Deferasirox
 | |
 | |
| Clinical data | |
|---|---|
| License data |
|
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 70% |
| Protein binding | 99% |
| Metabolism | Hepatic glucuronidation |
| Elimination half-life | 8 to 16 hours |
| Excretion | Fecal (84%) and renal (8%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.211.077 |
| Chemical and physical data | |
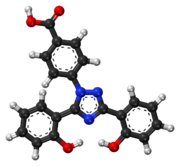
| Formula | C21H15N3O4 |
| Molar mass | 373.362 g/mol g·mol−1 |
| 3D model (JSmol) | |
| Density | 1.4±0.1[2] g/cm3 |
| |
| |
| | |
Deferasirox (marketed as Exjade,[3] Desirox, Defrijet, Desifer, Rasiroxpine and Jadenu) is an oral iron chelator. Its main use is to reduce chronic iron overload in patients who are receiving long-term blood transfusions for conditions such as beta-thalassemia and other chronic anemias.[4][5] It is the first oral medication approved in the USA for this purpose.[6]
It was approved by the United States Food and Drug Administration (FDA) in November 2005.[4][6] According to FDA (May 2007), renal failure and cytopenias have been reported in patients receiving deferasirox oral suspension tablets. It is approved in the European Union by the European Medicines Agency (EMA) for children 6 years and older for chronic iron overload from repeated blood transfusions.[7][8][9]
Properties

The half-life of deferasirox is between 8 and 16 hours allowing once a day dosing. Two molecules of deferasirox are capable of binding to 1 atom of iron which are subsequently eliminated by fecal excretion. Its low molecular weight and high lipophilicity allows the drug to be taken orally unlike deferoxamine which has to be administered by IV route (intravenous infusion). Together with deferiprone, deferasirox seems to be capable of removing iron from cells (cardiac myocytes and hepatocytes) as well as removing iron from the blood.
Synthesis
Deferasirox can be prepared from simple commercially available starting materials (salicylic acid, salicylamide and 4-hydrazinobenzoic acid) in the following two-step synthetic sequence:

The condensation of salicyloyl chloride (formed in situ from salicylic acid and thionyl chloride) with salicylamide under dehydrating reaction conditions results in formation of 2-(2-hydroxyphenyl)-1,3(4H)-benzoxazin-4-one. This intermediate is isolated and reacted with 4-hydrazinobenzoic acid in the presence of base to give 4-(3,5-bis(2-hydroxyphenyl)-1,2,4-triazol-1-yl)benzoic acid (Deferasirox).[10]
Risks
Deferasirox was the #2 drug on the list of 'Most frequent suspected drugs in reported patient deaths' compiled by the Institute for Safe Medical Practices in 2009. There were 1320 deaths reported, perhaps explained by an update to the ADE data of Novartis, and a new boxed warning about gastrointestinal haemorrhage as well as kidney and liver failure.[11]
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ "Material Safety Data Sheet (MSDS): Deferasirox". ChemSrc. 2018.
- ^ "EXJADE (deferasirox)". Novartis AG.
- ^ a b Choudhry VP, Naithani R (August 2007). "Current status of iron overload and chelation with deferasirox". Indian Journal of Pediatrics. 74 (8): 759–64. doi:10.1007/s12098-007-0134-7. PMID 17785900. Free full text Archived 2014-04-29 at the Wayback Machine
- ^ Yang LP, Keam SJ, Keating GM (2007). "Deferasirox : a review of its use in the management of transfusional chronic iron overload". Drugs. 67 (15): 2211–30. doi:10.2165/00003495-200767150-00007. PMID 17927285.
- ^ a b "FDA Approves First Oral Drug for Chronic Iron Overload" (Press release). United States Food and Drug Administration. November 9, 2005. Retrieved 2007-10-31.
- ^ "Exjade – deferasirox" (PDF). European Medicines Agency. 2018.
- ^ Kontoghiorghes GJ (April 2013). "Turning a blind eye to deferasirox's toxicity?". Lancet. 381 (9873): 1183–4. doi:10.1016/S0140-6736(13)60799-0. PMID 23561999.
- ^ "Review: Exjade side effects".
- ^ Steinhauser S, Heinz U, Bartholomä M, Weyhermüller T, Nick H, Hegetschweiler K (2004). "Complex Formation of ICL670 and Related Ligands with FeIII and FeII". European Journal of Inorganic Chemistry. 2004 (21): 4177–4192. doi:10.1002/ejic.200400363.]
- ^ ISMP (2010). "ISMP QuarterWatch(TM)". Vol. 15, no. 12. ISMP Medication Safety Alert. pp. 1–3.
