Endometrial polyp
| Endometrial polyp | |
|---|---|
| Other names | Uterine polyp |
 | |
| Endometrial polyp, viewed by sonography | |
| Specialty | Gynecology |
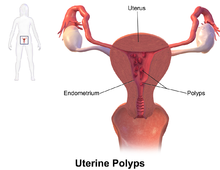
An endometrial polyp or uterine polyp is a mass in the inner lining of the uterus.[1] They may have a large flat base (sessile) or be attached to the uterus by an elongated pedicle (pedunculated).[1][2] Pedunculated polyps are more common than sessile ones.[3] They range in size from a few millimeters to several centimeters.[2] If pedunculated, they can protrude through the cervix into the vagina.[1][4] Small blood vessels may be present, particularly in large polyps.[1]
Signs and symptoms
They often cause no symptoms.[3] Where they occur, symptoms include irregular menstrual bleeding, bleeding between menstrual periods, excessively heavy menstrual bleeding (menorrhagia), and vaginal bleeding after menopause.[2][5] Bleeding from the blood vessels of the polyp contributes to an increase of blood loss during menstruation and blood "spotting" between menstrual periods, or after menopause.[6] If the polyp protrudes through the cervix into the vagina, pain (dysmenorrhea) may result.[4]
Cause
No definitive cause of endometrial polyps is known, but they appear to be affected by hormone levels and grow in response to circulating estrogen.[2] Risk factors include obesity, high blood pressure and a history of cervical polyps.[2] Taking tamoxifen or hormone replacement therapy can also increase the risk of uterine polyps.[2][7] The use of an intrauterine system containing levonorgestrel in women taking tamoxifen may reduce the incidence of polyps.[8]
Diagnosis

Endometrial polyps can be detected by vaginal ultrasound (sonohysterography), hysteroscopy and dilation and curettage.[2] Detection by ultrasonography can be difficult, particularly when there is endometrial hyperplasia (excessive thickening of the endometrium).[1] Larger polyps may be missed by curettage.[9]
Endometrial polyps can be solitary or occur with others.[10] They are round or oval and measure between a few millimeters and several centimeters in diameter.[6][10] They are usually the same red/brown color of the surrounding endometrium although large ones can appear to be a darker red.[6] The polyps consist of dense, fibrous tissue (stroma), blood vessels and glandlike spaces lined with endometrial epithelium.[6] If they are pedunculated, they are attached by a thin stalk (pedicle). If they are sessile, they are connected by a flat base to the uterine wall.[10] Pedunculated polyps are more common than sessile ones.[3]
Treatment
Polyps can be surgically removed using curettage with or without hysteroscopy.[11] When curettage is performed without hysteroscopy, polyps may be missed. To reduce this risk, the uterus can be first explored using grasping forceps at the beginning of the curettage procedure.[6] Hysteroscopy involves visualising the endometrium (inner lining of the uterus) and polyp with a camera inserted through the cervix. If it is a large polyp, it can be cut into sections before each section is removed.[6] If cancerous cells are discovered, a hysterectomy (surgical removal of the uterus) may be performed.[2] A hysterectomy would usually not be considered if cancer has been ruled out.[6] Whichever method is used, polyps are usually treated under general anesthetic.[9]
It is unclear if removing polyps affects fertility as it has not been studied.[12]
Prognosis
Endometrial polyps are usually benign although some may be precancerous or cancerous.[2] About 0.5% of endometrial polyps contain adenocarcinoma cells.[13] Polyps can increase the risk of miscarriage in women undergoing IVF treatment.[2] If they develop near the fallopian tubes, they may lead to difficulty in becoming pregnant.[2] Although treatments such as hysteroscopy usually cure the polyp concerned, recurrence of endometrial polyps is frequent.[6] Untreated, small polyps may regress on their own.[14]
Epidemiology
Endometrial polyps usually occur in women in their 40s and 50s.[2] Endometrial polyps occur in up to 10% of women.[1] It is estimated that they are present in 25% of women with abnormal vaginal bleeding.[7]
See also
References
- ^ a b c d e f Jane A. Bates (1997). Practical Gynaecological Ultrasound. Cambridge, UK: Cambridge University Press. ISBN 1-900151-51-0.
- ^ a b c d e f g h i j k l "Uterine polyps". MayoClinic.com. 2006-04-27.
- ^ a b c Sternberg, Stephen S.; Stacey E. Mills; Darryl Carter (2004). Sternberg's Diagnostic Surgical Pathology. Lippincott Williams & Wilkins. p. 2460. ISBN 0-7817-4051-7.
- ^ a b Dysmenorrhea: Menstrual abnormalities at Merck Manual of Diagnosis and Therapy Professional Edition
- ^ "Endometrial Polyp". GPnotebook. Retrieved 2007-10-20.
- ^ a b c d e f g h DeCherney, Alan H.; Lauren Nathan (2003). Current Obstetric & Gynecologic Diagnosis & Treatment. McGraw-Hill Professional. p. 703. ISBN 0-8385-1401-4.
- ^ a b Edmonds, D. Keith; Sir John Dewhurst (2006). Dewhurst's Textbook of Obstetrics and Gynaecology. Blackwell Publishing. p. 637. ISBN 1-4051-5667-8.
- ^ Chan SS, Tam WH, Yeo W, et al. (2007). "A randomised controlled trial of prophylactic levonorgestrel intrauterine system in tamoxifen-treated women". BJOG. 114 (12): 1510–5. doi:10.1111/j.1471-0528.2007.01545.x. PMID 17995495.
- ^ a b Macnair, Trisha. "Ask the doctor – Uterine polyps". BBC Health. Retrieved 2007-10-21.
- ^ a b c Bajo Arenas, José M.; Asim Kurjak (2005). Donald School Textbook Of Transvaginal Sonography. Taylor & Francis. p. 502. ISBN 1-84214-331-X.
- ^ "Uterine bleeding – Signs and Symptoms". UCSF Medical Center. 2007-05-08. Archived from the original on 2008-04-11. Retrieved 2007-10-20.
- ^ Jayaprakasan, K; Polanski, L; Sahu, B; Thornton, JG; Raine-Fenning, N (Aug 30, 2014). "Surgical intervention versus expectant management for endometrial polyps in subfertile women" (PDF). The Cochrane Database of Systematic Reviews. 8: CD009592. doi:10.1002/14651858.CD009592.pub2. PMID 25172985.
- ^ Rubin, Raphael; David S Strayer (2007). Rubin's Pathology: Clinicopathologic Foundations of Medicine. Lippincott Williams & Wilkins. p. 806. ISBN 0-7817-9516-8.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Kaunitz, Andrew M. (2002-08-26). "Asymptomatic Endometrial Polyps: What Is the Likelihood of Cancer?". Medscape Ob/Gyn & Women's Health. Retrieved 2008-04-20.
