01-20). "Study finds multisymptom condition is more prevalent among Persian Gulf vets". Washington University in St. Louis. Retrieved 2012-05-09.
