Tennis elbow
| Tennis elbow | |
|---|---|
| Other names | Enthesopathy of the extensor carpi radialis origin.[1] Lateral epicondylalgia, lateral elbow tendinopathy[2] |
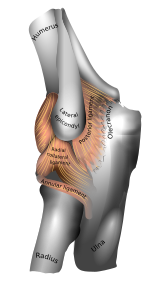 | |
| Left elbow-joint. (Lateral epicondyle visible at center.) | |
| Specialty | Orthopedics, sports medicine |
| Symptoms | Painful and tender outer part of the elbow[2] |
| Usual onset | Gradual[3] |
| Duration | Less than 1 to 2 years[4] |
| Causes | Middle age (ages 35-60). |
| Diagnostic method | Based on symptoms with medical imaging used to rule out other potential causes[3] |
| Differential diagnosis | Osteochondritis dissecans, osteoarthritis, radiculopathy[4] |
| Treatment | Nothing is proved to alter the natural course of the disease. Exercises, braces, ice or heat, and medications may be palliative. |
| Frequency | c. 2%[4] |
Tennis elbow, also known as lateral epicondylitis or enthesopathy of the extensor carpi radialis origin, is a condition in which the outer part of the elbow becomes painful and tender.[2][1] The pain may also extend into the back of the forearm.[3] Onset of symptoms is generally gradual although they can seem sudden and be misinterpreted as an injury.[3][5] Golfer's elbow is a similar condition that affects the inside of the elbow.[2]
Enthesopathies are idiopathic, meaning science has not yet determined the cause.[6] Enthesopathies are most common in middle age (ages 35 to 60).[7]
It is often stated that the condition is caused by excessive use of the muscles of the back of the forearm, but this is not supported by experimental evidence and is a common misinterpretation or unhelpful thought about symptoms.[3][8] It may be associated with work or sports, classically racquet sports,[2][3] but most people with the condition are not exposed to these activities.[9] The diagnosis is based on the symptoms and examination. Medical imaging is not particularly useful.[3][10] Signs consistent with the diagnosis include pain when a subject tries to bend back the wrist when the wrist is against resistance.[2]
The natural history of untreated enthesopathy is resolution over a period of 1-2 years.[11] Palliative (symptoms alleviating) treatment may include pain medications such as NSAIDS or acetaminophen (paracetamol), a wrist brace or strap over the upper forearm.[2][3] The role of corticosteroid injections is debated.[12] Recent evidence suggests corticosteroid injections may delay symptom resolution.[13]
Signs and symptoms
- Pain on the outer part of the elbow (lateral epicondyle)
- Point tenderness over the lateral epicondyle—a prominent part of the bone on the outside of the elbow
- Pain with resisted wrist extension or passive wrist flexion[14]
Symptoms associated with tennis elbow include, but are not limited to, pain from the outside of the elbow to the forearm and wrist and pain during extension of wrist.[15]
Terminology
The term "tennis elbow" is widely used (although informal), but the condition should be understood as not limited to tennis players.[16][17] Historically, the medical term "lateral epicondylitis" was most commonly used for the condition, but "itis" implies inflammation and the condition is not inflammatory.[3][16][17][18][19]
Since histological findings reveal noninflammatory tissue, the terms “lateral elbow tendinopathy" and "tendinosis” are suggested.[20][21] In 2019, a group of international experts suggested that "lateral elbow tendinopathy" was the most appropriate terminology.[22] But a disease of an attachment point (or enthesia) is most accurately referred to as an "enthesopathy."[23]
Causes

Enthesopathy of the extensor carpi radialis brevis origin is idiopathic, meaning that it has no known cause.[24]
Tennis players generally believe tennis elbow is caused by the repetitive nature of hitting thousands of tennis balls, which leads to tiny tears in the forearm tendon attachment at the elbow.[18] Traditionally, people have speculated that tennis elbow is a type of repetitive strain injury resulting from tendon overuse and failed healing of the tendon, but there is no evidence of injury or repair on histopathology, and misinterpretation of painful activities as a source of damage is common.[25]
Other speculative risk factors for lateral epicondylitis include taking up tennis later in life, unaccustomed strenuous activity, decreased mental chronometry and speed and repetitive eccentric contraction of muscle (controlled lengthening of a muscle group).[citation needed]

Pathophysiology
Histological findings are of mucoid degeneration: disorganized collagen, increased extracellular matrix, and chondroid metaplasia. There is no evidence of inflammation or repair.[26] Therefore, the disorder is more appropriately referred to as tendinosis or tendinopathy—more accurately an enthesopathy—rather than tendinitis.[20]
Diagnosis
Physical examination
Diagnosis is based on symptoms and clinical signs that are discrete and characteristic. For example, extension of the elbow and flexion of the wrist cause outer elbow pain. There is point tenderness at the origin of the extensor carpi radialis brevis muscle from the lateral epicondyle (extensor carpi radialis brevis origin).[14] There is also pain with resisted wrist extension (Cozen's test).[27]
Medical imaging
Medical imaging is not necessary or helpful.[28]
X-rays can confirm and distinguish possibilities of existing causes of pain that are unrelated to tennis elbow, such as fracture or arthritis. Rarely, calcification can be found where the extensor muscles attach to the lateral epicondyle.[14] Medical ultrasonography and magnetic resonance imaging (MRI) are other valuable tools for diagnosis but are frequently avoided due to the high cost.[29]
Longitudinal sonogram of the lateral elbow displays thickening and heterogeneity of the common extensor tendon that is consistent with tendinosis, as the ultrasound reveals calcifications, intrasubstance tears, and marked irregularity of the lateral epicondyle. Although the term “epicondylitis” is frequently used to describe this disorder, most histopathologic findings of studies have displayed no evidence of an acute, or a chronic inflammatory process. Histologic studies have demonstrated that this condition is the result of tendon degeneration, which replaces normal tissue with a disorganized arrangement of collagen.
Treatment
The natural history of untreated enthesopathy is resolution over a period of 1-2 years.[30][31]
Exercises
One way to help treat minor cases of tennis elbow is simply to relax the affected arm. The rest lets stress and tightness within the forearm slowly relax and eventually have the arm in working condition—in a day or two, depending on the case.[citation needed]
Other approaches that are not experimentally tested include eccentric exercise using a rubber bar.[32][33] The exercise involves grasping a rubber bar, twisting it, then slowly untwisting it.[32][34] Although it can be considered an evidence-based practice, long-term results have not yet been determined.[35]
There are differences in opinions on whether it is okay if pain occurs during these exercises.[36] Some suggest pain of less than 5/10 is okay.[36]
Moderate evidence exists demonstrating that joint manipulation directed at the elbow and wrist and spinal manipulation directed at the cervical and thoracic spinal regions results in clinical changes to pain and function.[37][38] There is also moderate evidence for short-term and mid-term effectiveness of cervical and thoracic spine manipulation as an add-on therapy to concentric and eccentric stretching plus mobilisation of wrist and forearm. Although not yet conclusive, the short-term analgesic effect of manipulation techniques may allow more vigorous stretching and strengthening exercises, resulting in a better and faster recovery process of the affected tendon in lateral epicondylitis.[39]
Low level laser therapy, administered at specific doses and wavelengths directly to the lateral elbow tendon insertions, may result in short-term pain relief and less disability.[40]
Extracorporeal shockwave therapy, while safe, is of unclear benefit.[41][42]
Orthotic devices


Orthosis is a device externally used on the limb to improve the function or reduce the pain. Orthotics may be useful in tennis elbow, however long-term effects are unknown.[43] There are two main types of orthoses prescribed for this problem: counterforce elbow orthoses and wrist extension orthoses. Counterforce orthosis has a circumferential structure surrounding the arm. This orthosis usually has a strap which applies a binding force over the origin of the wrist extensors. The applied force by orthosis reduces the elongation within the musculotendinous fibers. Wrist extensor orthosis maintains the wrist in the slight extension. This position reduces the overloading strain at the lesion area.[citation needed]
Medication
Although anti-inflammatories are a commonly prescribed treatment for tennis elbow, the evidence for their effect is usually anecdotal with only limited studies showing a benefit.[44] A systematic review found that topical non-steroidal anti-inflammatory drugs (NSAIDs) may improve pain in the short term (up to 4 weeks) but was unable to draw firm conclusions due to methodological issues.[45] Evidence for oral NSAIDs is mixed.[45]
Evidence is poor for long term improvement from injections of any type, whether corticosteroids, botulinum toxin, prolotherapy or other substances.[46] Corticosteroid injection may be effective in the short term[47] however are of little benefit after a year, compared to a wait-and-see approach.[48] A randomized control trial comparing the effect of corticosteroid injection, physiotherapy, or a combination of corticosteroid injection and physiotherapy found that patients treated with corticosteroid injection versus placebo had lower complete recovery or improvement at 1 year (Relative risk 0.86). Patients that received corticosteroid injection also had a higher recurrence rate at 1 year versus placebo (54% versus 12%, relative risk 0.23).[49] Complications from repeated steroid injections include skin problems such as hypopigmentation and fat atrophy leading to indentation of the skin around the injection site.[47] Steroid injections against appear to be more effective than shock wave therapy.[50] Botulinum toxin type A to paralyze the forearm extensor muscles in those with chronic tennis elbow that has not improved with conservative measures may be viable.[51]
Surgery
Surgery is an option.[52][53][54] Surgical methods include:[55]
- Lengthening, release, debridement, or repair of the origin of the extrinsic extensor muscles of the hand at the lateral epicondyle
Surgical techniques for lateral epicondylitis can be done by open surgery, percutaneous surgery or arthroscopic surgery, with no high-quality evidence that any particular type is better or worse than another.[56][53] Side effects include infection, damage to nerves and inability to straighten the arm.[57] A review of the evidence related to surgery found that published studies were of low quality and did not show that surgery was any more effective than other treatments.[56] A subsequent research trial showed that surgery was no more effective than sham surgery, where patients only received a skin incision, although the trial was limited by a small number of patients.[58]
Prognosis
According to a review and metanalysis from 2022 about 90% of tennis elbow achieve resolution within one year[31]
Depending upon severity and quantity of multiple tendon injuries that have built up, the extensor carpi radialis brevis may not be fully healed by conservative treatment. Nirschl defines four stages of lateral epicondylitis, showing the introduction of permanent damage beginning at Stage 2.
- Inflammatory changes that are reversible
- Nonreversible pathologic changes to origin of the extensor carpi radialis brevis muscle
- Rupture of ECRB muscle origin
- Secondary changes such as fibrosis or calcification.[59]
Epidemiology
Epidemiology of enthesopathy of the ECRB origin
Evidence from imaging studies suggests that about 1 in 5 humans have detectable enthesopathy of the extensor carpi radialis brevis origin in their lifetime.[60] Symptoms likely vary and are self-limited. The signal changes on MRI seem permanent. There is no evidence that specific occupations or activities are associated with enthesopathy.[61]
Epidemiology of symptoms of lateral epicondylitis
Symptoms suggestive of lateral epicondylitis are present in about 1% of the adult population, and is most common between ages 40 and 60.[62] The prevalence varies somewhat between studies, likely as a result of varied diagnostic criteria and limited reliability between different observers.[63] The data regarding symptoms of lateral epicondylitis in relation to occupations and sports are inconsistent and inconclusive.[64] The shortcomings of the evidence that addresses the relationship between symptoms and occupation/sport include: variation in diagnostic criteria, limited reliability of diagnosis, confounding association of psychosocial factors, selection bias due to a high non-response rate, and the fact that exposures are usually by subjective patient report and symptomatic patient might perceive greater exposure.
History
German physician F. Runge[65] is usually credited for the first description of the condition, calling it "writer's cramp" (Schreibekrampf) in 1873.[66] Later, it was called "washer women's elbow".[67] British surgeon Henry Morris published an article in The Lancet describing "lawn tennis arm" in 1883.[68][65] The popular term "tennis elbow" first appeared the same year in a paper by H. P. Major, described as "lawn-tennis elbow".[69][70]
See also
References
- ^ a b Behazin M, Kachooei AR (March 2021). "Arthroscopic Recession Technique in the Surgery of Tennis Elbow by Sharp Cutting the Extensor Carpi Radialis Brevis (ECRB) Tendon Origin". The Archives of Bone and Joint Surgery. 9 (2): 174–179. doi:10.22038/abjs.2020.48173.2383. PMC 8121031. PMID 34026934.
- ^ a b c d e f g Hubbard MJ, Hildebrand BA, Battafarano MM, Battafarano DF (June 2018). "Common Soft Tissue Musculoskeletal Pain Disorders". Primary Care. 45 (2): 289–303. doi:10.1016/j.pop.2018.02.006. PMID 29759125. S2CID 46886582.
- ^ a b c d e f g h i "Tennis Elbow (Lateral Epicondylitis)". OrthoInfo. July 2015. Retrieved 21 June 2018.
- ^ a b c Vaquero-Picado A, Barco R, Antuña SA (November 2016). "Lateral epicondylitis of the elbow". EFORT Open Reviews. 1 (11): 391–397. doi:10.1302/2058-5241.1.000049. PMC 5367546. PMID 28461918.
- ^ Solheim E, Hegna J, Øyen J (June 2011). "Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows". Knee Surgery, Sports Traumatology, Arthroscopy. 19 (6): 1023–1027. doi:10.1007/s00167-011-1477-1. PMC 3096769. PMID 21409461.
- ^ Gorski, Jerrold M. (August 2018). "Evaluation of Sleep Position for Possible Nightly Aggravation and Delay of Healing in Tennis Elbow". JAAOS Global Research & Reviews. 3 (8): e082. doi:10.5435/JAAOSGlobal-D-19-00082. ISSN 2474-7661. PMC 6754212. PMID 31592507.
- ^ Garden, R. S. (1961-02-01). "Tennis elbow". The Journal of Bone and Joint Surgery. British Volume. 43-B (1): 100–106. doi:10.1302/0301-620X.43B1.100. ISSN 0301-620X.
- ^ Bunata, Robert E.; Brown, David S.; Capelo, Roderick (September 2007). "Anatomic Factors Related to the Cause of Tennis Elbow". JBJS. 89 (9): 1955–1963. doi:10.2106/JBJS.F.00727. ISSN 0021-9355. PMID 17768192.
- ^ "Mouse Elbow - Injury Overview".
- ^ Ma, Kun-Long; Wang, Hai-Qiang (2020). "Management of Lateral Epicondylitis: A Narrative Literature Review". Pain Research & Management. 2020: 6965381. doi:10.1155/2020/6965381. ISSN 1918-1523. PMC 7222600. PMID 32454922.
- ^ Vaquero-Picado, Alfonso; Barco, Raul; Antuña, Samuel A. (2016-11-22). "Lateral epicondylitis of the elbow". EFORT Open Reviews. 1 (11): 391–397. doi:10.1302/2058-5241.1.000049. ISSN 2058-5241. PMC 5367546. PMID 28461918.
- ^ Karjalainen, Teemu V; Ponkilainen, Ville; Chong, Alphonsus; Johnston, Renea V; Le, Thi Lan Anh; Lähdeoja, Tuomas A; Buchbinder, Rachelle (2022-09-06). "Glucocorticoid injections for lateral elbow pain". Cochrane Database of Systematic Reviews. 2022 (9). Wiley. doi:10.1002/14651858.cd001978.pub2. ISSN 1465-1858. S2CID 252151420.
- ^ Hsieh, Lin-Fen; Kuo, Ying-Chen; Lee, Chia-Cheng; Liu, Ya-Fang; Liu, Yu-Chia; Huang, Vincent (February 2018). "Comparison Between Corticosteroid and Lidocaine Injection in the Treatment of Tennis Elbow: A Randomized, Double-Blinded, Controlled Trial". American Journal of Physical Medicine & Rehabilitation. 97 (2): 83–89. doi:10.1097/PHM.0000000000000814. ISSN 0894-9115. PMID 28816704. S2CID 24498663.
- ^ a b c Sarwark JF (2010). Essentials of musculoskeletal care. Rosemont, Ill.: American Academy of Orthopaedic Surgeons. ISBN 978-0892035793. OCLC 706805938.
- ^ Geoffroy P, Yaffe MJ, Rohan I (January 1994). "Diagnosing and treating lateral epicondylitis". Canadian Family Physician. 40: 73–78. PMC 2379994. PMID 8312757.
- ^ a b "Tennis elbow (lateral epicondylitis) Elbow Pain". Cleveland Clinic. 2018. Retrieved 23 January 2018.
- ^ a b "Tennis elbow". Mayo Clinic. 2 August 2017. Retrieved 23 January 2018.
- ^ a b Smith C (18 June 2004). "What is tennis elbow?". BBC Sport Academy. Retrieved 23 January 2018.
- ^ Nirschl, Robert P; Ashman, Edward S (2004-01-01). "Tennis elbow tendinosis (epicondylitis)". Instructional Course Lectures. 53: 587–598. ISSN 0065-6895. PMID 15116648.
- ^ a b McShane JM, Nazarian LN, Harwood MI (October 2006). "Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow". Journal of Ultrasound in Medicine. 25 (10): 1281–1289. doi:10.7863/jum.2006.25.10.1281. PMID 16998100. S2CID 22963436.
- ^ du Toit C, Stieler M, Saunders R, Bisset L, Vicenzino B (November 2008). "Diagnostic accuracy of power Doppler ultrasound in patients with chronic tennis elbow". British Journal of Sports Medicine. 42 (11): 872–876. doi:10.1136/bjsm.2007.043901. hdl:10072/22142. PMID 18308874. S2CID 3274396.
- ^ Scott A, Squier K, Alfredson H, Bahr R, Cook JL, Coombes B, et al. (March 2020). "ICON 2019: International Scientific Tendinopathy Symposium Consensus: Clinical Terminology". British Journal of Sports Medicine. 54 (5): 260–262. doi:10.1136/bjsports-2019-100885. PMID 31399426. S2CID 199517946.
- ^ Ikonen, Joona; Lähdeoja, Tuomas; Ardern, Clare L.; Buchbinder, Rachelle; Reito, Aleksi; Karjalainen, Teemu (April 2022). "Persistent Tennis Elbow Symptoms Have Little Prognostic Value: A Systematic Review and Meta-analysis". Clinical Orthopaedics and Related Research. 480 (4): 647–660. doi:10.1097/CORR.0000000000002058. ISSN 0009-921X. PMC 8923574. PMID 34874323.
{{cite journal}}: CS1 maint: PMC embargo expired (link) - ^ "Tennis Elbow". Hughston Clinic. Retrieved 2022-08-17.
- ^ Gunn, C. C.; Milbrandt, W. E. (1976-05-08). "Tennis elbow and the cervical spine". Canadian Medical Association Journal. 114 (9): 803–809. ISSN 0008-4409. PMC 1957126. PMID 1268791.
- ^ Nirschl, Robert P; Ashman, Edward S (2004-01-01). "Tennis elbow tendinosis (epicondylitis)". Instructional Course Lectures. 53: 587–598. ISSN 0065-6895. PMID 15116648.
- ^ "Tennis elbow". MedlinePlus Medical Encyclopedia.
- ^ Orchard, John; Kountouris, Alex (2011-05-10). "The management of tennis elbow". BMJ. 342: d2687. doi:10.1136/bmj.d2687. ISSN 1756-1833. PMID 21558359. S2CID 8358075.
- ^ "Tennis Elbow". Mayo Clinic Medical Information and Tools for Healthy Living – MayoClinic.com. 15 October 2008.
- ^ Vaquero-Picado, Alfonso; Barco, Raul; Antuña, Samuel A. (2016-11-22). "Lateral epicondylitis of the elbow". EFORT Open Reviews. 1 (11): 391–397. doi:10.1302/2058-5241.1.000049. ISSN 2058-5241. PMC 5367546. PMID 28461918.
- ^ a b Ikonen J, Lähdeoja T, Ardern CL, Buchbinder R, Reito A, Karjalainen T (April 2022). "Persistent Tennis Elbow Symptoms Have Little Prognostic Value: A Systematic Review and Meta-analysis". Clin Orthop Relat Res. 480 (4): 647–660. doi:10.1097/CORR.0000000000002058. PMC 8923574. PMID 34874323.
{{cite journal}}: CS1 maint: PMC embargo expired (link) - ^ a b Tyler TF, Thomas GC, Nicholas SJ, McHugh MP (September 2010). "Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis: a prospective randomized trial". Journal of Shoulder and Elbow Surgery. 19 (6): 917–922. doi:10.1016/j.jse.2010.04.041. PMID 20579907.
- ^ Reynolds, Gretchen, "Phys Ed:An Easy Fix for Tennis Elbow?", The New York Times, August 25, 2009, 11:54 pm
- ^ http://www.thera-bandacademy.com/elements/clients/docs/Tyler%20et%20al%20JSES%202010__201009DD_123442.pdf [bare URL PDF]
- ^ Page P (September 2010). "A new exercise for tennis elbow that works!". North American Journal of Sports Physical Therapy. 5 (3): 189–193. PMC 2971639. PMID 21589674.
- ^ a b Coombes BK, Bisset L, Vicenzino B (November 2015). "Management of Lateral Elbow Tendinopathy: One Size Does Not Fit All". The Journal of Orthopaedic and Sports Physical Therapy. 45 (11): 938–949. doi:10.2519/jospt.2015.5841. PMID 26381484.
- ^ Vicenzino B, Cleland JA, Bisset L (2007). "Joint manipulation in the management of lateral epicondylalgia: a clinical commentary". The Journal of Manual & Manipulative Therapy. 15 (1): 50–56. doi:10.1179/106698107791090132. PMC 2565595. PMID 19066643.
- ^ Herd CR, Meserve BB (2008). "A systematic review of the effectiveness of manipulative therapy in treating lateral epicondylalgia". The Journal of Manual & Manipulative Therapy. 16 (4): 225–237. doi:10.1179/106698108790818288. PMC 2716156. PMID 19771195.
- ^ Hoogvliet P, Randsdorp MS, Dingemanse R, Koes BW, Huisstede BM (November 2013). "Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review". British Journal of Sports Medicine. 47 (17): 1112–1119. doi:10.1136/bjsports-2012-091990. PMID 23709519. S2CID 1679092.
- ^ Bjordal JM, Lopes-Martins RA, Joensen J, Couppe C, Ljunggren AE, Stergioulas A, Johnson MI (May 2008). "A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow)". BMC Musculoskeletal Disorders. 9: 75. doi:10.1186/1471-2474-9-75. PMC 2442599. PMID 18510742.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Extracorporeal shockwave therapy for refractory tennis elbow". Interventional procedures guidance. National Institute for Health and Clinical Excellence. August 2009. IPG313.
- ^ Thiele S, Thiele R, Gerdesmeyer L (December 2015). "Lateral epicondylitis: This is still a main indication for extracorporeal shockwave therapy". International Journal of Surgery. 24 (Pt B): 165–170. doi:10.1016/j.ijsu.2015.09.034. PMID 26455532.
- ^ Struijs PA, Smidt N, Arola H, Dijk C, Buchbinder R, Assendelft WJ (2002-01-21). "Orthotic devices for the treatment of tennis elbow". The Cochrane Database of Systematic Reviews. 2010 (1): CD001821. doi:10.1002/14651858.cd001821. PMC 8407516. PMID 11869609.
- ^ Jayanthi N. "Epicondylitis (tennis and golf elbow)". UpToDate. UpToDate, Inc. Retrieved 17 August 2015.
- ^ a b Pattanittum P, Turner T, Green S, Buchbinder R (May 2013). "Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults". The Cochrane Database of Systematic Reviews. 5 (5): CD003686. doi:10.1002/14651858.CD003686.pub2. PMC 7173751. PMID 23728646.
- ^ Krogh TP, Bartels EM, Ellingsen T, Stengaard-Pedersen K, Buchbinder R, Fredberg U, et al. (June 2013). "Comparative effectiveness of injection therapies in lateral epicondylitis: a systematic review and network meta-analysis of randomized controlled trials". The American Journal of Sports Medicine. 41 (6): 1435–1446. doi:10.1177/0363546512458237. PMID 22972856. S2CID 25355427.
- ^ a b Coombes BK, Bisset L, Vicenzino B (November 2010). "Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials". Lancet. 376 (9754): 1751–1767. doi:10.1016/S0140-6736(10)61160-9. hdl:10072/35812. PMID 20970844. S2CID 45054853.
- ^ Haines T, Stringer B (April 2007). "Corticosteroid injections or physiotherapy were not more effective than wait and see for tennis elbow at 1 year". Evidence-Based Medicine. 12 (2): 39. doi:10.1136/ebm.12.2.39. PMID 17400631. S2CID 43254510.
- ^ Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B (February 2013). "Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial". JAMA. 309 (5): 461–469. doi:10.1001/jama.2013.129. PMID 23385272.
- ^ Buchbinder R, Green SE, Youd JM, Assendelft WJ, Barnsley L, Smidt N (October 2005). "Shock wave therapy for lateral elbow pain". The Cochrane Database of Systematic Reviews. 2009 (4): CD003524. doi:10.1002/14651858.cd003524.pub2. PMC 8717012. PMID 16235324.
- ^ Kalichman L, Bannuru RR, Severin M, Harvey W (June 2011). "Injection of botulinum toxin for treatment of chronic lateral epicondylitis: systematic review and meta-analysis". Seminars in Arthritis and Rheumatism. 40 (6): 532–538. doi:10.1016/j.semarthrit.2010.07.002. PMID 20822798. S2CID 22022658.
- ^ Monto R (September 2014). "Tennis elbow repair with or without suture anchors: a randomized clinical trial". Techniques in Shoulder and Elbow Surgery. 15 (3): 92–97. doi:10.1097/BTE.0000000000000027. S2CID 58020081.
- ^ a b Lo MY, Safran MR (October 2007). "Surgical treatment of lateral epicondylitis: a systematic review". Clinical Orthopaedics and Related Research. 463: 98–106. doi:10.1097/BLO.0b013e3181483dc4. PMID 17632419. S2CID 6954029.
- ^ Solheim E, Hegna J, Øyen J (May 2013). "Arthroscopic versus open tennis elbow release: 3- to 6-year results of a case-control series of 305 elbows". Arthroscopy. 29 (5): 854–859. doi:10.1016/j.arthro.2012.12.012. PMID 23388420.
- ^ Faro F, Wolf JM (October 2007). "Lateral epicondylitis: review and current concepts". The Journal of Hand Surgery. 32 (8): 1271–1279. doi:10.1016/j.jhsa.2007.07.019. PMID 17923315.
- ^ a b Bateman M, Littlewood C, Rawson B, Tambe AA (February 2019). "Surgery for tennis elbow: a systematic review". Shoulder & Elbow. 11 (1): 35–44. doi:10.1177/1758573217745041. PMC 6348580. PMID 30719096.
- ^ Buchbinder R, Johnston RV, Barnsley L, Assendelft WJ, Bell SN, Smidt N (March 2011). "Surgery for lateral elbow pain". The Cochrane Database of Systematic Reviews (3): CD003525. doi:10.1002/14651858.cd003525.pub2. PMC 7154580. PMID 21412883.
- ^ Kroslak M, Murrell GA (April 2018). "Surgical Treatment of Lateral Epicondylitis: A Prospective, Randomized, Double-Blinded, Placebo-Controlled Clinical Trial". The American Journal of Sports Medicine. 46 (5): 1106–1113. doi:10.1177/0363546517753385. PMID 29498885. S2CID 4487650.
- ^ Owens BD, Wolf JM, Murphy KP (2009-11-03). "Lateral Epicondylitis: Workup". eMedicine Orthopedic Surgery. Retrieved 2010-04-19.
- ^ Drake, Matthew L.; Ring, David C. (June 2016). "Enthesopathy of the Extensor Carpi Radialis Brevis Origin: Effective Communication Strategies". The Journal of the American Academy of Orthopaedic Surgeons. 24 (6): 365–369. doi:10.5435/JAAOS-D-15-00233. ISSN 1940-5480. PMID 27077478.
- ^ Shiri, Rahman; Viikari-Juntura, Eira (February 2011). "Lateral and medial epicondylitis: role of occupational factors". Best Practice & Research. Clinical Rheumatology. 25 (1): 43–57. doi:10.1016/j.berh.2011.01.013. ISSN 1532-1770. PMID 21663849.
- ^ Shiri, Rahman; Viikari-Juntura, Eira (February 2011). "Lateral and medial epicondylitis: role of occupational factors". Best Practice & Research. Clinical Rheumatology. 25 (1): 43–57. doi:10.1016/j.berh.2011.01.013. ISSN 1532-1770. PMID 21663849.
- ^ Shiri, Rahman; Viikari-Juntura, Eira (February 2011). "Lateral and medial epicondylitis: role of occupational factors". Best Practice & Research. Clinical Rheumatology. 25 (1): 43–57. doi:10.1016/j.berh.2011.01.013. ISSN 1532-1770. PMID 21663849.
- ^ Shiri, Rahman; Viikari-Juntura, Eira (February 2011). "Lateral and medial epicondylitis: role of occupational factors". Best Practice & Research. Clinical Rheumatology. 25 (1): 43–57. doi:10.1016/j.berh.2011.01.013. ISSN 1532-1770. PMID 21663849.
- ^ a b "Tennis Elbow-Cap". The Lancet. 128 (3301): 1083. 1886. doi:10.1016/s0140-6736(00)49587-5.
- ^ Runge F (1873). "Zur Genese und Behandlung des Schreibekrampfes". Berliner Klin Wochenschr. 10: 245–248.
- ^ Renstrom PA (5 November 2013). "Elbow Injuries in Tennis". In Reilly T, Hughes M, Lees A (eds.). Science and Racket Sports. E & FN Spon. ISBN 978-0-419-18500-0.
- ^ Flatt AE (October 2008). "Tennis elbow". Proceedings. 21 (4): 400–402. doi:10.1080/08998280.2008.11928437. PMC 2566914. PMID 18982084.
- ^ Major HP (1883). "Lawn-tennis elbow". BMJ. 2 (1185): 556–558. doi:10.1136/bmj.2.1185.556. PMC 2372911.
- ^ Kaminsky SB, Baker CL (December 2003). "Lateral epicondylitis of the elbow". Techniques in Hand & Upper Extremity Surgery. 7 (4): 179–189. doi:10.1097/00130911-200312000-00009. PMID 16518219. S2CID 128648.
External links
- Wilson JJ, Best TM (September 2005). "Common overuse tendon problems: A review and recommendations for treatment". American Family Physician. 72 (5): 811–818. PMID 16156339. Archived from the original on 2007-09-29. Retrieved 2006-03-11.
