Probiotic: Difference between revisions
Undid revision 626010085 by 94.210.50.111 (talk) by my read, the abstracts do support the claim of vitamin production |
|||
| Line 57: | Line 57: | ||
Although research does suggests that the relationship between [[Gut flora]] and humans is a [[Mutualism (biology)|mutualistic]] relationship.<ref>{{cite journal |doi=10.1016/j.anaerobe.2005.05.001 |title=A dynamic partnership: Celebrating our gut flora |year=2005 |last1=Sears |first1=Cynthia L. |journal=Anaerobe |volume=11 |issue=5 |pages=247–51 |pmid=16701579}}</ref> There is very little evidence to support claims that probiotic [[dietary supplements]] have any health benefits.<ref name=snake>{{cite journal | author = Slashinski MJ, McCurdy SA, Achenbaum LS, Whitney SN, McGuire AL | title = "Snake-oil," "quack medicine," and "industrially cultured organisms:" biovalue and the commercialization of human microbiome research | journal = BMC Medical Ethics | volume = 13 | page = 28 | year = 2012 | pmid = 23110633 | pmc = 3512494 | doi = 10.1186/1472-6939-13-28 }}</ref> Improved health through [[Gut flora]] modulation appears to be directly related to long term dietary changes. <ref>{{cite journal |doi=10.1126/science.1208344 |title=Linking Long-Term Dietary Patterns with Gut Microbial Enterotypes |year=2011 |last1=Wu |first1=G. D. |last2=Chen |first2=J. |last3=Hoffmann |first3=C. |last4=Bittinger |first4=K. |last5=Chen |first5=Y.-Y. |last6=Keilbaugh |first6=S. A. |last7=Bewtra |first7=M. |last8=Knights |first8=D. |last9=Walters |first9=W. A. |last10=Knight |first10=R. |last11=Sinha |first11=R. |last12=Gilroy |first12=E. |last13=Gupta |first13=K. |last14=Baldassano |first14=R. |last15=Nessel |first15=L. |last16=Li |first16=H. |last17=Bushman |first17=F. D. |last18=Lewis |first18=J. D. |journal=Science |volume=334 |issue=6052 |pages=105–8 |pmid=21885731 |pmc=3368382}}</ref> |
Although research does suggests that the relationship between [[Gut flora]] and humans is a [[Mutualism (biology)|mutualistic]] relationship.<ref>{{cite journal |doi=10.1016/j.anaerobe.2005.05.001 |title=A dynamic partnership: Celebrating our gut flora |year=2005 |last1=Sears |first1=Cynthia L. |journal=Anaerobe |volume=11 |issue=5 |pages=247–51 |pmid=16701579}}</ref> There is very little evidence to support claims that probiotic [[dietary supplements]] have any health benefits.<ref name=snake>{{cite journal | author = Slashinski MJ, McCurdy SA, Achenbaum LS, Whitney SN, McGuire AL | title = "Snake-oil," "quack medicine," and "industrially cultured organisms:" biovalue and the commercialization of human microbiome research | journal = BMC Medical Ethics | volume = 13 | page = 28 | year = 2012 | pmid = 23110633 | pmc = 3512494 | doi = 10.1186/1472-6939-13-28 }}</ref> Improved health through [[Gut flora]] modulation appears to be directly related to long term dietary changes. <ref>{{cite journal |doi=10.1126/science.1208344 |title=Linking Long-Term Dietary Patterns with Gut Microbial Enterotypes |year=2011 |last1=Wu |first1=G. D. |last2=Chen |first2=J. |last3=Hoffmann |first3=C. |last4=Bittinger |first4=K. |last5=Chen |first5=Y.-Y. |last6=Keilbaugh |first6=S. A. |last7=Bewtra |first7=M. |last8=Knights |first8=D. |last9=Walters |first9=W. A. |last10=Knight |first10=R. |last11=Sinha |first11=R. |last12=Gilroy |first12=E. |last13=Gupta |first13=K. |last14=Baldassano |first14=R. |last15=Nessel |first15=L. |last16=Li |first16=H. |last17=Bushman |first17=F. D. |last18=Lewis |first18=J. D. |journal=Science |volume=334 |issue=6052 |pages=105–8 |pmid=21885731 |pmc=3368382}}</ref> |
||
In a 2009 blog post, one expert reasoned that preliminary clinical results exist for some applications, such as treating diarrhea, but wider health benefits claimed by probiotic proponents lack plausibility since the body's "ecosystem" is sufficiently complex that adding a few bacteria is unlikely to have the claimed effect. Accordingly, he reasoned, "the alleged health benefits of probiotics are often an example of spin".<ref name="sbm">{{cite web|url=http://www.sciencebasedmedicine.org/probiotics/|title=Probiotics|last1=Crislip|first=Mark|authorlink=Mark Crislip|date=16 January 2009|publisher=Science-based Medicine|accessdate=8 October 2013}}</ref>. Since then, there has been an increase in the body of scientific evidence supporting the use of specific probiotics to improve health (See table on [[Probiotic#Strains|Probiotic strains]] section). Although the body's complex microbial community is incompletely understood at present, there is strong scientific consensus on the benefits of using of probiotics to address certain medical states or conditions <ref>{{cite journal | author = Colin Hill, Francisco Guarner, Gregor Reid, Glenn R. Gibson, Daniel J. Merenstein, Bruno Pot, Lorenzo Morelli, Roberto Berni Canani, Harry J. Flint, Seppo Salminen, Philip C. Calder, Mary Ellen Sanders | title = Expert consensus document: The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic | journal = Nature Reviews Gastroenterology and Hepatology | volume = 11 | issue = 8 | pages = 506-514 | year = 2014 | doi = 10.1038/nrgastro.2014.66 }} </ref>. |
|||
===Allergies=== |
===Allergies=== |
||
Revision as of 11:14, 25 September 2014
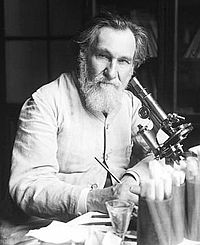
Probiotics are microorganisms that provide health benefits when consumed, as claimed by some.[1] The term probiotic is currently used to name ingested microorganisms associated with beneficial effects to humans and animals.[2] Introduction of the concept is generally attributed to Nobel Prize recipient Eli Metchnikoff, who in 1907 suggested that "the dependence of the intestinal microbes on the food makes it possible to adopt measures to modify the flora in our bodies and to replace the harmful microbes by useful microbes".[3] A significant expansion of the potential market for probiotics has led to higher requirements for scientific substantiation of putative beneficial effects conferred by the microorganisms.
Etymology
Some literature gives it a full Greek etymology,[4][5] but the term appears to be a composite of the Latin preposition pro ("for") and the Greek adjective βιωτικός (biotic), the latter deriving from the noun βίος (bios, "life").[6]
Definition
The World Health Organization's 2001 definition of probiotics is "live micro-organisms which, when administered in adequate amounts, confer a health benefit on the host".[7] Following this definition, a working group convened by the FAO/WHO in May 2002 issued the “Guidelines for the Evaluation of Probiotics in Food”. This first global effort was further developed in 2010, two expert groups of academic scientists and industry representatives made recommendations for the evaluation and validation of probiotic health claim.[8][9] The same principles emerged from those groups as the ones expressed in the Guidelines of FAO/WHO in 2002. This definition, although widely adopted, is not acceptable to the European Food Safety Authority because it embeds a health claim which is not measurable.[1]
A consensus definition of the term “probiotics”, based on the available information and scientific evidence, was adopted after a joint Food and Agricultural Organization of the United Nations and World Health Organization expert consultation. In October 2001, this expert consultation defined probiotics as: “live micro-organisms which, when administered in adequate amounts, confer a health benefit on the host”.[2] The FAO/WHO consultation was also a first effort towards the assessment of probiotics efficacy and resulted in May 2002 in a document named “Guidelines for the Evaluation of Probiotics in Food”.[10] This effort is accompanied by local governmental and supra-governmental regulatory bodies requirements to better characterize health claims substantiations.
Probiotics have to be alive when administered.[11][12][13] One of the concerns throughout the scientific literature resides in the viability and reproducibility on a large scale of the observed results, as well as the viability and stability during use and storage and finally the ability to survive in the intestinal ecosystem.[14] Probiotics must have undergone controlled evaluation to document health benefits in the target host. Only products containing live organisms shown in reproducible human studies to confer a health benefit can actually claim to be a probiotic.[15][16][17] The correct definition of health benefit, backed with solid scientific evidence, is a strong element for the proper identification and assessment of the effect of a probiotic. This aspect represents a major challenge for scientific and industrial investigations because several difficulties arise, such as variability in the site for probiotic use (oral, vaginal, intestinal) and mode of application.[11]
The probiotic candidate must be a taxonomically defined microbe or combination of microbes (genus, species and strain level). It is commonly admitted that most effects of probiotic are strain-specific and cannot be extended to other probiotics of the same genus or species.[12] This calls for a precise identification of the strain, i.e. genotypic and phenotypic characterization of the tested microorganism.[8]
Probiotics must be safe for their intended use. The 2002 FAO/WHO guidelines recommend that, though bacteria may be Generally Recognized as Safe (GRAS), the safety of the potential probiotic should be assessed by the minimum required tests:[citation needed]
- Determination of antibiotic resistance patterns
- Assessment of certain metabolic activities (e.g., D-lactate production, bile salt deconjugation)
- Assessment of side-effects during human studies
- Epidemiological surveillance of adverse incidents in consumers (post-market)
- If the strain under evaluation belongs to a species that is a known mammalian toxin producer, it must be tested for toxin production. One possible scheme for testing toxin production has been recommended by the EU Scientific Committee on Animal Nutrition (SCAN, 2000)
- If the strain under evaluation belongs to a species with known hemolytic potential, determination of hemolytic activity is required
In Europe, EFSA has adopted a pre-market system for safety assessment of microbial species used in food and feed productions, in order to set priorities for the need of risk assessment. The assessment is made for a selected group of microorganisms, which if favorable, leads to the “Qualified Presumption of Safety” (QPS) status.[18]
Finally probiotics have to be supplied in adequate amounts which may be defined as the amount able to trigger the targeted effect on the host.[citation needed] It depends on strain specificity, process and matrix, as well as the targeted effect. Most of reported benefits demonstrated with the traditional probiotics have been observed after ingestion of a concentration around 107 to 108 probiotics per gram, with serving size around 100 to 200 mg per day.[8][failed verification]
History
Probiotics have received renewed attention recently from product manufacturers, research studies and consumers. The history of probiotics can be traced back to the first use of cheese and fermented products, that were well known to the Greeks and Romans who recommended their consumption.[19] The fermentation of dairy foods represents one of the oldest techniques for food preservation.[20]
The original modern hypothesis of the positive role played by certain bacteria was first introduced by Russian scientist and Nobel laureate Élie Metchnikoff, who in 1907 suggested that it would be possible to modify the gut flora and to replace harmful microbes with useful microbes.[21] Metchnikoff, at that time a professor at the Pasteur Institute in Paris, proposed the hypothesis that the aging process results from the activity of putrefactive (proteolytic) microbes producing toxic substances in the large bowel. Proteolytic bacteria such as clostridia, which are part of the normal gut flora, produce toxic substances including phenols, indols and ammonia from the digestion of proteins. According to Metchnikoff these compounds were responsible for what he called "intestinal auto-intoxication", which would cause the physical changes associated with old age.[22]
It was at that time known that milk fermented with lactic-acid bacteria inhibits the growth of proteolytic bacteria because of the low pH produced by the fermentation of lactose. Metchnikoff had also observed that certain rural populations in Europe, for example in Bulgaria and the Russian steppes who lived largely on milk fermented by lactic-acid bacteria were exceptionally long lived. Based on these observations, Metchnikoff proposed that consumption of fermented milk would "seed" the intestine with harmless lactic-acid bacteria and decrease the intestinal pH and that this would suppress the growth of proteolytic bacteria. Metchnikoff himself introduced in his diet sour milk fermented with the bacteria he called "Bulgarian Bacillus" and found his health benefited. Friends in Paris soon followed his example and physicians began prescribing the sour milk diet for their patients.[23]
Bifidobacteria were first isolated from a breast-fed infant by Henry Tissier who also worked at the Pasteur Institute. The isolated bacterium named Bacillus bifidus communis[24] was later renamed to the genus Bifidobacterium. Tissier found that bifidobacteria are dominant in the gut flora of breast-fed babies and he observed clinical benefits from treating diarrhea in infants with bifidobacteria. The claimed effect was bifidobacterial displacement of proteolytic bacteria causing the disease.[citation needed]
During an outbreak of shigellosis in 1917, German professor Alfred Nissle isolated a strain of Escherichia coli from the feces of a soldier who was not affected by the disease.[25] Methods of treating infectious diseases were needed at that time when antibiotics were not yet available, and Nissle used the Escherichia coli Nissle 1917 strain in acute gastrointestinal infectious salmonellosis and shigellosis.[citation needed]
In 1920, Rettger and Cheplin reported that Metchnikoff's "Bulgarian Bacillus", later called Lactobacillus delbrueckii subsp. bulgaricus, could not live in the human intestine.[26] They conducted experiments involving rats and humans volunteers, by feeding them with Lactobacilus acidophilus. They observed changes in composition of fecal microbiota, which they described as “transformation of the intestinal flora”.[26] Rettger further explored the possibilities of Lactobacilus acidophilus and reasoned that bacteria originating from the gut were more likely to produce the desired effect in this environment. In 1935 certain strains of Lactobacillus acidophilus were found to be very active when implanted in the human digestive tract.[27] Trials were carried out using this organism, and encouraging results were obtained especially in the relief of chronic constipation.[citation needed]
According to Hamilton-Miller et al., in a letter in which they call for the oldest known citation of the word, the term "probiotics" was first introduced in 1953 by Werner Kollath (see Hamilton-Miller et al. 2003) to describe organic and inorganic food supplements applied to restore health to patients suffering from manlnutrition. Contrasting antibiotics, probiotics were defined as microbially derived factors that stimulate the growth of other microorganisms. In 1989, Roy Fuller suggested a definition of probiotics that has been widely used: "A live microbial feed supplement which beneficially affects the host animal by improving its intestinal microbial balance".[11] Fuller's definition emphasizes the requirement of viability for probiotics and introduces the aspect of a beneficial effect on the host.[citation needed]
The term "probiotic" originally referred to microorganisms that have effects on other microorganisms, a usage credited to Lilly and Stilwell (1965).[28] Their conception of probiotics involved the notion that substances secreted by one microorganism stimulated the growth of another microorganism. The term was used again in 1971 by Sperti [29] to describe tissue extracts which stimulated microbial growth. The term probiotics was taken up by Parker in 1974 [30] who defined the concept as, “organisms and substances that have a beneficial effect on the host animal by contributing to its intestinal microbial balance”. Later, the definition was greatly improved by Fuller in 1989,[11] whose explanation was very close to the definition used today. Fuller in 1989 described probiotics as a "live microbial feed supplement which beneficially affects the host animal by improving its intestinal microbial balance". He stressed two important facts of probiotics: the viable nature of probiotics and the capacity to help with intestinal balance.
In the following decades, intestinal lactic acid bacterial species with alleged health beneficial properties have been introduced as probiotics, including Lactobacillus rhamnosus, Lactobacillus casei, and Lactobacillus johnsonii.[31]
Research
Probiotics are under considerable research, as the concept holds promise for human health and well-being, and corresponding commercial opportunities. Protection of consumers requires health claims to be confirmed with sufficient scientific evidence. Overall scientific demonstration of probiotic effects requires defining a healthy microbiota and interactions between microbiota and host, and the difficulty to characterize probiotic effectiveness in health and disease. Recent developments of high-throughput sequencing technology and the consequent progresses of metagenomics represent a new approach for the future of probiotics research.[32]
Studies are examining whether probiotics affect mechanisms of intestinal inflammation,[33] diarrhea,[34] urogenital infections[35] or allergies.[36] Through 2012, however, in all cases proposed as health claims to the European Food Safety Authority, the scientific evidence remains insufficient to prove a cause and effect relationship between consumption of probiotic products and any health benefit.[37]
Research into the potential health effects of supplemental probiotics has included the molecular biology and genomics of Lactobacillus in immune function, cancer, and antibiotic-associated diarrhea, travellers' diarrhea, pediatric diarrhea, inflammatory bowel disease and irritable bowel syndrome.[38] Testing of a probiotic applies to a specific strain under study.[39] The scientific community cautions against extrapolating an effect from a tested strain to an untested strain.[40][41]
Although research does suggests that the relationship between Gut flora and humans is a mutualistic relationship.[42] There is very little evidence to support claims that probiotic dietary supplements have any health benefits.[43] Improved health through Gut flora modulation appears to be directly related to long term dietary changes. [44]
In a 2009 blog post, one expert reasoned that preliminary clinical results exist for some applications, such as treating diarrhea, but wider health benefits claimed by probiotic proponents lack plausibility since the body's "ecosystem" is sufficiently complex that adding a few bacteria is unlikely to have the claimed effect. Accordingly, he reasoned, "the alleged health benefits of probiotics are often an example of spin".[45]. Since then, there has been an increase in the body of scientific evidence supporting the use of specific probiotics to improve health (See table on Probiotic strains section). Although the body's complex microbial community is incompletely understood at present, there is strong scientific consensus on the benefits of using of probiotics to address certain medical states or conditions [46].
Allergies
A 2013 meta-analysis of 25 trials found that probiotic supplementation in pregnancy and early life might help with atopic sensitivity in infants but probably not with asthma or wheezing.[47]
Diarrhea
Some probiotics have been shown in preliminary research to possibly treat various forms of gastroenteritis.[48] A Cochrane Collaboration systematic review of the use of probiotics to treat acute infectious diarrhoea found encouraging results, but said further research was necessary to confirm the reported benefits.[49][50]
- Antibiotic-associated diarrhea
Some of the best evidence in support of probiotic health benefits is in the treatment of Antibiotic-associated diarrhea (AAD).[45] Antibiotics are a common treatment for children, and 20% of antibiotic-treated children develop diarrhea. AAD results from an imbalance in the colonic microbiota caused by antibiotic therapy. Microbiota alteration changes carbohydrate metabolism with decreased short-chain fatty acid absorption and an osmotic diarrhea as a result. The preventive role of some probiotics has been correctly assessed in randomly clinical trials. A review, assessing the work of 16 different studies representing more than 3400 patients’ evaluation, concluded that the evidence gathered suggested a protective effect of some probiotics in this condition.[51][52] In adults, some probiotics showed a beneficial role in reducing the occurrence of antibiotic associated diarrhea.[53] Another consequence of antibiotic therapy leading to diarrhea is overgrowth of potentially pathogenic organisms such as Clostridium difficile.[54]
Probiotic treatment might reduce the incidence and severity of AAD as indicated in several meta-analyses.[55] For example, treatment with probiotic formulations including Lactobacillus rhamnosus may reduce the risk of antibiotic-associated diarrhea, improve stool consistency during antibiotic therapy, and enhance the immune response after vaccination.[56] However, further documentation of these findings through randomized, double blind, placebo-controlled trials is required to confirm specific effects and obtain regulatory approval, which currently does not exist.
Potential efficacy of probiotic AAD prevention is dependent on the probiotic strain(s) used and on the dosage.[57][58] A Cochrane Collaboration systematic review, in which 16 randomized clinical trials (n=3432 participants) were analyzed, concluded that treatments with less than 5000 million of CFU/day did not show a significant decrease of AAD. On the other hand, patients treated with ≥5000 million of CFU/day (including Lactobacillus rhamnosus and Saccharomyces boulardii) had 60% lower relative risk (95%CI: 44%-71%) of experiencing AAD than non-treated patients.[51]
Lactose intolerance
Ingestion of certain active strains may help lactose-intolerant individuals tolerate more lactose than they would otherwise have tolerated.[59]
Cholesterol
Preliminary human and animal studies have demonstrated the efficacy of some strains of lactic acid bacteria for reducing serum cholesterol levels, presumably by breaking down bile in the gut, thus inhibiting its reabsorption (where it enters the blood as cholesterol).[59][60]
A meta-analysis that included five double blind trials examining the short term (2–8 weeks) effects of a yogurt with probiotic strains on serum cholesterol levels found a minor change of 8.5 mg/dL (0.22 mmol/L) (~4% decrease) in total cholesterol concentration, and a decrease of 7.7 mg/dL (0.2 mmol/L) (~5% decrease) in serum LDL concentration.[61]
A slightly longer study evaluating the effect of a yogurt with probiotic strains on twenty-nine subjects over six months found no statistically significant differences in total serum cholesterol or LDL values. However, the study did note a significant increase in serum HDL from, 50 mg/dL (1.28 mmol/L) to 62 mg/dL (1.6 mmol/L) following treatment. This corresponds to a possible improvement of LDL/HDL ratio.[62]
Studies specifically on hyper-lipidemic subjects are still needed.
Blood pressure
Some studies have indicated that consumption of milk fermented with various strains of LAB may result in modest reductions in blood pressure, an effect possibly related to the ACE inhibitor-like peptides produced during fermentation.[59]
Immune function and infections
Some strains of LAB may affect pathogens by means of competitive inhibition (i.e., by competing for growth) and there is evidence to suggest that they may improve immune function by increasing the number of IgA-producing plasma cells, increasing or improving phagocytosis as well as increasing the proportion of T lymphocytes and Natural Killer cells.[63][64] Clinical trials have demonstrated that probiotics may decrease the incidence of respiratory tract infections[65] and dental caries in children.[66] LAB products might aid in the treatment of acute diarrhea, and possibly affect rotavirus infections in children and travelers' diarrhea in adults,[63][64] but no products are approved for such indications.
A 2010 study suggested that probiotics, by introducing "good" bacteria into the gut, may help maintain immune system activity, which in turn helps the body react more quickly to new infections. Antibiotics seem to reduce immune system activity as a result of killing off the normal gut bacteria.[67]
Helicobacter pylori
Some strains of LAB may affect Helicobacter pylori infections (which may cause peptic ulcers) in adults when used in combination with standard medical treatments, but there is no standard in medical practice or regulatory approval for such treatment.[68]
Inflammation
Some strains of LAB may modulate inflammatory and hypersensitivity responses, an observation thought to be at least in part due to the regulation of cytokine function.[63] Clinical studies suggest that they can prevent reoccurrences of inflammatory bowel disease in adults,[63] as well as improve milk allergies.[69] They are not effective for treating eczema, a persistent skin inflammation.[70] How probiotics may influence the immune system remains unclear, but a potential mechanism under research concerns the response of T lymphocytes to pro-inflammatory stimuli.[71]
Bacterial growth under stress
In a study done to see the effects of stress on intestinal flora, rats that were fed probiotics had little occurrence of harmful bacteria adhering to their intestines compared to rats that were fed sterile water.[72]
Irritable bowel syndrome and colitis
There is some evidence probiotics may help people with irritable bowel syndrome, although uncertainty remains around which type of priobiotic works best, and around the size of the effect.[73]
There is no good evidence taking probiotics helps maintain remission from ulcerative colitis.[74]
Necrotizing enterocolitis (NEC)
Several clinical studies provide evidence for the potential of probiotics to lower the risk of NEC and mortality in premature infants. One meta-analysis indicated that probiotics reduce all-cause mortality and risk of having NEC by more than 50% compared with controls.[75]
Vitamin production
Probiotics synthesize vitamins. For example, they produce vitamin K,[76] folic acid,[77] and vitamin B12.[78]
Eczema
In 2003, researchers found that a combination of L rhamnosus 19070-2 and L reuteri DSM 122460 was beneficial in the management of Atopic Dermatitis. The effect was more pronounced in patients with increased IgE levels.[79] In 14 trials, most done between 2007 and 2011, researchers found a roughly 20% reduction in the rate of atopic dermatitis (from around 34% in the children in these trials to 26%).[80]
Bacterial Vaginosis
In 2013, researchers found that administration of hydrogen peroxide producing strains, such as L. acidophilus and L. rhamnosus, were able to normalize vaginal pH and re-balance vaginal flora, preventing and alleviating bacterial vaginosis.[81]
Other
Current research is focusing on the molecular biology and genomics of Lactobacillus strains and bifidobacteria. The application of modern whole genome approaches is providing insights into bifidobacterial evolution, while also revealing genetic functions that may explain their presence in the particular ecological environment of the gastrointestinal tract.[82][83]
Side effects
In some situations, such as where the person consuming probiotics is critically ill, probiotics could be harmful. In a therapeutic clinical trial conducted by the Dutch Pancreatitis Study Group, the consumption of a mixture of six probiotic bacteria increased the death rate of patients with predicted severe acute pancreatitis.[84]
In a clinical trial conducted at the University of Western Australia, aimed at showing the effectiveness of probiotics in reducing childhood allergies, researchers gave 178 children either a probiotic or a placebo for the first six months of their life. Those given the probiotic were more likely to develop a sensitivity to allergens.[85]
Some hospitals have reported treating lactobacillus septicaemia, which is a potentially fatal disease caused by the consumption of probiotics by people with lowered immune systems or who are already very ill.[85][86][unreliable medical source?]
Probiotics taken orally can be destroyed by the acidic conditions of the stomach. A number of micro-encapsulation techniques are being developed to address this problem.[87]
One 2009 study causally linked probiotic products such as yogurts with obesity trends.[88] However, this is contested as the link to obesity, and other health related issues with yogurt may link to its dairy and calorie attributes.[89][90]
Some experts are skeptical on the efficacy of many strains and believe not all subjects will benefit from the use of probiotics.[91]
Strains
Live probiotic cultures are available in fermented dairy products and probiotic fortified foods. However, tablets, capsules, powders and sachets containing the bacteria in freeze dried form are also available.
Only preliminary evidence exists for most probiotic health claims. Even of the most researched strains, few have been sufficiently developed in basic and clinical research to warrant approval for health claim status to a regulatory agency such as the Food and Drug Administration or European Food Safety Authority, and to date no claims have been approved by those two agencies.
| Probiotic Research[92] | |||
|---|---|---|---|
| Strain | Claimed potential effect in humans | ||
| Bacillus coagulans GBI-30, 6086 | May improve abdominal pain and bloating in IBS patients.[93] May increase immune response to a viral challenge.[94] | ||
| Bifidobacterium longum subsp. infantis 35624 | Possible relief from abdominal pain/discomfort, bloating and constipation.[95] | ||
| Lactobacillus acidophilus NCFM | Shown in one study to reduce the side effects of antibiotic therapy.[96] | ||
| Lactobacillus paracasei St11 (or NCC2461) | One study indicated reduction of diarrhea in children[97] | ||
| Lactobacillus johnsonii La1 (= Lactobacillus LC1, Lactobacillus johnsonii NCC533) | May reduce incidence of H. pylori-caused gastritis and may reduce inflammation [98] | ||
| Lactobacillus plantarum 299v | May affect symptoms of IBS.[99] | ||
| Lactobacillus reuteri ATCC 55730 (Lactobacillus reuteri SD2112) | Evidence for diarrhea mitigation in children,[100][101] decreased crying in infantile colic,[102] H. pylori infection,[103] antibiotic-associated side-effects,[104][105] fever and diarrhea in children[106] and number of sick days in adults.[107] | ||
| Lactobacillus reuteri Protectis (DSM 17938, daughter strain of ATCC 55730)[108] | Evidence for shortened duration of diarrhea in children,[109] decreased crying in infantile colic,[110][111] reduced risk of diarrhea in children,[112] may affect constipation [113] and functional abdominal pain in children.[114] | ||
| Lactobacillus reuteri Prodentis (DSM 17938/ATCC 55730 and ATCC PTA 5289 in combination) for oral health | Evidence for effect on gingivitis and periodontitis,[115][116][117][118] preliminary evidence for reduction of oral malodor,[119] evidence for reduction of risk factors for caries [120][121][122] | ||
| Saccharomyces boulardii | Evidence for inhibition of antibiotic-associated diarrhea[123] and acute diarrhea.[124][125] | ||
| tested as mixture: Lactobacillus rhamnosus GR-1® & Lactobacillus reuteri RC-14® |
In one study, oral ingestion resulted in vaginal colonisation and reduced vaginitis.[126] | ||
| tested as mixture: Lactobacillus acidophilus CL1285 & Lactobacillus casei LBC80R |
May affect digestive health.[127] In vitro inhibition of Listeria monocytogenes and L. innocua, Escherichia coli, Staphylococcus aureus, Enterococcus faecalis and Enterococcus faecium.[128] | ||
| Lactobacillus plantarum HEAL 9 & Lactobacillus paracasei 8700:2 | Under study for common cold infections.[130] | ||
Some additional forms of lactic acid bacteria include:
- Lactobacillus bulgaricus
- Streptococcus thermophilus
- "Lactobacillus bifidus" - became new genus Bifidobacterium
Some fermented products containing similar lactic acid bacteria include:
- Pickled vegetables[131][132][133][134]
- Fermented bean paste such as tempeh,[135] miso and doenjang
- Kefir[136]
- Buttermilk or Karnemelk[137]
- Kimchi [132][138]
- Pao cai[134][139]
- Sauerkraut[140]
- Soy sauce[141]
- Zha cai[134]
EFSA scientific review of probiotics
The European Food Safety Authority has so far rejected 260 claims[142] on probiotics in Europe due to insufficient research and thus inconclusive proof. The review did not refute the potential for effectiveness, but rather that a cause-effect relationship had not been sufficiently established in studies to date. The claims rejected include:
- Lactobacillus paracasei LMG P 22043 decreases potentially pathogenic gastro-intestinal microorganisms or reduce gastro-intestinal discomfort.
- Lactobacillus johnsonii BFE 6128 . Immunity and skin claims (all too general for consideration).
- Lactobacillus fermentum ME-3 decreases potentially pathogenic gastro-intestinal microorganisms.
- Lactobacillus plantarum BFE 1685. Immunity claim (deemed too general).
- Bifidobacterium longum BB536 improves bowel regularity; resists cedar pollen allergens; decreases pathogens.
- Lactobacillus plantarum 299v reduces flatulence and bloating and protects DNA, proteins and lipids from oxidative damage.
- Lactobacillus rhamnosus LB21 NCIMB 40564 helps maintain individual intestinal microbiota in subjects receiving antibiotic treatment.[143]
Multi-probiotic
Preliminary research is evaluating the potential physiological effects of multiple probiotic strains, as opposed to a single strain.[144][145] As the human gut may contain several hundred microbe species, one theory indicates that this diverse environment may benefit from consuming multiple probiotic strains, an effect that remains scientifically unconfirmed.
See also
- Fecal bacteriotherapy
- Microbial food cultures
- Prebiotic (nutrition)
- Synbiotics
- Probiotics in pediatrics
References
- ^ a b Rijkers GT, de Vos WM, Brummer RJ, Morelli L, Corthier G, Marteau P (2011). "Health benefits and health claims of probiotics: Bridging science and marketing". British Journal of Nutrition. 106 (9): 1291–6. doi:10.1017/S000711451100287X. PMID 21861940.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b http://www.who.int/foodsafety/publications/fs_management/en/probiotics.pdf Health and Nutritional Properties of Probiotics in Food including Powder Milk with Live Lactic Acid Bacteria
- ^ Metchnikoff, E. 1907. Essais optimistes. Paris. The prolongation of life. Optimistic studies. Translated and edited by P. Chalmers Mitchell. London: Heinemann, 1907
- ^ Fuller, R., ed. (1992) Probioiics. The Scieniific Basis. Chapman & Hall, London, U.K
- ^ Alvarez-Olmos MI, Oberhelman RA (2001). "Probiotic agents and infectious diseases: a modern perspective on a traditional therapy". Clin. Infect. Dis. 32 (11): 1567–76. doi:10.1086/320518. PMID 11340528.
- ^ Hamilton-Miller JM, Gibson GR, Bruck W (October 2003). "Some insights into the derivation and early uses of the word 'probiotic'". Br. J. Nutr. 90 (4): 845. doi:10.1079/BJN2003954. PMID 14552330.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Schlundt, Jorgen. "Health and Nutritional Properties of Probiotics in Food including Powder Milk with Live Lactic Acid Bacteria" (PDF). Report of a Joint FAO/WHO Expert Consultation on Evaluation of Health and Nutritional Properties of Probiotics in Food Including Powder Milk with Live Lactic Acid Bacteria. FAO / WHO. Retrieved 17 December 2012.
- ^ a b c Rijkers GT, Bengmark S, Enck P, Haller D, Herz U, Kalliomaki M, Kudo S, Lenoir-Wijnkoop I, Mercenier A, Myllyluoma E, Rabot S, Rafter J, Szajewska H, Watzl B, Wells J, Wolvers D, Antoine JM (2010). "Guidance for substantiating the evidence for beneficial effects of probiotics: current status and recommendations for future research". J. Nutr. 140 (3): 671S–6S. doi:10.3945/jn.109.113779. PMID 20130080.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Shane AL, Cabana MD, Vidry S, Merenstein D, Hummelen R, Ellis CL, Heimbach JT, Hempel S, Lynch SV, Sanders ME et al.: Guide to designing, conducting, publishing and communicating results of clinical studies involving probiotic applications in human participants. Gut Microbes 2010, 1:243-253
- ^ ftp://ftp.fao.org/es/esn/food/wgreport2.pdf Guidelines for the Evaluation of Probiotics in Food
- ^ a b c d Fuller R (May 1989). "Probiotics in man and animals". The Journal of Applied Bacteriology. 66 (5): 365–78. doi:10.1111/j.1365-2672.1989.tb05105.x. PMID 2666378.[non-primary source needed]
- ^ a b Fuller R. Probiotics in human medicine. Gut 1991;32:439–42
- ^ Fuller R. Probiotics the Scientific Thesis. London: Chapman & Hall, 1992
- ^ Review of probiotics available to modify gastrointestinal flora, Gismondo, 1999
- ^ Quigley EMM: The future of probiotics. In Probiotics in Pediatric Medicine. Edited by Michail S, Sherman P. Totowa, NJ: Humana Press; 2008:323-329
- ^ Reid G, Gaudier E, Guarner F, Huffnagle GB, Macklaim JM, Munoz AM, Martini M, Ringel-Kulka T, Sartor B, Unal R, Verbeke K, Walter J (2010). "Responders and non-responders to probiotic interventions: how can we improve the odds?". Gut Microbes. 1 (3): 200–4. doi:10.4161/gmic.1.3.12013. PMC 3023600. PMID 21637034.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ O'Hara AM, O'Regan P, Fanning A, O'Mahony C, Macsharry J, Lyons A, Bienenstock J, O'Mahony L, Shanahan F (2006). "Functional modulation of human intestinal epithelial cell responses by Bifidobacterium infantis and Lactobacillus salivarius". Immunology. 118 (2): 202–15. doi:10.1111/j.1365-2567.2006.02358.x. PMC 1782284. PMID 16771855.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.efsa.europa.eu/de/scdocs/doc/587.pdf Introduction of a Qualified Presum ption of Safety (QPS) approach for assessment of selected microorganisms referred to EFSA
- ^ Gismondo MR, Drago L, Lombardi A (1999). "Review of probiotics available to modify gastrointestinal flora". Int. J. Antimicrob. Agents. 12 (4): 287–92. doi:10.1016/s0924-8579(99)00050-3. PMID 10493604.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Azizpour K, Bahrambeygi S, Mahmoodpour S (2009). "History and Basic of Probiotics". Research Journal of Biological Sciences. 4 (4): 409–426.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Metchnikoff, E. 1907. Essais optimistes. Paris. The prolongation of life. Optimistic studies. Translated and edited by P. Chalmers Mitchell. London: Heinemann, 1907.
- ^ Arteriosclerosis and intestinal poisons. [a contemporary review of Metchnikoff's work] JAMA 1910, 55:2311-12.
- ^ Vaughan RB (July 1965). "The romantic rationalist: A study of Elie Metchnikoff". Medical History. 9 (3): 201–15. doi:10.1017/S0025727300030702. PMC 1033501. PMID 14321564.
- ^ Tissier, H. 1900. Recherchers sur la flora intestinale normale et pathologique du nourisson. Thesis, University of Paris, Paris, France.
- ^ Die antagonistische Behandlung chronischer Darmstörungen mit Colibakterien (1918). Med Klin. 2: 29–30.
{{cite journal}}: Missing or empty|title=(help) - ^ a b Cheplin HA, Rettger LF (December 1920). "Studies on the Transformation of the Intestinal Flora, with Special Reference to the Implantation of Bacillus Acidophilus: II. Feeding Experiments on Man". Proceedings of the National Academy of Sciences of the United States of America. 6 (12): 704–5. Bibcode:1920PNAS....6..704C. doi:10.1073/pnas.6.12.704. PMC 1084701. PMID 16576567.[non-primary source needed]
- ^ Rettger, L.F., W.N. Levy, L. Weinstein, and J.E. Weiss. 1935. Lactobacillus acidophilus and its therapeutic application. Yale University Press, New Haven.[non-primary source needed]
- ^ Lilly DM, Stillwell RH (1965). "Probiotics: Growth-promoting factors produced by microorganisms". Science. 147 (3659). New York, N.Y.: 747–748. Bibcode:1965Sci...147..747L. doi:10.1126/science.147.3659.747. PMID 14242024.
- ^ Sperti, G. S. (1971). Probiotics. West Point, CT: AVI Publishing Co. ISBN 0870550993.
- ^ Parker, R. B. (1974). "Probiotics, the other half of the antibiotic story". Animal Nutrition and Health. 29: 4–8.
- ^ Tannock GW (September 2003). "Probiotics: time for a dose of realism". Current Issues in Intestinal Microbiology. 4 (2): 33–42. PMID 14503687.
- ^ Gueimonde M, Collado MC (2012). "Metagenomics and probiotics". Clinical Microbiology and Infection. 18 Suppl 4: 32–4. doi:10.1111/j.1469-0691.2012.03873.x. PMID 22647045.
- ^ Mach T (November 2006). "Clinical usefulness of probiotics against chronic inflammatory bowel diseases". Journal of Physiology and Pharmacology. 57 Suppl 9: 23–33. PMID 17242485.
- ^ Yan F, Polk DB (November 2006). "Probiotics as functional food in the treatment of diarrhea". Current Opinion in Clinical Nutrition and Metabolic Care. 9 (6): 717–21. doi:10.1097/01.mco.0000247477.02650.51. PMID 17053425.
- ^ Reid G (September 2008). "Probiotic Lactobacilli for urogenital health in women". J. Clin. Gastroenterol. 42 (Suppl 3 Pt 2): S234–6. doi:10.1097/MCG.0b013e31817f1298. PMID 18685506.
- ^ Vanderhoof JA (November 2008). "Probiotics in allergy management". Journal of Pediatric Gastroenterology and Nutrition. 47 Suppl 2: S38–40. doi:10.1097/01.mpg.0000338810.74933.c1. PMID 18931598.
- ^ "European Food Safety Authority (EFSA) – Committed since 2002 to ensuring that Europe's food is safe". Efsa.europa.eu. Retrieved 2012-11-08.
- ^ Ljungh A, Wadstrom T, ed. (2009). Lactobacillus Molecular Biology: From Genomics to Probiotics. Caister Academic Press. ISBN 978-1904455417.[page needed]
- ^ Gilliland SE, Walker DK (April 1990). "Factors to consider when selecting a culture of Lactobacillus acidophilus as a dietary adjunct to produce a hypocholesterolemic effect in humans". Journal of Dairy Science. 73 (4): 905–11. doi:10.3168/jds.S0022-0302(90)78747-4. PMID 2111831.[unreliable medical source?]
- ^ http://www.who.int/foodsafety/publications/fs_management/en/probiotics.pdf
- ^ Rowland I, Capurso L, Collins K, Cummings J, Delzenne N, Goulet O, Guarner F, Marteau P, Meier R (2010). "Current level of consensus on probiotic science: Report of an expert meeting-London, 23 November 2009". Gut Microbes. 1 (6): 436–439. doi:10.4161/gmic.1.6.13610. PMC 3056112. PMID 21637035.
{{cite journal}}: Invalid|display-authors=222(help)CS1 maint: multiple names: authors list (link) - ^ Sears, Cynthia L. (2005). "A dynamic partnership: Celebrating our gut flora". Anaerobe. 11 (5): 247–51. doi:10.1016/j.anaerobe.2005.05.001. PMID 16701579.
- ^ Slashinski MJ, McCurdy SA, Achenbaum LS, Whitney SN, McGuire AL (2012). ""Snake-oil," "quack medicine," and "industrially cultured organisms:" biovalue and the commercialization of human microbiome research". BMC Medical Ethics. 13: 28. doi:10.1186/1472-6939-13-28. PMC 3512494. PMID 23110633.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Wu, G. D.; Chen, J.; Hoffmann, C.; Bittinger, K.; Chen, Y.-Y.; Keilbaugh, S. A.; Bewtra, M.; Knights, D.; Walters, W. A.; Knight, R.; Sinha, R.; Gilroy, E.; Gupta, K.; Baldassano, R.; Nessel, L.; Li, H.; Bushman, F. D.; Lewis, J. D. (2011). "Linking Long-Term Dietary Patterns with Gut Microbial Enterotypes". Science. 334 (6052): 105–8. doi:10.1126/science.1208344. PMC 3368382. PMID 21885731.
- ^ a b Crislip, Mark (16 January 2009). "Probiotics". Science-based Medicine. Retrieved 8 October 2013.
- ^ Colin Hill, Francisco Guarner, Gregor Reid, Glenn R. Gibson, Daniel J. Merenstein, Bruno Pot, Lorenzo Morelli, Roberto Berni Canani, Harry J. Flint, Seppo Salminen, Philip C. Calder, Mary Ellen Sanders (2014). "Expert consensus document: The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic". Nature Reviews Gastroenterology and Hepatology. 11 (8): 506–514. doi:10.1038/nrgastro.2014.66.
{{cite journal}}: horizontal tab character in|author=at position 61 (help)CS1 maint: multiple names: authors list (link) - ^ Elazab N, Mendy A, Gasana J, Vieira ER, Quizon A, Forno E (2013). "Probiotic Administration in Early Life, Atopy, and Asthma: A Meta-analysis of Clinical Trials". Pediatrics. 132 (3): e666–76. doi:10.1542/peds.2013-0246. PMID 23958764.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ King CK, Glass R, Bresee JS, Duggan C (November 2003). "Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy". MMWR Recomm Rep. 52 (RR–16): 1–16. PMID 14627948.
{{cite journal}}: CS1 maint: multiple names: authors list (link)[unreliable medical source?] - ^ Allen SJ, Martinez EG, Gregorio GV, Dans LF (2010). Allen, Stephen J (ed.). "Probiotics for treating acute infectious diarrhoea". Cochrane Database Syst Rev. 11 (11): CD003048. doi:10.1002/14651858.CD003048.pub3. PMID 21069673.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Probiotics 'ease upset stomachs'". NHS Choices. 2010. Retrieved 28 October 2013.
- ^ a b Johnston BC, Goldenberg JZ, Vandvik PO, Sun X, Guyatt GH (2011). "Probiotics for the prevention of pediatric antibiotic-associated diarrhea". Cochrane Database Syst Rev (11): CD004827. doi:10.1002/14651858.CD004827.pub3. PMID 22071814.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Szajewska H, Ruszczyński M, Radzikowski A (2006). "Probiotics in the prevention of antibiotic-associated diarrhea in children: a meta-analysis of randomized controlled trials". J. Pediatr. 149 (3): 367–372. doi:10.1016/j.jpeds.2006.04.053. PMID 16939749.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ McFarland LV (2006). "Meta-analysis of probiotics for the prevention of antibiotic associated diarrhea and the treatment of Clostridium difficile disease". Am. J. Gastroenterol. 101 (4): 812–22. doi:10.1111/j.1572-0241.2006.00465.x. PMID 16635227.
- ^ Segarra-Newnham M (2007). "Probiotics for Clostridium difficile-Associated Diarrhea: Focus on Lactobacillus rhamnosus GG and Saccharomyces boulardii". Annals of Pharmacotherapy. 41 (7): 1212–1221. doi:10.1345/aph.1K110. PMID 17595306.
- ^
- D'Souza AL, Rajkumar C, Cooke J, Bulpitt CJ (June 2002). "Probiotics in prevention of antibiotic associated diarrhoea: meta-analysis". BMJ. 324 (7350): 1361. doi:10.1136/bmj.324.7350.1361. PMC 115209. PMID 12052801.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Cremonini F, Di Caro S, Nista EC, Bartolozzi F, Capelli G, Gasbarrini G, Gasbarrini A (August 2002). "Meta-analysis: the effect of probiotic administration on antibiotic-associated diarrhoea". Aliment. Pharmacol. Ther. 16 (8): 1461–7. doi:10.1046/j.1365-2036.2002.01318.x. PMID 12182746.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - McFarland LV (April 2006). "Meta-analysis of probiotics for the prevention of antibiotic associated diarrhea and the treatment of Clostridium difficile disease". Am J Gastroenterol. 101 (4): 812–22. doi:10.1111/j.1572-0241.2006.00465.x. PMID 16635227.
- Szajewska H, Mrukowicz J (2005-09-01). "Meta-analysis: non-pathogenic yeast Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea". Aliment Pharmacol Ther. 22 (5): 365–72. doi:10.1111/j.1365-2036.2005.02624.x. PMID 16128673.
- Szajewska H, Ruszczyński M, Radzikowski A (September 2006). "Probiotics in the prevention of antibiotic-associated diarrhea in children: a meta-analysis of randomized controlled trials". J Pediatr. 149 (3): 367–372. doi:10.1016/j.jpeds.2006.04.053. PMID 16939749.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Sazawal S, Hiremath G, Dhingra U, Malik P, Deb S, Black RE (June 2006). "Efficacy of probiotics in prevention of acute diarrhoea: a meta-analysis of masked, randomised, placebo-controlled trials". Lancet Infect Dis. 6 (6): 374–82. doi:10.1016/S1473-3099(06)70495-9. PMID 16728323.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- D'Souza AL, Rajkumar C, Cooke J, Bulpitt CJ (June 2002). "Probiotics in prevention of antibiotic associated diarrhoea: meta-analysis". BMJ. 324 (7350): 1361. doi:10.1136/bmj.324.7350.1361. PMC 115209. PMID 12052801.
- ^ Arvola T, Laiho K, Torkkeli S, Mykkänen H, Salminen S, Maunula L, Isolauri E (1999). "Prophylactic Lactobacillus GG reduces antibiotic-associated diarrhea in children with respiratory infections: A randomized study". Pediatrics. 104 (5): e64. doi:10.1542/peds.104.5.e64. PMID 10545590.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Doron SI, Hibberd PL, Gorbach SL (July 2008). "Probiotics for prevention of antibiotic-associated diarrhea". J Clin Gastroenterol. 42 (Suppl 2): S58–63. doi:10.1097/MCG.0b013e3181618ab7. PMID 18542041.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Surawicz CM (July 2008). "Role of probiotics in antibiotic-associated diarrhea, Clostridium difficile-associated diarrhea, and recurrent Clostridium difficile-associated diarrhea". J Clin Gastroenterol. 42 (Suppl 2): S64–70. doi:10.1097/MCG.0b013e3181646d09. PMID 18545161.
- ^ a b c Sanders ME (February 2000). "Considerations for use of probiotic bacteria to modulate human health". The Journal of Nutrition. 130 (2S Suppl): 384S–390S. PMID 10721912. Retrieved 2012-05-14.
- ^ Kumar M, Nagpal R, Kumar R, Hemalatha R, Verma V, Kumar A, Chakraborty C, Singh B, Marotta F, Jain S, Yadav H (2012). "Cholesterol-lowering probiotics as potential biotherapeutics for metabolic diseases". Experimental Diabetes Research. 2012: 902917. doi:10.1155/2012/902917. PMC 3352670. PMID 22611376.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Agerholm-Larsen L, Bell ML, Grunwald GK, Astrup A (2002). "The effect of a probiotic milk product on plasma cholesterol: a meta-analysis of short term intervention studies". European Journal of Clinical Nutrition. 54 (11): 856–860. doi:10.1038/sj.ejcn.1601104. PMID 11114681.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kiessling G, Schneider J, Jahreis G (2002). "Long term consumption of fermented dairy products over 6 months increases HDL cholesterol". European Journal of Clinical Nutrition. 56 (9): 843–849. doi:10.1038/sj.ejcn.1601399. PMID 12209372.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b c d Reid G, Jass J, Sebulsky MT, McCormick JK (October 2003). "Potential uses of probiotics in clinical practice". Clin. Microbiol. Rev. 16 (4): 658–72. doi:10.1128/CMR.16.4.658-672.2003. PMC 207122. PMID 14557292.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Ouwehand AC, Salminen S, Isolauri E (August 2002). "Probiotics: an overview of beneficial effects" (PDF). Antonie Van Leeuwenhoek. 82 (1–4): 279–89. doi:10.1023/A:1020620607611. PMID 12369194. Retrieved 2012-05-14.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hatakka K, Savilahti E, Pönkä A, Meurman JH, Poussa T, Näse L, Saxelin M, Korpela R (June 2001). "Effect of long term consumption of probiotic milk on infections in children attending day care centres: double blind, randomised trial". BMJ. 322 (7298): 1327. doi:10.1136/bmj.322.7298.1327. PMC 32161. PMID 11387176.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Näse L, Hatakka K, Savilahti E, Saxelin M, Pönkä A, Poussa T, Korpela R, Meurman JH (2001). "Effect of long-term consumption of a probiotic bacterium, Lactobacillus rhamnosus GG, in milk on dental caries and caries risk in children". Caries Research. 35 (6): 412–20. doi:10.1159/000047484. PMID 11799281.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ University of Pennsylvania School of Medicine (February 3, 2010). "'Good' bacteria keep immune system primed to fight future infections". ScienceDaily. Retrieved July 13, 2010.
{{cite news}}: Check|url=value (help); soft hyphen character in|url=at position 28 (help) - ^ Hamilton-Miller JM (October 2003). "The role of probiotics in the treatment and prevention of Helicobacter pylori infection". International Journal of Antimicrobial Agents. 22 (4): 360–6. doi:10.1016/S0924-8579(03)00153-5. PMID 14522098.
- ^ Kirjavainen PV, Salminen SJ, Isolauri E (February 2003). "Probiotic bacteria in the management of atopic disease: underscoring the importance of viability". J. Pediatr. Gastroenterol. Nutr. 36 (2): 223–7. doi:10.1097/00005176-200302000-00012. PMID 12548058.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Boyle RJ, Bath-Hextall FJ, Leonardi-Bee J, Murrell DF, Tang ML (2008). Boyle, Robert John (ed.). "Probiotics for treating eczema". Cochrane Database Syst Rev (4): CD006135. doi:10.1002/14651858.CD006135.pub2. PMID 18843705.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Braat H, van den Brande J, van Tol E, Hommes D, Peppelenbosch M, van Deventer S (2004). "Lactobacillus rhamnosus induces peripheral hyporesponsiveness in stimulated CD4+ T cells via modulation of dendritic cell function". The American journal of clinical nutrition. 80 (6): 1618–25. PMID 15585777.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hitti, Miranda (April 25, 2006). "Probiotics May Help Stressed Gut". WebMD. Retrieved 2012-05-14.
- ^ Moayyedi P, Ford AC, Talley NJ, Cremonini F, Foxx-Orenstein AE, Brandt LJ, Quigley EM (March 2010). "The efficacy of probiotics in the treatment of irritable bowel syndrome: a systematic review". Gut (Systematic review). 59 (3): 325–32. doi:10.1136/gut.2008.167270. PMID 19091823.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Naidoo K, Gordon M, Fagbemi AO, Thomas AG, Akobeng AK (2011). "Probiotics for maintenance of remission in ulcerative colitis". Cochrane Database Syst Rev (Systematic review) (12): CD007443. doi:10.1002/14651858.CD007443.pub2. PMID 22161412.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Alfaleh K, Anabrees J, Bassler D, Al-Kharfi T (2011). "Probiotics for prevention of necrotizing enterocolitis in preterm infants". Cochrane Database of Systematic Reviews (Online). 3 (3): CD005496. doi:10.1002/14651858.CD005496.pub3. PMID 21412889.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cooke, G.; Behan, J.; Costello, M. (2006). "Newly identified vitamin K-producing bacteria isolated from the neonatal faecal flora". Microbial Ecology in Health and Disease. 18 (3–4): 133. doi:10.1080/08910600601048894.
- ^ Strozzi GP, Mogna L (2008). "Quantification of Folic Acid in Human Feces After Administration of Bifidobacterium Probiotic Strains". Journal of Clinical Gastroenterology. 42: S179–S184. doi:10.1097/MCG.0b013e31818087d8. PMID 18685499.
- ^ Molina VC, Médici M, Taranto MP, Font de Valdez G (2009). "Lactobacillus reuteriCRL 1098 prevents side effects produced by a nutritional vitamin B12deficiency". Journal of Applied Microbiology. 106 (2): 467–473. doi:10.1111/j.1365-2672.2008.04014.x. PMID 19200314.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Rosenfeldt V, Benfeldt E, Nielsen SD, Michaelsen KF, Jeppesen DL, Valerius NH, Paerregaard A (2003). "Effect of probiotic Lactobacillus strains in children with atopic dermatitis". J. Allergy Clin. Immunol. 111 (2): 389–95. doi:10.1067/mai.2003.389. PMID 12589361.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Pelucchi C, Chatenoud L, Turati F, Galeone C, Moja L, Bach JF, La Vecchia C (May 2012). "Probiotics supplementation during pregnancy or infancy for the prevention of atopic dermatitis: a meta-analysis". Epidemiology (Cambridge, Mass.). 23 (3): 402–414. doi:10.1097/EDE.0b013e31824d5da2. ISSN 1531-5487. PMID 22441545.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Borges S, Silva J, Teixeira P (March 2014). "The role of lactobacilli and probiotics in maintaining vaginal health". Arch. Gynecol. Obstet. (Review). 289 (3): 479–89. doi:10.1007/s00404-013-3064-9. PMID 24170161.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Mayo, B; van Sinderen, D, eds. (2010). Bifidobacteria: Genomics and Molecular Aspects. Caister Academic Press. ISBN 978-1-904455-68-4.
- ^ Sonomoto, K; Yokota, A, eds. (2011). Lactic Acid Bacteria and Bifidobacteria: Current Progress in Advanced Research. Caister Academic Press. ISBN 978-1-904455-82-0.
- ^ Besselink MG, van Santvoort HC, Buskens E, Boermeester MA, van Goor H, Timmerman HM, Nieuwenhuijs VB, Bollen TL, van Ramshorst B, Witteman BJ, Rosman C, Ploeg RJ, Brink MA, Schaapherder AF, Dejong CH, Wahab PJ, van Laarhoven CJ, van der Harst E, van Eijck CH, Cuesta MA, Akkermans LM, Gooszen HG (February 2008). "Probiotic prophylaxis in predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial". Lancet. 371 (9613): 651–9. doi:10.1016/S0140-6736(08)60207-X. PMID 18279948.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ a b Bee, Peta (November 10, 2008). "Probiotics, Not so friendly after all". The Times. London.
- ^ "So-called 'friendly' bacteria may be dangerous, according to new research - so which should you be taking?". Daily Mail. 29 January 2008.
- ^ Islam MA, Yun CH, Choi YJ, Cho CS (2010). "Microencapsulation of live probiotic bacteria" (PDF). Journal of Microbiology and Biotechnology. 20 (1367–1377): 1367–1377. doi:10.4014/jmb.1003.03020. PMID 21030820.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Raoult D (September 2009). "Probiotics and obesity : a link ?". Nature Reviews Microbiology. 7 (9): 616. doi:10.1038/nrmicro2209. PMID 21548178.
- ^ Raoult, Didier (2009). "No link between probiotics and obesity? Author reply" (PDF). Nature Reviews Microbiology. 7 (12): 901. doi:10.1038/nrmicro2209-c3.
- ^ Ehrlich SD (2009). "Probiotics - little evidence for a link to obesity". Nature Reviews Microbiology. 7 (12): 901, author reply 901. doi:10.1038/nrmicro2209-c1. PMID 19915581.
- ^ Bee, Peta (November 10, 2008). "Probiotics, not so friendly after all?". The Times. London. Retrieved 18 June 2010.
- ^ Sanders, ME (June 2007). "Probiotics, strains matter". Functional foods & nutraceuticals magazine: 36–41.
- ^ Hun L (2009). "Bacillus coagulans Significantly Improved Abdominal Pain and Bloating in Patients with IBS". Postgraduate Medicine. 121 (2): 119–124. doi:10.3810/pgm.2009.03.1984. PMID 19332970. Retrieved 2012-05-14.
- ^ Baron M (2009). "A patented A Strain of Bacillus coagulans Increased Immune Response to Viral Challenge". Postgraduate Medicine. 121 (2): 114–118. doi:10.3810/pgm.2009.03.1971. PMID 19332969. Retrieved 2012-05-14.
- ^ Brenner DM, Moeller MJ, Chey WD, Schoenfeld PS (April 2009). "The utility of probiotics in the treatment of irritable bowel syndrome: a systematic review". Am J Gastroenterol. 104 (4): 1033–49, quiz 1050. doi:10.1038/ajg.2009.25. PMID 19277023.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Engelbrektson A, Korzenik JR, Pittler A, Sanders ME, Klaenhammer TR, Leyer G, Kitts CL (2009). "Probiotics to minimize the disruption of faecal microbiota in healthy subjects undergoing antibiotic therapy". J. Med. Microbiol. 58 (Pt 5): 663–70. doi:10.1099/jmm.0.47615-0. PMID 19369530.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sarker SA, Sultana S, Fuchs GJ, Alam NH, Azim T, Brüssow H, Hammarström L (August 2005). "Lactobacillus paracasei strain ST11 has no effect on rotavirus but ameliorates the outcome of nonrotavirus diarrhea in children from Bangladesh". Pediatrics. 116 (2): e221–8. doi:10.1542/peds.2004-2334. PMID 15995003.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sgouras DN, Panayotopoulou EG, Martinez-Gonzalez B, Petraki K, Michopoulos S, Mentis A (2005). "Lactobacillus johnsonii La1 Attenuates Helicobacter pylori-Associated Gastritis and Reduces Levels of Proinflammatory Chemokines in C57BL/6 Mice". Clinical and Vaccine Immunology. 12 (12): 1378. doi:10.1128/CDLI.12.12.1378-1386.2005. PMC 1317072. PMID 16339060.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Niedzielin K, Kordecki H, Birkenfeld B (October 2001). "A controlled, double-blind, randomized study on the efficacy of Lactobacillus plantarum 299V in patients with irritable bowel syndrome". Eur J Gastroenterol Hepatol. 13 (10): 1135–6. doi:10.1097/00042737-200110000-00004. PMID 11711768.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Shornikova AV, Casas IA, Isolauri E, Mykkänen H, Vesikari T (1997). "Lactobacillus reuteri as a therapeutic agent in acute diarrhea in young children". J Pediatr Gastroenterol Nutr. 24 (4): 399–404. doi:10.1097/00005176-199704000-00008. PMID 9144122.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Shornikova AV, Casas IA, Mykkänen H, Salo E, Vesikari T (December 1997). "Bacteriotherapy with Lactobacillus reuteri in rotavirus gastroenteritis". Pediatr. Infect. Dis. J. 16 (12): 1103–7. doi:10.1097/00006454-199712000-00002. PMID 9427453.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Savino F, Pelle E, Palumeri E, Oggero R, Miniero R (2007). "Lactobacillus reuteri ATCC 55730 versus Simethicone in the treatment of infantile colic: a prospective randomized study". Pediatrics. 119 (1): e124–e130. doi:10.1542/peds.2006-1222. PMID 17200238.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Saggioro A, Caroli M, Pasini M, Bortoluzzi F, Girardi L, Pilone G. (2005). "Helicobacter pylori eradication with Lactobacillus reuteri. A double blind placebo-controlled study". Dig Liver Dis. 37 (suppl 1): S88, abstr. PO1.49.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Lionetti E, Miniello VL, Castellaneta SP, Magistá AM, de Canio A, Maurogiovanni G, Ierardi E, Cavallo L, Francavilla R (2006). "Lactobacillus reuteri therapy to reduce side-effects during anti-Helicobacter pylori treatment in children: a randomised placebo controlled trial". Aliment Pharmacol Ther. 24 (10): 1461–1468. doi:10.1111/j.1365-2036.2006.03145.x. PMID 17032283.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cimperman L, Bayless G, Best K, Diligente A, Mordarski B, Oster M, Smith M, Vatakis F, Wiese D, Steiber A, Katz J (2011). "A randomized, double-blind, placebo-controlled pilot study of Lactobacillus reuteri ATCC 55730 for the prevention of antibiotic-associated diarrhea in hospitalized adults". J Clin Gastroenterol. 45 (9): 785–789. doi:10.1097/MCG.0b013e3182166a42. PMID 21552138.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Weizman Z, Asli G, Alsheikh A (January 2005). "Effect of a probiotic infant formula on infections in child care centers: comparison of two probiotic agents". Pediatrics. 115 (1): 5–9. doi:10.1542/peds.2004-1815. PMID 15629974.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ Tubelius P, Stan V, Zachrisson A (2005). "Increasing work-place healthiness with the probiotic Lactobacillus reuteri: a randomised, double-blind placebo-controlled study". Environ Health. 4: 25. doi:10.1186/1476-069X-4-25. PMC 1298318. PMID 16274475.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Rosander A, Connolly E, Roos S (Oct 2008). "Removal of antibiotic resistance gene-carrying plasmids from Lactobacillus reuteri ATCC 55730 and characterization of the resulting daughter strain, L. reuteri DSM 17938". Appl Environ Microbiol. 74 (19): 6032–40. doi:10.1128/AEM.00991-08. PMC 2565949. PMID 18689509.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Francavilla R, Lionetti E, Castellaneta S, Ciruzzi F, Indrio F, Masciale A, Fontana C, La Rosa MM, Cavallo L, Francavilla A (2012). "Randomised clinical trial: Lactobacillus reuteri DSM 17938 vs. placebo in children with acute diarrhoea - a double-blind study". Aliment Pharmacol Ther. 36 (4): 363–369. doi:10.1111/j.1365-2036.2012.05180.x. PMID 22680836.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Savino F, Cordisco L, Tarasco V, Palumeri E, Calabrese R, Oggero R, Roos S, Matteuzzi D (2010). "Lactobacillus reuteri DSM 17938 in infantile colic: A randomized, double-blind, placebo-controlled trial". Pediatrics. 126 (3): 526–533. doi:10.1542/peds.2010-0433. PMID 20713478.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Szajewska H, Gyrczuk E, Horvath A (2013). "Lactobacillus reuteri DSM 17938 for the management of infantile colic in breastfed infants: a randomized, double-blind, placebo-controlled trial". J Pediatr. 162 (2): 257–262. doi:10.1016/j.jpeds.2012.08.004. PMID 22981952.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Agustina R, Kok FJ, van de Rest O, Fahmida U, Firmansyah A, Lukito W, Feskens EJ, van den Heuvel EG, Albers R, Bovee-Oudenhoven IM (2012). "Randomized trial of probiotics and calcium on diarrhea and respiratory tract infections in Indonesian children". Pediatrics. 129 (5): 1155–1164. doi:10.1542/peds.2011-1379. PMID 22492764.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Coccorullo P, Strisciuglio C, Martinelli M, Miele E, Greco L, Staiano A (2010). "Lactobacillus reuteri (DSM 17938) in infants with functional chronic constipation: a double-blind, randomized, placebo-controlled study". J Pediatr. 157 (4): 598–602. doi:10.1016/j.jpeds.2010.04.066. PMID 20542295.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Romano C, Ferrau' V, Cavataio F, Iacono G, Spina M, Lionetti E, Comisi F, Famiani A, Comito D (2010). "Lactobacillus reuteri in children with functional abdominal pain (FAP)". J Paediatr Child Health.: no. doi:10.1111/j.1440-1754.2010.01797.x. PMID 20626584.
{{cite journal}}: Invalid|display-authors=3333(help)CS1 maint: multiple names: authors list (link) - ^ Krasse P, Carlsson B, Dahl C, Paulsson A, Nilsson A, Sinkiewicz G (2006). "Decreased gum bleeding and reduced gingivitis by the probiotic Lactobacillus reuteri". Swed Dent J. 30 (2): 55–60. PMID 16878680.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Twetman S, Derawi B, Keller M, Ekstrand K, Yucel-Lindberg T, Stecksen-Blicks C (2009). "Short-term effect of chewing gums containing probiotic Lactobacillus reuteri on the levels of inflammatory mediators in gingival crevicular fluid". Acta Odontol Scand. 67 (1): 19–24. doi:10.1080/00016350802516170. PMID 18985460.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Vivekananda MR, Vandana KL, Bhat KG (2010). "Effect of the probiotic Lactobacilli reuteri (Prodentis) in the management of periodontal disease: a preliminary randomized clinical trial". J Oral Microbiol. 2: 10.3402/jom.v2i0.5344. doi:10.3402/jom.v2i0.5344. PMC 3084569. PMID 21523225.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Vicario M, Santos A, Violant D, Nart J, Giner L (2012). "Clinical changes in periodontal subjects with the probiotic Lactobacillus reuteri Prodentis: A preliminary randomized clinical trial". Acta Odontol Scand. 71 (3–4): 813–9. doi:10.3109/00016357.2012.734404. PMID 23176716.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Keller MK, Bardow A, Jensdottir T, Lykkeaa J, Twetman S (2012). "Effect of chewing gums containing the probiotic bacterium Lactobacillus reuteri on oral malodour". Acta Odontol Scand. 70 (3): 246–250. doi:10.3109/00016357.2011.640281. PMID 22182258.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Caglar E, Kavaloglu SC, Kuscu OO, Sandalli N, Holgerson PL, Twetman S (2007). "Effect of chewing gums containing xylitol or probiotic bacteria on salivary mutans streptococci and lactobacilli". Clin Oral Investig. 11 (4): 425–429. doi:10.1007/s00784-007-0129-9. PMID 17574481.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Caglar E, Kuscu OO, Cildir SK, Kuvvetli SS, Sandalli N (2008). "A probiotic lozenge administered medical device and its effect on salivary mutans streptococci and lactobacilli". Int J Paediatr Dent. 18 (1): 35–39. doi:10.1111/j.1365-263X.2007.00866.x. PMID 18086024.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cildir SK, Sandalli N, Nazli S, Alp F, Caglar E (2012). "A novel delivery system of probiotic drop and its effect on dental caries risk factors in cleft lip/palate children". Swed Dent J. 49 (3): 369–372. doi:10.1597/10-035. PMID 21309653.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Czerucka, D.; Piche, T.; Rampal, P. (2007). "Review article: yeast as probiotics - Saccharomyces boulardii". Alimentary Pharmacology & Therapeutics. 26 (6): 767–778. doi:10.1111/j.1365-2036.2007.03442.x.
- ^ "Therapeutic evaluation of Saccharomyces boulardii in children with acute diarrhea" (PDF). Annales de Pediatrie. 41 (6): 397–400.
- ^ Kurugöl Z, Koturoğlu G (January 2005). "Effects of Saccharomyces boulardii in children with acute diarrhoea". Acta Paediatrica. 94 (1): 44–7. doi:10.1080/08035250410022521. PMID 15858959.
- ^ Anukam K, Osazuwa E, Ahonkhai I, Ngwu M, Osemene G, Bruce AW, Reid G (May 2006). "Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1® and Lactobacillus reuteri RC-14®: randomized, double-blind, placebo controlled trial". Microbes Infect. 8 (6): 1450–4. doi:10.1016/j.micinf.2006.01.003. PMID 16697231.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Beausoleil M, Fortier N, Guénette S, L'ecuyer A, Savoie M, Franco M, Lachaine J, Weiss K (November 2007). "Effect of a fermented milk combining Lactobacillus acidophilus Cl1285 and Lactobacillus casei in the prevention of antibiotic-associated diarrhea: a randomized, double-blind, placebo-controlled trial". Canadian Journal of Gastroenterology. 21 (11): 732–6. PMC 2658588. PMID 18026577.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Millette M, Luquet FM, Lacroix M (March 2007). "In vitro growth control of selected pathogens by Lactobacillus acidophilus- and Lactobacillus casei-fermented milk". Letters of Applied Microbiology. 44 (3): 314–9. doi:10.1111/j.1472-765X.2006.02060.x. PMID 17309510.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Robinson, R.K., ed. (2007). "Sellars, R.L.". Acidophilus Products (Therapeutic Properties of Fermented Milks). Chapman & Hall, London. pp. 81–116.
- ^ Berggren A, Lazou Ahrén I, Larsson N, Önning G (Aug 2010). "Randomised, double-blind and placebo-controlled study using new probiotic lactobacilli for strengthening the body immune defence against viral infections". Eur J Nutr. 50 (3): 203–10. doi:10.1007/s00394-010-0127-6. PMID 20803023.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Seseña S, Palop ML (2007). "An ecological study of lactic acid bacteria from Almagro eggplant fermentation brines". Journal of Applied Microbiology. 103 (5). Blackwell Publishing: 1553–1561. doi:10.1111/j.1365-2672.2007.03387.x. PMID 17953566. Retrieved 7 November 2007.
- ^ a b Frederick, Breidt, Jr; et al. (2007). "Fermented Vegetables" (PDF). ASM Press. Retrieved 7 November 2007.
{{cite web}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Ji, Feng-Di; Ji, B.-P.; Li, B.; Han, B.-Z. (2007). "Note. Microbial Changes During the Salting Process of Traditional Pickled Chinese Cabbage". Food Science and Technology International. 13 (1). SAGE Publications: 11–16. doi:10.1177/1082013207075952. Retrieved 7 November 2007.
- ^ a b c Kumar M, Ghosh M, Ganguli A (2012). "Mitogenic response and probiotic characteristics of lactic acid bacteria isolated from indigenously pickled vegetables and fermented beverages". World journal of microbiology & biotechnology. 28 (2): 703–11. doi:10.1007/s11274-011-0866-4. PMID 22806866.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Moreno MR, Leisner JJ, Tee LK, Ley C, Radu S, Rusul G, Vancanneyt M, De Vuyst L (2002). "Microbial analysis of Malaysian tempeh, and characterization of two bacteriocins produced by isolates of Enterococcus faecium". Journal of Applied Microbiology. 92 (1). The Microbiology Research Foundation: 147–157. doi:10.1046/j.1365-2672.2002.01509.x. PMID 11849339. Retrieved 7 November 2007.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Plessas S, Alexopoulos A, Voidarou C, Stavropoulou E, Bezirtzoglou E (2011). "Microbial ecology and quality assurance in food fermentation systems. The case of kefir grains application". Anaerobe. 17 (6): 483–5. doi:10.1016/j.anaerobe.2011.03.014. PMID 21497663.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Shiby VK, Mishra HN (2013). "Fermented milks and milk products as functional foods--a review". Critical reviews in food science and nutrition. 53 (5): 482–96. doi:10.1080/10408398.2010.547398. PMID 23391015.
- ^ Oh CK, Oh MC, Kim SH (2004). "The Depletion of Sodium Nitrite by Lactic Acid Bacteria Isolated from Kimchi". Journal of Medicinal Food. 7 (1). Mary Ann Liebert: 38–44. doi:10.1089/109662004322984680. PMID 15117551. Retrieved 7 November 2007.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Pederson CS, Niketic G, Albury MN (1962). "Fermentation of the Yugoslavian pickled cabbage". Applied microbiology. 10 (1): 86–9. PMC 1057814. PMID 14484853.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Friedman, Y; Hugenholtz, Jeroen; De Vos, Willem M.; Smid, Eddy J. (2006). "Safe use of genetically modified lactic acid bacteria in food. Bridging the gap between consumers, green groups, and industry". Electronic Journal of Biotechnology. 9 (4). Pontificia Universidad Católica de Valparaíso: E49–55. doi:10.2225/vol9-issue4-fulltext-12. Retrieved 7 November 2007.
- ^ Tanasupawat S, Thongsanit J, Okada S, Komagata K (2002). "Lactic acid bacteria isolated from soy sauce mash in Thailand". Journal of General and Applied Microbiology. 48 (4). The Microbiology Research Foundation: 201–209. doi:10.2323/jgam.48.201. PMID 12469319.
{{cite journal}}: Invalid|display-authors=1(help)CS1 maint: multiple names: authors list (link) - ^ EFSA calls for characterisation work as probiotic resubmissions loom
- ^ Template:Wayback
- ^ Timmerman HM, Koning CJ, Mulder L, Rombouts FM, Beynen AC (November 2004). "Monostrain, multistrain and multispecies probiotics—A comparison of functionality and efficacy". Int. J. Food Microbiol. 96 (3): 219–33. doi:10.1016/j.ijfoodmicro.2004.05.012. PMID 15454313.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Williams EA, Stimpson J, Wang D, Plummer S, Garaiova I, Barker ME, Corfe BM (September 2008). "Clinical trial: a multistrain probiotic preparation significantly reduces symptoms of irritable bowel syndrome in a double-blind placebo-controlled study". Aliment. Pharmacol. Ther. 29 (1): 97–103. doi:10.1111/j.1365-2036.2008.03848.x. PMID 18785988.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
