Sexual anomalies
Sexual anomalies, also known as sexual abnormalities, are a set of clinical conditions due to chromosomal, gonadal and/or genitalia variation. Individuals with congenital (inborn) discrepancy between sex chromosome, gonadal, and their internal and external genitalia are categorised as individuals with a disorder of sex development (DSD).[1] Afterwards, if the family or individual wishes, they can partake in different management and treatment options for their conditions (e.g. hormone therapy).
Infants born with atypical genitalia often cause confusion and distress for the family. Psychosexual development is influenced by numerous factors that include, but are not limited to, gender differences in brain structure, genes associated with sexual development, prenatal androgen exposure, interactions with family, and cultural and societal factors.[2] Because of the complex and multifaceted factors involved, communication and psychosexual support are all important.
A team of experts, or patient support groups, are usually recommended for cases related to sexual anomalies. This team of experts are usually derived from a variety of disciplines including pediatricians, neonatologists, pediatric urologists, pediatric general surgeons, endocrinologists, geneticists, radiologists, psychologists and social workers.[3][4][5] These professionals are capable of providing first line (prenatal) and second line diagnostic (postnatal) tests to examine and diagnose sexual anomalies.
Overview
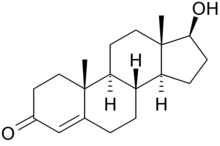
In the normal prenatal stages of fetal development, the fetus is exposed to testosterone - albeit more in male fetuses than female ones. Upon the presence of the 5α-reductase enzyme, testosterone is converted to dihydrotestosterone (i.e. DHT). If DHT is present, the male external genitalia will develop.
Development of male external genitalia:
- Genital tubercle forms the penis[6]
- Urethral folds forms the urethra[6]
- Genital swelling forms the scrotum[6]
On the other hand, if maternal placenta estrogen is present without DHT, then the development of female external genitalia occurs.
Development of female external genitalia:
- Genital tubercle forms the clitoris[7]
- Urethral folds forms the labia minora[7]

Chemical structure of dihydrotestosterone (DHT) - Genital swelling forms the labia majora[7]
However, in abnormal cases, sexual anomalies occur due to a variety of factors that lead to an excess of androgens in the fetus. The effects of excessive androgens differ in fetuses with XX chromosome (female) and XY chromosomes (male).
In XX chromosome fetuses, excess androgens result in ambiguous genitalia. This makes identification of external genitalia as male or female difficult.[7] Additionally, the individual may have clitoromegaly, a shallow vagina, early and rapid growth of pubic hair in childhood, delayed puberty, hirsutism, virilisation, irregular menstrual cycle in adolescence and infertility due to anovulation.[8]
In XY chromosome fetuses, excess androgens result in a functional and average-sized penis with extreme virilisation, but the inability for sperm production.[9] Additionally, the individual will also experience early and rapid growth of pubic hair during childhood and precocious puberty stages.[8]
Classification
Differences/disorders of sexual development (DSD) are classified into different categories: chromosomal variation, gonadal development disorders, abnormal genital development and others.
Chromosomal variation

DSDs caused by chromosomal variation generally do not present with genital ambiguity. This includes sex chromosome DSDs such as Klinefelter syndrome, Turner syndrome and 45,X or 46,XY gonadal dysgenesis.[10]
Males with Klinefelter syndrome usually have a karyotype of 47,XXY as a result of having two or more X chromosomes.[11] Affected patients generally have normal genital development, yet are infertile and suffer from small, poor functioning testes, breast growth and delayed puberty.[11] The incidence for 47,XXY is 1 in 500 males, but severe and rare cases of Klinefelter syndrome presents as three or more X chromosomes.[11]
Turner syndrome is classified as aneuploidy or structural rearrangement of the X chromosome. Signs and symptoms of affected females vary among them, such as low birth weight, low-set ears, short stature, short neck and delayed puberty.[12] The incidence is 1 in 2500 live-born females, while most patients do not survive for more than one year after birth.[10]
Gonadal development disorders
Gonadal development disorders form a wide spectrum, classified by their cytogenetic and histopathological features. However, unsolved diagnosis and malignancy still represent difficulties in the sex determination of these patients.[13] Such disorders include partial or complete gonadal dysgenesis, ovotesticular DSD, testicular DSD and sex reversal.[3]
Abnormal genital development
Genital abnormality can occur in the penis, scrotum or testes in males; and vagina and labia in females.[3] Sometimes, ambiguous genitalia could occur, where the clear distinction of external genitalia is absent in both male and female. Hence, examination (typically at birth) is carried out where the sex of the patient will be determined through imaging and blood tests.[3] Abnormal genital development includes disorders of fetal origin, disorders in androgen synthesis or action, disorders in anti-Müllerian hormone synthesis or action.[3]
Others
In addition to the aforementioned sexual anomalies, there are other unclassified sexual anomalies. In males, this includes severe early-onset intrauterine growth restriction, isolated hypospadias, congenital hypogonadotropic hypogonadism, hypogonadism and cryptorchidism. In females, this includes Malformation syndromes, Müllerian agenesis/hypoplasia, uterine anomalies, vaginal atresia and labial adhesions.[3]
Causes
Sexual anomalies often generate from genetic abnormalities caused by many factors, leading to different sexual development. These genetic abnormalities occur during the prenatal stage of an individuals' fetal development. During this stage, genetic mutations can result from endocrine disrupters in the mother's diet or environmental factors.[14] The general causes of sexual anomalies can not be outlined due to the high variability of each individual's situations. Thus, the cause of each specific anomaly has to be studied independently.
Sexual differentiation occurs through various processes during the prenatal development period of the fetus. These processes are initiated and regulated by biological metabolites such as DNA, hormones and proteins. The initial steps of sexual differentiation begin with the development of the gonads and genitals. This process is consistent with both genders spanning over the course of the first 6 weeks following conception, during which the embryo remains pluripotent.[15] Differentiation of the gonads begins after the 6th week, which is determined by the sex-determining region Y (SRY) gene in the Y chromosome.[7]
The SRY gene plays an important role in developing the testes of a male individual. Following the development of the testes, hormones synthesized within the testes regulate the differentiation of both internal and external parts of the genitals. The absence of the testicles or the hormones synthesized may lead to irregular differentiation of the genitals. Genetic abnormalities or environmental factors that influence these procedures may lead to the incomplete development of the gonads and the genitals. These malformations can occur any time during the development or the birth of the embryo, manifesting as ambiguous genitals or dissonance within the genotypic and phenotypic sex of the individual, leading to a late onset of puberty, amenorrhea, a lack of or excess virilization, or later in life, infertility or early occurrence of menopause.[16]
Diagnosis and symptoms
First line diagnostic tests (prenatal)

Family history
- Symptoms such as infertility, early menopause, amenorrhea or sudden infant death syndrome (SIDS) could be a sign. Hence, an early check-up should be conducted.[3]
Analysis of karyotype
- Peripheral blood is collected for karyotyping. This helps classify the patient in one of the three main categories of DSD: chromosomal variation, gonadal development disorders and abnormal genital development.[3]
Abdominal ultrasounds
- The presence of gonads, uterus and vagina should be monitored. This can be done through abdominal ultrasounds. However, the absence of these sex organs will lead to difficulties in gender identification.[3]
Second line diagnostic tests (postnatal)
Physical Examination
- Inspection of the genitalia with care and palpation must be conducted with the following points in mind.[3]
- Determining the degree of virilization or masculinisation:
- In a female fetus, the Prader scale should be used to assess the extent of the virilisation if the karyotyping results are not out yet.[3]
- In males, the external masculinization score should be used.[3]
- Determining the degree of virilization or masculinisation:
- Palpation of gonads from the labioscrotal fold to the abdomen (inguinal canal).[3]
- Hydration and blood pressure assessment should be conducted.[3]
- Additional dysmorphic features should be ruled out because genitalia malformations would occur if the patient suffers from multiple malformation syndromes.[3]
Evaluation of hormones 48 hours after birth
- 17-Hydroxyprogesterone can be used to screen for congenital adrenal hyperplasia (CAH). This is commonly found in patients with 46, XX DSD.[3][17]
- Dehydroepiandrosterone (DHEA) in addition to progesterone allows for the diagnosis of more uncommon forms of CAH and other inherited disorders.[3]
- Base testosterone, follicle stimulating hormone (FSH) and luteinising hormone (LH) levels are precursors in individuals with 46,XX DSD. These tests are conducted within the timeframe of thirty hours post-birth to anywhere between fifteen and ninety days post-birth. This data collected within time frame can be used to gauge the growth of the fetus when it reaches six months of age.[3][17]
- Basal cortisol levels and adrenocorticotropic hormone (ACTH) is essential in diagnosing panhypopituitarism and enzymatic disorders affecting adrenal steroidogenesis.[3]
- The anti-Müllerian hormone is used for evaluating the function of Sertoli cells.[3]
- A urinary steroid profile shows the ratio of precursor metabolites within measured urine concentrations and the resultant products produced indicates the enzyme is the cause of a sexual defect. This is a more specific procedure in the detection of the defect in comparison to analysing blood.[3]
Treatment and management
The treatment and/or management of DSDs with atypical genitalia will vary from person to person. This may include gender assignment, medical treatment and surgical treatment.
Gender assignment
Gender assignment plays a critical role in the management of sexual anomaly cases. Ultimately, the parents and a multidisciplinary team are responsible for assigning the gender. The current guidelines of gender assignment include the psychosocial effects in adults with etiological diagnosis, the potential for fertility, surgical opportunities and hormone replacement therapy in the course of puberty.[5]
There are other factors considered during this process. This may include cultural and religious factors as well as the implications it has on the individual in later life. It is regulated by reference centers with groups specialised in managing cases of sexual anomalies.[5]
Medical treatment
Hormonal treatment is an accepted and standardised approach to treat different congenital sexual anomalies. Patients that are deficient in hormones produced by the adrenal glands require immediate medical attention. They are given a hormone called hydrocortisone, a form of hormone replacement therapy, with the objective to induce puberty.[5]
Utilizing sex steroids as hormonal therapy is deemed controversial with concerns of its duration of initiation, dosage and regimen.[5] However, it is agreed amongst most clinicians that low doses of hormonal treatment should begin around the age of 11 to 12 years old and should be increased progressively.[5]
Surgical treatment
Surgical procedures are an alternative to hormonal treatment available for patients to address genital anomalies and improve the body's sexual functions. However, a common dilemma in these procedures is that they are often derived from the patient's expectation of ‘normal’ genitals from an aesthetic and functional standpoint. Oftentimes, this leads to extensive surgical interventions.[18]
In most cases, surgical procedures result in permanent changes to the appearance and function of the patient's body. Therefore, the decision to proceed with this arrangement must be a joint agreement between the family and the multidisciplinary team. The most ideal situation would be to include the patient as part of the decision-making process. However, cases where surgical treatments were performed at an early age are recognised as mutilation of the body. Subsequently, it has become increasingly common to defer surgical treatments until the patient is of appropriate age to be involved in the decision-making process.[5]
Controversy and implications
Even though the term disorder of sex development (DSD) is widely accepted by the medical community, its suitability and adequacy to represent these individuals are criticised by many support and advocacy groups. Firstly, the word ‘disorder’ carries negative connotations. Secondly, with current nomenclature, DSD is an overly generalised term for conditions that do not have differences in genital appearance or gender identity (e.g. Klinefelter syndrome and Turner syndrome). Thirdly, the term ‘DSD’ lacks specificity and clarity; and therefore unhelpful in the diagnosis process. Hence, many support groups and advocates believe that the medical community should discontinue the use of ‘DSD’ as a designation tool.[19]
Furthermore, people who live with conditions regarding sexual abnormalities may encounter various mental and physical health problems. This may include traumatic experience with their own bodies, dissatisfaction with body image, low-self esteem, anxiety, depression, bipolar disorders, eating disorders, personality disorders, schizophrenia disorders, trauma and stress-related disorders, etc.[20]
See also
References
- ^ "Disorders of Sex Development Loci". 2017-01-01. doi:10.1016/B978-0-12-809633-8.06552-3.
{{cite journal}}: Cite journal requires|journal=(help) - ^ Achermann, John C.; Hughes, Ieuan A. (2016), "Pediatric Disorders of Sex Development", Williams Textbook of Endocrinology, Elsevier, pp. 893–963, doi:10.1016/b978-0-323-29738-7.00023-x, ISBN 978-0-323-29738-7, retrieved 2021-04-01
- ^ a b c d e f g h i j k l m n o p q r s t u Guerrero-Fernández, Julio; Azcona San Julián, Cristina; Barreiro Conde, Jesús; Bermúdez de la Vega, José Antonio; Carcavilla Urquí, Atilano; Castaño González, Luis Antonio; Martos Tello, José María; Rodríguez Estévez, Amaya; Yeste Fernández, Diego; Martínez Martínez, Leopoldo; Martínez-Urrutia, María José (2018). "Management guidelines for disorders/different sex development (DSD)". Anales de Pediatría (English Edition). 89 (5): 315.e1–315.e19. doi:10.1016/j.anpede.2018.06.006.
- ^ "Ambiguous genitalia - Diagnosis and treatment - Mayo Clinic". www.mayoclinic.org. Retrieved 2021-04-01.
- ^ a b c d e f g Deligdisch-Schor, Liane; Mareş Miceli, Angelica, eds. (2020). "Hormonal Pathology of the Uterus". Advances in Experimental Medicine and Biology: 133. doi:10.1007/978-3-030-38474-6. ISSN 0065-2598.
- ^ a b c Kinter, Kevin; Anekar, Aabha (2021-03-13). "Biochemistry, Dihydrotestosterone". StatPearls.
- ^ a b c d e A, Aatsha P.; Krishan, Kewal (2020-05-30). "Embryology, Sexual Development". StatPearls.
- ^ a b Momodu, Ifeanyi; Lee, Brian; Singh, Gurdeep (2021-02-05). "Congenital Adrenal Hyperplasia". StatPearls.
- ^ Witchel, Selma Feldman (April 2018). "Disorders of sex development". Best Practice & Research Clinical Obstetrics & Gynaecology. 48: 90–102. doi:10.1016/j.bpobgyn.2017.11.005. PMC 5866176. PMID 29503125.
- ^ a b Witchel, Selma Feldman (2018). "Disorders of sex development". Best Practice & Research Clinical Obstetrics & Gynaecology. 48: 90–102. doi:10.1016/j.bpobgyn.2017.11.005. PMC 5866176. PMID 29503125.
- ^ a b c "Klinefelter syndrome - Symptoms and causes". Mayo Clinic. Retrieved 2021-04-01.
- ^ Gravholt, Claus H; Andersen, Niels H; Conway, Gerard S; Dekkers, Olaf M; Geffner, Mitchell E; Klein, Karen O; Lin, Angela E; Mauras, Nelly; Quigley, Charmian A; Rubin, Karen; Sandberg, David E (2017). "Clinical practice guidelines for the care of girls and women with Turner syndrome: proceedings from the 2016 Cincinnati International Turner Syndrome Meeting". European Journal of Endocrinology. 177 (3): G1–G70. doi:10.1530/EJE-17-0430. ISSN 0804-4643.
- ^ Wolffenbuttel, K. P.; Hersmus, R.; Stoop, H.; Biermann, K.; Hoebeke, P.; Cools, M.; Looijenga, L. H. J. (2016-12-12). "Gonadal dysgenesis in disorders of sex development: Diagnosis and surgical management". Journal of Pediatric Urology. 12 (6): 411–416. doi:10.1016/j.jpurol.2016.08.015. ISSN 1873-4898. PMID 27769830.
- ^ Rogers, Kara (2016-12-05). "Endocrine disruptor | biochemistry". Encyclopedia Britannica. Retrieved 2021-04-13.
{{cite web}}: CS1 maint: url-status (link) - ^ Peinkofer, Gabriel; Burkert, Karsten; Urban, Katja; Krausgrill, Benjamin; Hescheler, Jürgen; Saric, Tomo; Halbach, Marcel (2016). "From Early Embryonic to Adult Stage: Comparative Study of Action Potentials of Native and Pluripotent Stem Cell-Derived Cardiomyocytes". Stem Cells and Development. 25 (19): 1397–1406. doi:10.1089/scd.2016.0073. ISSN 1547-3287.
- ^ Pal, AsokeK; Ambulkar, PrafullaS; Sontakke, BharatR; Talhar, ShwetaS; Bokariya, Pradeep; Gujar, VijayK (2019). "A study on chromosomal analysis of patients with primary amenorrhea". Journal of Human Reproductive Sciences. 12 (1): 29. doi:10.4103/jhrs.JHRS_125_17. ISSN 0974-1208. PMC 6472206. PMID 31007464.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Juniarto, A. Zulfa; van der Zwan, Yvonne G.; Santosa, Ardy; Ariani, Mahayu Dewi; Eggers, Stefanie; Hersmus, Remko; Themmen, Axel P.N.; Bruggenwirth, Hennie T.; Wolffenbuttel, Katja P.; Sinclair, Andrew; White, Stefan J. (2016). "Hormonal evaluation in relation to phenotype and genotype in 286 patients with a disorder of sex development from Indonesia". Clinical Endocrinology. 85 (2): 247–257. doi:10.1111/cen.13051.
- ^ Physiopedia contributors (2020-10-22). "Klinefelter Syndrome". Physiopedia. Retrieved 2021-04-11.
{{cite web}}:|last=has generic name (help)CS1 maint: url-status (link) - ^ Houk, Christopher P; Baskin, Laurence S; Levitsky, Lynne L (Jan 9, 2021). Geffner, Mitchell E; Hoppin, Alison G (eds.). "Management of the infant with atypical genitalia (disorder of sex development)". UpToDate. Retrieved April 9, 2021.
{{cite web}}: CS1 maint: url-status (link) - ^ "Supporting yourself - Intersex people". headtohealth.gov.au. 2019-09-24. Retrieved 2021-04-01.
{{cite web}}: CS1 maint: url-status (link)

