Amyloidosis: Difference between revisions
PhnomPencil (talk | contribs) m Carefully removing and/or (see MOS:ANDOR and my explanation), replaced: and/or → or using AWB |
No edit summary |
||
| Line 76: | Line 76: | ||
| [[gelsolin|GSN]] |
| [[gelsolin|GSN]] |
||
| [[Finnish type amyloidosis]] |
| [[Finnish type amyloidosis]] |
||
| {{OMIM2|105120}} |
| {{OMIM2|105120}}jigaboio |
||
|- |
|- |
||
| '''ACys''' |
| '''ACys''' |
||
Revision as of 06:27, 17 April 2012
| Amyloidosis | |
|---|---|
| Specialty | Endocrinology, cardiology, hematology |
In medicine, amyloidosis refers to a variety of conditions wherein amyloid proteins are abnormally deposited in organs or tissues and cause harm. A protein is described as being amyloid if, due to an alteration in its secondary structure, it takes on a particular aggregated insoluble form, similar to the beta-pleated sheet.[1] Symptoms vary widely depending upon where in the body amyloid deposits accumulate. Amyloidosis may be inherited or acquired.[2]
Classification of amyloid
The modern classification of amyloid disease tends to use an abbreviation of the protein that makes the majority of deposits, prefixed with the letter A. For example, amyloidosis caused by transthyretin is termed "ATTR." Deposition patterns vary between patients but are almost always composed of just one amyloidogenic protein. Deposition can be systemic (affecting many different organ systems) or organ-specific. Many amyloidoses are inherited, due to mutations in the precursor protein.
Other forms are due to different diseases causing overabundant or abnormal protein production - such as with overproduction of immunoglobulin light chains in multiple myeloma (termed AL amyloidosis), or with continuous overproduction of acute phase proteins in chronic inflammation (which can lead to AA amyloidosis).
Out of the approximately 60 amyloid proteins that have been identified so far,[3] at least 36 have been associated in some way with a human disease.[4]
Pathogenesis
When a native cell creates a protein, it could either make the actual protein or protein fragments. These fragments could come and join together to form the actual protein. Such a protein can sometimes regress into the protein fragments. This process of "flip flopping" happens frequently in certain proteins, especially the ones that cause this disease.
The fragments or actual proteins are at risk of mis-folding as they are synthesized, to make a bad protein. This causes proteolysis, which is the directed degradation of proteins by cellular enzymes called proteases or by intramolecular digestion; proteases come and digest the mis-folded fragments and proteins. The problem occurs when the proteins do not dissolve in proteolysis. This happens because the mis-folded proteins sometimes become robust enough that they are not dissolved by normal proteolysis. When the fragments do not dissolve, they get spit out of proteolysis and they aggregate to form oligomers. The reason they aggregate is that the parts of the protein that do not dissolve in proteolysis are the β-pleated sheets, which are extremely hydrophobic. They are usually sequestered in the middle of the protein, while parts of the protein that are more soluble are found near the outside. When they are exposed to water, these hydrophobic pieces tend to aggregate with other hydrophobic pieces. This ball of fragments gets stabilized by GAG's (glycosaminoglycans) and SAP (serum amyloid P, a component found in amyloid aggregations that is thought to stabilize them and prevent proteolytic cleavage). The stabilized balls of protein fragments are called oligomers. The oligomers can aggregate together and further stabilize to make amyloid fibrils.
Both the oligomers and amyloid fibrils can cause cell toxicity and organ dysfunction.[5]
Classification
The names of the amyloid usually start with the letter "A". Following is a brief description of the more common types of amyloid:
As of 2010, there were 27 human and nine animal fibril proteins classified, along with eight inclusion bodies.[7]
Symptoms
There are numerous symptoms that are associated with this disease. The most common ones have to do with the heart, such as heart failure, arrhythmia, and an irregular heartbeat. Also, the respiratory tract can be affected and cause hemoptysis. Usually, the spleen enlarges and sometimes ruptures. The gastrointestinal tract is usually affected and causes vomiting, hemorrhaging and diarrhea. Amyloidosis can also affect the body's motor functions and cause polyneuropathy.
When the amyloid fibrils and oligomers get to the skin, they can cause skin lesions and petechiae.
One of the most famous symptoms is macroglossia.[5]
Diagnosis
If diagnosis of amyloidosis is suspected, a tissue sample of abdominal wall fat, the rectum or a salivary gland, can be examined in biopsy for evidence of characteristic amyloid deposits.
The tissue is treated with various stains. The most useful stain in the diagnosis of amyloid is Congo red, which, combined with polarized light, makes the amyloid proteins appear apple-green on microscopy. Alternatively, thioflavin T stain may be used.[8] An abdominal wall fat biopsy is not completely sensitive and, sometimes, biopsy of an involved organ (such as the kidney) is required to achieve a diagnosis.[8]
The nature of the amyloid protein can be determined by various ways: the detection of abnormal proteins in the bloodstream (on protein electrophoresis or light chain determination), binding of particular antibodies to the amyloid found in the tissue, or extraction of the protein and identification of its individual amino acids.[8]
Alternative classifications
An older, clinical, method of classification refers to amyloidoses as systemic or localised
- Systemic amyloidoses affect more than one body organ or system. Examples are: AL, AA and Aβ2m.[9]
- Localised amyloidoses affect only one body organ or tissue type. Examples are: Aβ, IAPP, Atrial natriuretic factor (in isolated atrial amyloidosis) and Calcitonin (in medullary carcinoma of the thyroid)[9]
Another classification is primary or secondary.
- Primary amyloidoses arise from a disease with disordered immune cell function such as multiple myeloma and other immunocyte dyscrasias.
- Secondary (reactive) amyloidoses are those occurring as a complication of some other chronic inflammatory or tissue destructive disease. Examples are reactive systemic amyloidosis and secondary cutaneous amyloidosis.[9]
Additional images
-
Small bowel duodenum with amyloid deposition congo red 10X
-
Amyloidosis, dystrophic calcification
-
Small bowel duodenum with amyloid deposition 20X
-
Amyloidosis, Node, Congo Red
-
Amyloidosis, blood vessels, H&E
-
Amyloidosis, lymph node, H&E
-
Amyloidosis, lymph node, polarizer
See also
References
- ^ "Atlas of Pathology".
- ^ Pavelka, Margit; Roth, Jürgen. Functional Ultrastructure: An Atlas of Tissue Biology and Pathology. Springer. p. 258. ISBN 3-211-83564-4.
{{cite book}}: Cite has empty unknown parameter:|coauthors=(help)CS1 maint: multiple names: authors list (link) - ^ Mok KH, Pettersson J, Orrenius S, Svanborg C (2007). "HAMLET, protein folding, and tumor cell death". Biochem. Biophys. Res. Commun. 354 (1): 1–7. doi:10.1016/j.bbrc.2006.12.167. PMID 17223074.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Pettersson-Kastberg J, Aits S, Gustafsson L; et al. (2008). "Can misfolded proteins be beneficial? The HAMLET case". Ann. Med. 41 (3): 1–15. doi:10.1080/07853890802502614. PMID 18985467.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b [1], Karp, Judith E., ed. Amyloidosis Diagnosis and Treatment. Rochester: Humana, 2010. Online Source. .
- ^ Hassan W, Al-Sergani H, Mourad W, Tabbaa R (2005). "Amyloid heart disease. New frontiers and insights in pathophysiology, diagnosis, and management". Tex Heart Inst J. 32 (2): 178–84. PMC 1163465. PMID 16107109.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sipe JD, Benson MD, Buxbaum JN; et al. (2010). "Amyloid fibril protein nomenclature: 2010 recommendations from the nomenclature committee of the International Society of Amyloidosis". Amyloid. 17 (3–4): 101–104. doi:10.3109/13506129.2010.526812. PMID 21039326.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c Dember LM (2006). "Amyloidosis-associated kidney disease". J. Am. Soc. Nephrol. 17 (12): 3458–71. doi:10.1681/ASN.2006050460. PMID 17093068.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b c Table 5-12 in: Mitchell, Richard Sheppard; Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson (2007). Robbins Basic Pathology. Philadelphia: Saunders. ISBN 1-4160-2973-7.
{{cite book}}: CS1 maint: multiple names: authors list (link) 8th edition.



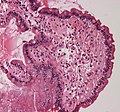




![Cardiac amyloidosis[disambiguation needed]. H&E stain.](http://upload.wikimedia.org/wikipedia/commons/thumb/1/16/Cardiac_amyloidosis_very_high_mag_he.jpg/120px-Cardiac_amyloidosis_very_high_mag_he.jpg)