Adrenal tumor
| Adrenal tumor | |
|---|---|
 | |
| Incidences and prognoses of adrenal tumors.[1] | |
| Specialty | Oncology |
An adrenal tumor or adrenal mass[2] is any benign or malignant neoplasms of the adrenal gland, several of which are notable for their tendency to overproduce endocrine hormones. Adrenal cancer is the presence of malignant adrenal tumors, and includes neuroblastoma, adrenocortical carcinoma and some adrenal pheochromocytomas. Most adrenal pheochromocytomas and all adrenocortical adenomas are benign tumors, which do not metastasize or invade nearby tissues, but may cause significant health problems by unbalancing hormones.
Metastasis to the adrenals
[edit]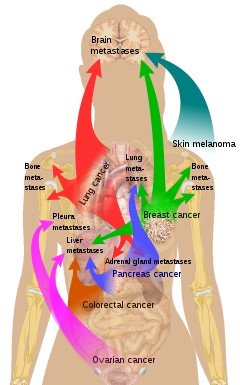
Metastasis to one or both adrenal glands is the most common form of malignant adrenal lesion, and the second most common adrenal tumor after benign adenomas.[4] Primary tumors in such cases are most commonly from lung cancer (39%), breast cancer (35%), malignant melanoma, gastrointestinal tract cancer, pancreas cancer, and renal cancer.[4]
Tumors of the adrenal cortex
[edit]The adrenal cortex is composed of three distinct layers of endocrine cells which produce critical steroid hormones. These include the glucocorticoids, which are critical for regulation of blood sugar and the immune system, as well as response to physiological stress; the mineralcorticoid aldosterone, which regulates blood pressure and kidney function; and certain sex hormones. Both benign and malignant tumors of the adrenal cortex may produce steroid hormones, with important clinical consequences.[citation needed]
Adrenocortical adenoma
[edit]Adrenocortical adenomas are benign tumors of the adrenal cortex that are extremely common (present in 1-10% of persons at autopsy). They should not be confused with adrenocortical "nodules", which are not true neoplasms. Adrenocortical adenomas are uncommon in patients younger than 30 years old, and have equal incidence in both sexes.[citation needed] The clinical significance of these neoplasms is twofold. First, they have been detected as incidental findings with increasing frequency in recent years, due to the increasing use of CT scans and magnetic resonance imaging in a variety of medical settings. This can result in expensive additional testing and invasive procedures to rule out the slight possibility of an early adrenocortical carcinoma. Second, a minority (about 15%) of adrenocortical adenomas are "functional", meaning that they produce glucocorticoids, mineralcorticoids, and/or sex steroids, resulting in endocrine disorders such as Cushing's syndrome, Conn's syndrome (hyperaldosteronism), virilization of females, or feminization of males. Functional adrenocortical adenomas are surgically curable.[citation needed]
Most of the adrenocortical adenomas are less than 2 cm in greatest dimension and less than 50 gram in weight. However, size and weight of the adrenal cortical tumors are no longer considered to be a reliable sign of benignity or malignancy. Grossly, adrenocortical adenomas are encapsulated, well-circumscribed, solitary tumors with solid, homogeneous yellow-cut surface. Necrosis and hemorrhage are rare findings.[citation needed]
Adrenocortical carcinoma
[edit]Adrenocortical carcinoma (ACC) is a rare, highly aggressive cancer of adrenal cortical cells, which may occur in children or adults. ACCs may be "functional", producing steroid hormones and consequent endocrine dysfunction similar to that seen in many adrenocortical adenomas, but many are not. Due to their location deep in the retroperitoneum, most adrenocortical carcinomas are not diagnosed until they have grown quite large. They frequently invade large vessels, such as the renal vein and inferior vena cava, as well as metastasizing via the lymphatics and through the blood to the lungs and other organs. The most effective treatment is surgery, although this is not feasible for many patients, and the overall prognosis of the disease is poor. Chemotherapy, radiation therapy, and hormonal therapy may also be employed in the treatment of this disease.[citation needed]
Tumors of the adrenal medulla
[edit]The adrenal medulla is located anatomically at the center of each adrenal gland, and is composed of neuroendocrine (chromaffin) cells which produce and release epinephrine (adrenaline) into the bloodstream in response to activation of the sympathetic nervous system. Neuroblastoma and pheochromocytoma are the two most important tumors which arise from the adrenal medulla. Both tumors may also arise from extra-adrenal sites, specifically, in the paraganglia of the sympathetic chain.[citation needed]
Neuroblastoma
[edit]Neuroblastoma is an aggressive cancer of immature neuroblastic cells (precursors of neurons), and is one of the most common pediatric cancers, with a median age at diagnosis of two years.[5] Adrenal neuroblastoma typically presents with a rapidly enlarging abdominal mass. Although the tumor has often spread to distant parts of the body at the time of diagnosis, this cancer is unusual in that many cases are highly curable when the spread is limited to the liver, skin, and/or bone marrow (stage IVS). Related, but less aggressive tumors composed of more mature neural cells include ganglioneuroblastoma and ganglioneuroma. Neuroblastic tumors often produce elevated levels of catecholamine hormone metabolites, such as vanillylmandelic acid (VMA) and homovanillic acid, and may produce severe watery diarrhea through production of vasoactive intestinal peptide. Treatment of neuroblastoma includes surgery and radiation therapy for localized disease, and chemotherapy for metastatic disease.[6]
Pheochromocytoma
[edit]Pheochromocytoma is a neoplasm composed of cells similar to the chromaffin cells of the mature adrenal medulla. Pheochromocytomas occur in patients of all ages, and may be sporadic, or associated with a hereditary cancer syndrome, such as multiple endocrine neoplasia (MEN) types IIA and IIB, neurofibromatosis type I, or von Hippel–Lindau syndrome. Only 10% of adrenal pheochromocytomas are malignant, while the rest are benign tumors. The most clinically important feature of pheochromocytomas is their tendency to produce large amounts of the catecholamine hormones epinephrine (adrenaline) and norepinephrine. This may lead to potentially life-threatening high blood pressure, or cardiac arrhythmias, and numerous symptoms such as headache, palpitations, anxiety attacks, sweating, weight loss, and tremor. Diagnosis is most easily confirmed through urinary measurement of catecholamine metabolites such as VMA and metanephrines. Most pheochromocytomas are initially treated with anti-adrenergic drugs to protect against catecholamine overload, with surgery employed to remove the tumor once the patient is medically stable.[7]
Incidentalomas
[edit]An adrenal incidentaloma is an adrenal tumor found by coincidence without clinical symptoms or suspicion. It is one of the more common unexpected findings revealed by computed tomography (CT), magnetic resonance imaging (MRI), or ultrasonography.[8]
In these cases, a dexamethasone suppression test is often used to detect cortisol excess, and metanephrines or catecholamines for excess of these hormones. Tumors under 3 cm are generally considered benign and are only treated if there are grounds for a diagnosis of Cushing's syndrome or pheochromocytoma.[9] Radiodensity gives a clue in estimating malignancy risk, wherein a tumor with 10 Hounsfield units or less on an unenhanced CT is probably a lipid-rich adenoma.[10]
On CT scan, benign adenomas typically are of low radiographic density (due to fat content) and show rapid washout of contrast medium (50% or more of the contrast medium washes out at 10 minutes). If the hormonal evaluation is negative and imaging suggests benign, follow-up should be considered with imaging at 6, 12, and 24 months and repeat hormonal evaluation yearly for 4 years.[11]
Adrenal-dedicated CT and MRI imaging can be performed to distinguish benign adenomas from potentially malignant lesions.[12][13] Online calculators assist radiologists in calculating the washout of contrast in adrenal nodules on CT[14] and chemical shift on MRI.[15]
Hormonal evaluation can also be helpful, which includes:[11]
- 1-mg overnight dexamethasone suppression test
- 24-hour urinary specimen for measurement of fractionated metanephrines and catecholamines
- Blood plasma aldosterone concentration and plasma renin activity, if hypertension is present
Treatment
[edit]Surgical
For adrenal carcinomas, the most effective treatment is surgery, although this is not feasible for many patients, and the overall prognosis of the disease is poor. Chemotherapy, radiation therapy, and hormonal therapy may also be employed in the treatment of this disease.
A 2018 Cochrane Systematic review compared two different types of surgery: laparoscopic retroperotenial adrenalectomy and laporoscopic transperitoenal adrenelectomy in different types of adrenal tumors.[16] Laparoscopic retroperotenial adrenalectomy appeared to reduce late morbility, time to oral fluid or food intake and time to ambulation, when compared to laparoscopic transperitoenal adrenalectomy.[16] However there was uncertainty in these findings due to low-quality evidence, as well as inconclusive findings about effects of either surgery on all-cause mortality, early morbidity, socioeconomic effects, duration of surgery, operative blood loss, conversion to open surgery.[16]
Future diagnostic tools
[edit]Blood circulating microRNAs (miRNA) has been investigated in the recent years for the potential as a less-invasive biomarker for adrenal diseases. Nine studies have so far investigated the occurrence of circulating miRNAs in blood from patients diagnosed with adrenocortical tumors.[17][18] MiRNAs can be released into the blood stream by three different types of excretion.[19] Cellular damage with passive release (necrosis, inflammation), active secretion in the form of extracellular vesicles (EV) (microvesicles, exosomes and apoptotic bodies) or in association with high density lipoproteins (HDL) and Argonaute (AGO) proteins.[20][21] The majority of miRNAs found in blood are in complexes with AGO.[22][23] Despite the promising results, the sensitivity of potential circulating miRNA markers for adrenocortical tumors appears to be variable. An increase in sensitivity could possibly be achieved by targeting only EV-associated miRNAs as the release of miRNAs into EVs are hypothesized to be a controlled process.[24] EV-associated miRNAs could thereby act as more specific markers of malignancy.[24] However, as there were significant differences in the results of the studies performed, methodological differences and low patient numbers could contribute to this discrepancy. This calls for further studies on larger cohorts with uniform methodological requirements to clarify the applicability of circulating miRNAs as biomarkers of prognosis and malignancy in patients diagnosed with adrenocortical tumors.[17]
References
[edit]- ^ Data and references for pie chart are located at file description page in Wikimedia Commons.
- ^ Perappadan BS. "Doctors remove 'world's largest adrenal tumour'". The Hindu. Retrieved 2017-02-23.
- ^ List of included entries and references is found on main image page in Commons: File:Metastasis sites for common cancers.svg
- ^ a b Cingam SR, Karanchi H (2022). "Adrenal Metastasis". Cancer, Adrenal Metastasis. StatPearls. PMID 28722909.
{{cite book}}:|website=ignored (help) - ^ "Neuroblastoma". The Lecturio Medical Concept Library. Retrieved 11 August 2021.
- ^ Saab ST, MacLennan GT (2015). "Adrenal Cortical Neoplasms: Perspectives in Pediatric Patients". In Santulli G (ed.). Adrenal Glands: From Pathophysiology to Clinical Evidence. Nova Science. ISBN 978-1-63483-550-3.
- ^ Lenders JW, Eisenhofer G, Mannelli M, Pacak K (20–26 August 2005). "Phaeochromocytoma". Lancet. 366 (9486): 665–675. doi:10.1016/S0140-6736(05)67139-5. PMID 16112304. S2CID 208788653.
- ^ Arnold DT, Reed JB, Burt K (January 2003). "Evaluation and management of the incidental adrenal mass". Proceedings. 16 (1): 7–12. doi:10.1080/08998280.2003.11927882. PMC 1200803. PMID 16278716.
- ^ Grumbach MM, Biller BM, Braunstein GD, Campbell KK, Carney JA, Godley PA, et al. (March 2003). "Management of the clinically inapparent adrenal mass ("incidentaloma")". Annals of Internal Medicine. 138 (5): 424–429. doi:10.7326/0003-4819-138-5-200303040-00013. PMID 12614096. S2CID 23454526.
- ^ Willatt JM, Francis IR (June 2010). "Radiologic evaluation of incidentally discovered adrenal masses". American Family Physician. 81 (11): 1361–1366. PMID 20521756.
- ^ a b Young WF (February 2007). "Clinical practice. The incidentally discovered adrenal mass". The New England Journal of Medicine. 356 (6): 601–610. doi:10.1056/NEJMcp065470. PMID 17287480.
- ^ Nandra, Gurinder; Duxbury, Oliver; Patel, Pawan; Patel, Jaymin H.; Patel, Nirav; Vlahos, Ioannis (2020). "Technical and Interpretive Pitfalls in Adrenal Imaging". Radiographics. 40 (4): 1041–1060. doi:10.1148/rg.2020190080. ISSN 1527-1323. PMID 32609593.
- ^ Adam, Sharon Z.; Nikolaidis, Paul; Horowitz, Jeanne M.; Gabriel, Helena; Hammond, Nancy A.; Patel, Tanvi; Yaghmai, Vahid; Miller, Frank H. (2016). "Chemical Shift MR Imaging of the Adrenal Gland: Principles, Pitfalls, and Applications". Radiographics. 36 (2): 414–432. doi:10.1148/rg.2016150139. ISSN 1527-1323. PMID 26849154.
- ^ "Adrenal Washout Calculator for CT". Rad At Hand. Retrieved 2024-07-09.
- ^ "Adrenal Chemical Shift MRI Calculator". Rad At Hand. Retrieved 2024-07-09.
- ^ a b c Arezzo A, Bullano A, Cochetti G, Cirocchi R, Randolph J, Mearini E, et al. (Cochrane Metabolic and Endocrine Disorders Group) (December 2018). "Transperitoneal versus retroperitoneal laparoscopic adrenalectomy for adrenal tumours in adults". The Cochrane Database of Systematic Reviews. 2018 (12): CD011668. doi:10.1002/14651858.CD011668.pub2. PMC 6517116. PMID 30595004.
- ^ a b Decmann A, Perge P, Turai PI, Patócs A, Igaz P (February 2020). "Non-Coding RNAs in Adrenocortical Cancer: From Pathogenesis to Diagnosis". Cancers. 12 (2): 461. doi:10.3390/cancers12020461. PMC 7072220. PMID 32079166.
- ^ Vetrivel S, Zhang R, Engel M, Altieri B, Braun L, Osswald A, et al. (2021-02-22). "Circulating microRNA Expression in Cushing's Syndrome". Frontiers in Endocrinology. 12: 620012. doi:10.3389/fendo.2021.620012. PMC 7937959. PMID 33692756.
- ^ Perge P, Nagy Z, Igaz I, Igaz P (April 2015). "Suggested roles for microRNA in tumors". Biomolecular Concepts. 6 (2): 149–155. doi:10.1515/bmc-2015-0002. PMID 25870972. S2CID 8376269.
- ^ Redis RS, Calin S, Yang Y, You MJ, Calin GA (November 2012). "Cell-to-cell miRNA transfer: from body homeostasis to therapy". Pharmacology & Therapeutics. 136 (2): 169–174. doi:10.1016/j.pharmthera.2012.08.003. PMC 3855335. PMID 22903157.
- ^ Zen K, Zhang CY (March 2012). "Circulating microRNAs: a novel class of biomarkers to diagnose and monitor human cancers". Medicinal Research Reviews. 32 (2): 326–348. doi:10.1002/med.20215. PMID 22383180. S2CID 13429401.
- ^ Arroyo JD, Chevillet JR, Kroh EM, Ruf IK, Pritchard CC, Gibson DF, et al. (March 2011). "Argonaute2 complexes carry a population of circulating microRNAs independent of vesicles in human plasma". Proceedings of the National Academy of Sciences of the United States of America. 108 (12): 5003–5008. Bibcode:2011PNAS..108.5003A. doi:10.1073/pnas.1019055108. PMC 3064324. PMID 21383194.
- ^ Turchinovich A, Weiz L, Langheinz A, Burwinkel B (September 2011). "Characterization of extracellular circulating microRNA". Nucleic Acids Research. 39 (16): 7223–7233. doi:10.1093/nar/gkr254. PMC 3167594. PMID 21609964.
- ^ a b Valadi H, Ekström K, Bossios A, Sjöstrand M, Lee JJ, Lötvall JO (June 2007). "Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells". Nature Cell Biology. 9 (6): 654–659. doi:10.1038/ncb1596. PMID 17486113. S2CID 8599814.
Further reading
[edit]- Santulli G, ed. (2015). Adrenal Glands: From Pathophysiology to Clinical Evidence. New York, NY: Nova Science. ISBN 978-1-63483-570-1.
- Cotran R, Kumar V, Collins T (1999). Robbins Pathologic Basis of Disease (Sixth ed.). W.B. Saunders. ISBN 978-0-7216-7335-6.
- Cote R, Suster S, Weiss L (2003). Noel Weidner (ed.). Modern Surgical Pathology (2 Volume Set). London: W B Saunders. ISBN 978-0-7216-7253-3.
