Juxtaglomerular apparatus

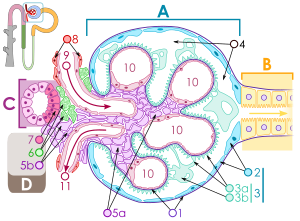
The juxtaglomerular apparatus is a microscopic structure in the kidney, which regulates the function of each nephron. The juxtaglomerular apparatus is named for its proximity to the glomerulus: it is found between the vascular pole of the renal corpuscle and the returning thick ascending limb of the same nephron. This location is critical to its function in regulating renal blood flow and glomerular filtration rate. The three cellular components of the apparatus are the macula densa, extraglomerular mesangial cells, and juxtaglomerular cells.
Cells of the Juxtaglomerular Apparatus
There are 3 different types of cells in the Juxtaglomerular Apparatus: Juxtaglomerular Cells, Macula Densa Cells, and lacis cells
Granular Cells
Granular cells are modified pericytes of glomerular arterioles. They are also known as Juxtaglomerular cells (juxtaglomerular cells are not granular cells but are granulated as they release Renin).
The Juxtaglomerular cells secrete renin in response to:
- Beta1 adrenergic stimulation
- Decrease in renal perfusion pressure (detected directly by the granular cells)
- Decrease in NaCl reabsorption in the Macula Densa (often due to a decrease in glomerular filtration rate, or GFR, due to slower filtrate movement through the proximal tubule and thus more time for reabsorption. This results in a lower NaCl concentration by the time the filtrate reaches the Macula Densa).
Macula Densa Cells
Macula densa cells are columnar epithelium thickening of the distal tubule. The macula densa senses sodium chloride concentration in the distal tubule of the kidney and secretes a locally active (paracrine) vasopressor which acts on the adjacent afferent arteriole to decrease glomerular filtration rate (GFR), as part of the tubuloglomerular feedback loop. Specifically, excessive filtration at the glomerulus or inadequate sodium uptake in the proximal tubule / thick ascending loop of Henle brings fluid to the distal convoluted tubule that has an abnormally high concentration of sodium. Na/Cl cotransporters move sodium into the cells of the macula densa. The macula densa cells do not have enough basolateral Na/K ATPases to excrete this added sodium, so the cell's osmolarity increases. Water flows into the cell to bring the osmolarity back down, causing the cell to swell. When the cell swells, a stretch-activated non-selective anion channel is opened on the basolateral surface. ATP escapes through this channel and is subsequently converted to adenosine. Adenosine vasoconstricts the afferent arteriole via A1 receptors and vasodilates (to a lesser degree) efferent arterioles via A2 receptors which decreases GFR. Also, adenosine inhibits renin release in JG cells via A2 receptors on JG cells using Gi pathway. Also, when macula densa cells detect higher concentrations of Na and Cl they inhibit Nitric Oxide Synthetase (decreasing renin release) with an unknown pathway.
A decrease in GFR means less solute in the tubular lumen. As the filtrate reaches the macula densa, less NaCl is re-absorbed. The macula densa cells detect lower concentrations in Na and Cl and upregulate Nitric Oxide Synthetase (NOS). NOS creates NO which catalyses the formation of prostaglandins. These prostaglandins diffuse to the granular cells and activate a prostaglandin specific Gs receptor. This receptor activates adenylate cyclase which increases levels of cAMP. cAMP augments renin release. Prostaglandins and NO also vasodilate the afferent arterioles. Efferent arterioles are spared from this effect by renin release.
See also
References
