Glycogen storage disease
| Glycogen storage disease | |
|---|---|
| Other names | Gycogenosis, dextrinosis |
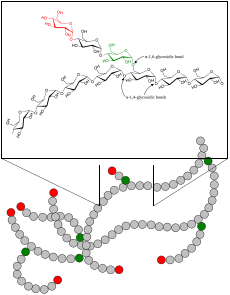 | |
| Glycogen | |
| Specialty | Endocrinology |
A glycogen storage disease (GSD, also glycogenosis and dextrinosis) is a metabolic disorder caused by enzyme deficiencies affecting either glycogen synthesis, glycogen breakdown or glycolysis (glucose breakdown), typically within muscles and/or liver cells.[citation needed]
GSD has two classes of cause: genetic and acquired. Genetic GSD is caused by any inborn error of metabolism (genetically defective enzymes) involved in these processes. In livestock, acquired GSD is caused by intoxication with the alkaloid castanospermine.[1]
Types
| Type (Eponym) |
Enzyme deficiency (Gene[2]) |
Incidence (births) | Hypo- glycemia? |
Hepato- megaly? |
Hyperlip- idemia? |
Muscle symptoms | Development/ prognosis | Other symptoms |
|---|---|---|---|---|---|---|---|---|
| GSD 0 | Glycogen synthase (GYS2) |
? | Yes | No | No | Occasional muscle cramping | Growth failure in some cases | |
| GSD I / GSD 1 (von Gierke's disease) |
Glucose-6-phosphatase (G6PC / SLC37A4) |
1 in 50,000 – 100,000[3][4] | Yes | Yes | Yes | None | Growth failure | Lactic acidosis, hyperuricemia |
| GSD II / GSD 2 (Pompe's disease ) |
Acid alpha-glucosidase (GAA) |
1 in 40,000 – 50,000.[5][6] | No | Yes | No | Muscle weakness | *Death by age ~2 years (infantile variant) | Heart failure |
| GSD III / GSD 3 (Cori's disease or Forbes' disease) |
Glycogen debranching enzyme (AGL) |
1 in 100,000 | Yes | Yes | Yes | Myopathy | ||
| GSD IV / GSD 4 (Andersen disease) |
Glycogen branching enzyme (GBE1) |
1 in 500,000[6] | No | Yes, also cirrhosis |
No | Myopathy and dilated cardiomyopathy (it was set to none) | Failure to thrive, death at age ~5 years | |
| GSD V / GSD 5 (McArdle disease) |
Muscle glycogen phosphorylase (PYGM) |
1 in 100,000 – 500,000[7][6] | No | No | No | Exercise-induced cramps, Rhabdomyolysis | Renal failure by myoglobinuria, second wind phenomenon | |
| GSD VI / GSD 6 (Hers' disease) |
Liver glycogen phosphorylase (PYGL) Muscle phosphoglycerate mutase (PGAM2) |
1 in 65,000 – 85,000[8] | Yes | Yes | Yes [9] | None | initially benign, developmental delay follows. | |
| GSD VII / GSD 7 (Tarui's disease) |
Muscle phosphofructokinase (PKFM) |
1 in 1,000,000[10] | No | No | No | Exercise-induced muscle cramps and weakness | developmental delay | In some haemolytic anaemia |
| GSD IX / GSD 9 | Phosphorylase kinase (PHKA2 / PHKB / PHKG2 / PHKA1) |
? | Yes | Yes | Yes | None | Delayed motor development, Developmental delay | |
| GSD X / GSD 10 | Enolase 3 (ENO3) |
? | ? | ? | ? | |||
| GSD XI / GSD 11 | Muscle lactate dehydrogenase (LDHA) |
? | ? | ? | ? | |||
| Fanconi-Bickel syndrome formerly GSD XI / GSD 11, no longer considered a GSD |
Glucose transporter (GLUT2) |
? | Yes | Yes | No | None | ||
| GSD XII / GSD 12 (Aldolase A deficiency) |
Aldolase A (ALDOA) |
? | ? | In some | ? | Exercise intolerance, cramps. In some Rhabdomyolysis. | Hemolytic anemia and other symptoms | |
| GSD XIII / GSD 13 | β-enolase (ENO3) |
? | ? | ? | ? | Exercise intolerance, cramps | Increasing intensity of myalgias over decades[11] | Serum CK: Episodic elevations; Reduced with rest[11] |
| GSD XV / GSD 15 | Glycogenin-1 (GYG1) |
Rare[12] | No | No | No | Muscle atropy | Slowly progressive weakness over decades | None |
Remarks:
- Some GSDs have different forms, e.g. infantile, juvenile, adult (late-onset).
- Some GSDs have different subtypes, e.g. GSD1a / GSD1b, GSD9A1 / GSD9A2 / GSD9B / GSD9C / GSD9D.[2]
- GSD type 0: Although glycogen synthase deficiency does not result in storage of extra glycogen in the liver, it is often classified with the GSDs as type 0 because it is another defect of glycogen storage and can cause similar problems.
- GSD type VIII (GSD 8): In the past it was considered a distinct condition,[13] however it is now classified with GSD type VI[14] or GSD IXa1;[15] it has been described as X-linked recessive inherited.[16]
- GSD type XI (GSD 11): Fanconi-Bickel syndrome, hepatorenal glycogenosis with renal Fanconi syndrome, no longer considered a glycogen storage disease.[2]
- GSD type XIV (GSD 14): Now classed as Congenital disorder of glycosylation type 1 (CDG1T), affects the phosphoglucomutase enzyme (gene PGM1).[2]
- Lafora disease is considered a complex neurodegenerative disease and also a glycogen metabolism disorder.[17]
Diagnosis

This section needs expansion. You can help by adding to it. (November 2017) |
Treatment
Treatment is depended on the type of glycogen storage disease. E.g. GSD I is typically treated with frequent small meals of carbohydrates and cornstarch to prevent low blood sugar, while other treatments may include allopurinol and human granulocyte colony stimulating factor.[18]
Epidemiology
Overall, according to a study in British Columbia, approximately 2.3 children per 100,000 births (1 in 43,000) have some form of glycogen storage disease.[19] In the United States, they are estimated to occur in 1 per 20,000–25,000 births.[3] Dutch incidence rate is estimated to be 1 per 40,000 births.
References
- ^ Stegelmeier BL, Molyneux RJ, Elbein AD, James LF (May 1995). "The lesions of locoweed (Astragalus mollissimus), swainsonine, and castanospermine in rats". Veterinary Pathology. 32 (3): 289–98. doi:10.1177/030098589503200311. PMID 7604496.
- ^ a b c d Glycogen Metabolism themedicalbiochemistrypage.org
- ^ a b eMedicine Specialties > Glycogen-Storage Disease Type I Author: Karl S Roth. Updated: Aug 31, 2009
- ^ The Association for Glycogen Storage Disease > Type I Glycogen Storage Disease Type I GSD Archived 2010-08-03 at the Wayback Machine October 2006.
- ^ Ausems MG, Verbiest J, Hermans MP, et al. (September 1999). "Frequency of glycogen storage disease type II in The Netherlands: implications for diagnosis and genetic counselling". Eur. J. Hum. Genet. 7 (6): 713–716. doi:10.1038/sj.ejhg.5200367. PMID 10482961.
- ^ a b c [1]
- ^ http://mcardlesdisease.org/
- ^ eMedicine Specialties > Pediatrics: Genetics and Metabolic Disease > Metabolic Diseases > Glycogen-Storage Disease Type VI Author: Lynne Ierardi-Curto, MD, PhD. Updated: Aug 4, 2008
- ^ Goldman, Lee; Schafer, Andrew (2012). Goldman's Cecil medicine (24th ed.). Philadelphia: Elsevier/Saunders. p. 1356. ISBN 978-1-4377-1604-7.
- ^ "Rare Disease Database". Orpha.net. Retrieved 2015-09-20.
- ^ a b http://neuromuscular.wustl.edu/msys/glycogen.html#enolase
- ^ Malfatti E, Nilsson J, Hedberg-Oldfors C, Hernandez-Lain A, Michel F, Dominguez-Gonzalez C, Viennet G, Akman HO, Kornblum C, Van den Bergh P, Romero NB, Engel AG, DiMauro S, Oldfors A (2014) A new muscle glycogen storage disease associated with glycogenin-1 deficiency. Ann Neurol 76(6):891-898
- ^ Ludwig M, Wolfson S, Rennert O (October 1972). "Glycogen storage disease, type 8". Arch. Dis. Child. 47 (255): 830–833. doi:10.1136/adc.47.255.830. PMC 1648209. PMID 4508182.
- ^ "Glycogen-Storage Disease Type VI : Article by Lynne Ierardi-Curto". eMedicine.
- ^ GLYCOGEN STORAGE DISEASE IXa1; GSD9A1 OMIM - Online Mendelian Inheritance in Man
- ^ "Definition: glycogen storage disease type VIII from Online Medical Dictionary".
- ^ Ortolano S, Vieitez I et al. Loss of cortical neurons underlies the neuropathology of Lafora disease. Mol Brain 2014;7:7 PMC 3917365
- ^ "Glycogen Storage Disease Type I - NORD (National Organization for Rare Disorders)". NORD (National Organization for Rare Disorders). Retrieved 23 March 2017.
- ^ Applegarth DA, Toone JR, Lowry RB (January 2000). "Incidence of inborn errors of metabolism in British Columbia, 1969–1996". Pediatrics. 105 (1): e10. doi:10.1542/peds.105.1.e10. PMID 10617747.
