Bladder cancer: Difference between revisions
| Line 69: | Line 69: | ||
==Differential Diagnosis <ref name="bladder"/>== |
==Differential Diagnosis <ref name="bladder"/>== |
||
*[[ |
*[[Urinary tract infection]] |
||
*[[Urinary stones]] |
*[[Bladder_stone|Urinary stones]] |
||
*[[Trauma]] |
*[[Trauma]] |
||
* |
*Intrinsic glomerular disease |
||
*[[Kidney cancer]] |
*[[Kidney cancer]] |
||
*[[Prostate cancer]] |
*[[Prostate cancer]] |
||
Revision as of 18:12, 15 October 2011
| Bladder cancer | |
|---|---|
| Specialty | Oncology |
Bladder cancer is any of several types of malignant growths of the urinary bladder. It is a disease in which abnormal cells multiply without control in the bladder.[1] Bladder cancer is the most common malignancy of the urinary tract and the fourth most common cancer in men.[2] The bladder is a hollow, muscular organ that stores urine; it is located in the pelvis. The most common type of bladder cancer begins in cells lining the inside of the bladder and is called transitional cell carcinoma (sometimes urothelial cell carcinoma).
Risk Factors [2]
- Tobacco smoking
- Exposure to chemicals in the dye, rubber, petroleum, and textile industries
- Exposure to aromatic amines
- Chronic cystitis, especially in squamous cell
- Schistosoma haematobium
- Pelvic irradiation
- Cyclophosphamide
- Exposure to arsenic
- Analgesic abuse, artificial sweeteners, low fluid consumption, high intake of fried meats and fats, and high coffee consumption.
Signs and symptoms
Bladder cancer characteristically causes blood in the urine; this may be visible to the naked eye (gross hematuria) or detectable only by microscope (microscopic hematuria). Other possible symptoms include pain during urination, frequent urination (polyuria) or feeling the need to urinate without results. These signs and symptoms are not specific to bladder cancer, and are also caused by non-cancerous conditions, including prostate infections and cystitis. Kidney cancer also can cause hematuria.
Causes
Tobacco smoking is the main known contributor to urinary bladder cancer; in most populations, smoking is associated with over half of bladder cancer cases in men and one-third of cases among women.[3] There is a linear relationship between smoking and risk, and quitting smoking reduces the risk.[4] Passive smoking has not been proven to be involved.[5] In a 10-year study involving almost 48,000 men, researchers found that men who drank 1.5L of water a day had a significantly reduced incidence of bladder cancer when compared with men who drank less than 240mL (around 1 cup) per day. The authors proposed that bladder cancer might partly be caused by the bladder directly contacting carcinogens that are excreted in urine, although this has not yet been confirmed in other studies.[6] Thirty percent of bladder tumors probably result from occupational exposure in the workplace to carcinogens such as benzidine. 2-Naphthylamine, which is found in cigarette smoke, has also been shown to increase bladder cancer risk. Occupations at risk are bus drivers, rubber workers, motor mechanics, leather (including shoe) workers, blacksmiths, machine setters and mechanics.[7] Hairdressers are thought to be at risk as well because of their frequent exposure to permanent hair dyes. A 2008 study commissioned by the World Health Organisation concluded that "specific fruit and vegetables may act to reduce the risk of bladder cancer."[6] Fruit and yellow-orange vegetables, particularly carrots and selenium,[8] are probably associated with a moderately reduced risk of bladder cancer. Citrus fruits and cruciferous vegetables were also identified as having a possible protective effect.
It has been suggested that mutations at HRAS, KRAS2, RB1, and FGFR3 may be associated in some cases.[9]
Diagnosis
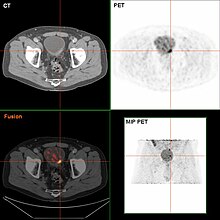
Many patients with a history, signs, and symptoms suspicious for bladder cancer are referred to a urologist or other physician trained in cystoscopy, a procedure in which a flexible tube bearing a camera and various instruments is introduced into the bladder through the urethra. Suspicious lesions may be biopsied and sent for pathologic analysis.[citation needed]
The gold standard for diagnosing bladder cancer is biopsy obtained during cystoscopy. Sometimes it is an incidental finding during cystoscopy.[10] Urine cytology can be obtained in voided urine or at the time of the cystoscopy ("bladder washing"). Cytology is very specific (a positive result is highly indicative of bladder cancer) but suffers from low sensitivity (inability of a negative result to reliably exclude bladder cancer). There are newer non-invasive urine bound markers available as aids in the diagnosis of bladder cancer, including human complement factor H-related protein, high-molecular-weight carcinoembryonic antigen, and nuclear matrix protein 22 (NMP22).[11] NMP22 is also available as a prescription home test.
The diagnosing of bladder cancer can also be done with a Cysview™ guided fluorescence cystoscopy, as an adjunct to conventional white-light cystoscopy. This procedure improves the detection of bladder cancer and reduces the rate of early tumour recurrence, compared with white-light cystoscopy alone. Cysview cystoscopy detects more cancer and reduce recurrency. Cysview is marketed in Europa under the brand name Hexvix® [12][13][14][15]
Pathological classification
90% of bladder cancers are Transitional cell carcinoma. The other 10% are squamous cell carcinoma, adenocarcinoma, sarcoma, small cell carcinoma and secondary deposits from cancers elsewhere in the body.[citation needed]
Carcinoma in situ (CIS) invariably consists of cytologically high grade tumour cells.[citation needed]
Staging
The following stages are used to classify the location, size, and spread of the cancer, according to the TNM (tumor, lymph node, and metastasis) staging system:
- Stage 0: Cancer cells are found only on the inner lining of the bladder (This stage is also often called Stage Ta).
- Stage I: Cancer cells have proliferated to the layer beyond the inner lining of the urinary bladder but not to the muscles of the urinary bladder.
- Stage II: Cancer cells have proliferated to the muscles in the bladder wall but not to the fatty tissue that surrounds the urinary bladder.
- Stage III: Cancer cells have proliferated to the fatty tissue surrounding the urinary bladder and to the prostate gland, vagina, or uterus, but not to the lymph nodes or other organs.
- Stage IV: Cancer cells have proliferated to the lymph nodes, pelvic or abdominal wall, and/or other organs.
- Recurrent: Cancer has recurred in the urinary bladder or in another nearby organ after having been treated.[16]
Differential Diagnosis [2]
- Urinary tract infection
- Urinary stones
- Trauma
- Intrinsic glomerular disease
- Kidney cancer
- Prostate cancer
- Benign prostate hypertrophy
- Menstrual blood contamination
Screening
As of 2010 there is insufficient evidence to determine if screening for bladder cancer in people without symptoms is effective or not.[17]
Treatment

The treatment of bladder cancer depends on how deep the tumor invades into the bladder wall. Superficial tumors (those not entering the muscle layer) can be "shaved off" using an electrocautery device attached to a cystoscope. Immunotherapy in the form of BCG instillation is also used to treat and prevent the recurrence of superficial tumors.[18]
BCG immunotherapy is effective in up to 2/3 of the cases at this stage. Instillations of chemotherapy, such as valrubicin (Valstar) into the bladder can also be used to treat BCG-refractory CIS disease when cystectomy is not an option.[19] Urocidin is phase III trials for this.[20]
Patients whose tumors recurred after treatment with BCG are more difficult to treat.[21] Many physicians recommend Cystectomy for these patients. This recommendation is in accordance with the official guidelines of the European Association of Urologists (EAU).[22] and the American Urological Association (AUA)[23] However, many patients refuse to undergo this life changing operation, and prefer to try novel conservative treatment options before opting to this last radical resort. Device assisted chemotherapy is such one group of novel technologies used to treat superficial bladder cancer.[24] These technologies use different mechanisms to facilitate the absorption and action of a chemotherapy drug instilled directly into the bladder. Another technology uses an electrical current to enhance drug absorption.[25] Another technology, thermotherapy, uses radio-frequency energy to directly heat the bladder wall, which together with chemotherapy shows a synergistic effect, enhancing each other's capacity to kill tumor cells. This technology was studied by different investigators.[26][27][28][29]
Untreated, superficial tumors may gradually begin to infiltrate the muscular wall of the bladder. Tumors that infiltrate the bladder require more radical surgery where part or all of the bladder is removed (a cystectomy) and the urinary stream is diverted. In some cases, skilled surgeons can create a substitute bladder (a neobladder) from a segment of intestinal tissue, but this largely depends upon patient preference, age of patient, renal function, and the site of the disease.
A combination of radiation and chemotherapy can also be used to treat invasive disease. It has not yet been determined how the effectiveness of this form of treatment compares to that of radical ablative surgery.
There is weak observational evidence from one very small study (84) to suggest that the concurrent use of statins is associated with failure of BCG immunotherapy.[30]
Photodynamic diagnosis may improve surgical outcome on bladder cancer.[31]
Epidemiology

In the United States, bladder cancer is the fourth most common type of cancer in men and the ninth most common cancer in women. More than 50,000 men and 16,000 women are diagnosed with bladder cancer each year. Smoking can only partially explain this higher incidence.[33] One other reason is that the androgen receptor, which is much more active in men than in women, plays a major part in the development of the cancer.[34] Certain medications, such as the diabetes drug Actos, manufactured by Takeda Pharmaceuticals, have also been associated with the causation of bladder cancer.
See also
References
- ^ Bladder cancer at Mount Sinai Hospital
- ^ a b c Essential Bladder Cancer Information Retrieved 15th October, 2011
- ^ Zeegers MP; Tan, FE; Dorant, E; Van Den Brandt, PA (2000). "The impact of characteristics of cigarette smoking on urinary tract cancer risk: a meta-analysis of epidemiologic studies". Cancer. 89 (3): 630–9. doi:10.1002/1097-0142(20000801)89:3<630::AID-CNCR19>3.0.CO;2-Q. PMID 10931463.
- ^ Boffetta P (2008). "Tobacco smoking and risk of bladder cancer". Scand J Urol Nephrol Suppl. 42 (S218): 45–54. doi:10.1080/03008880802283664. PMID 18815916.
- ^ Zeegers MP; Goldbohm, RA; Van Den Brandt, PA (2002). "A prospective study on active and environmental tobacco smoking and bladder cancer risk". Cancer Causes Control. 13 (1): 83–90. doi:10.1023/A:1013954932343. PMID 11899922.
- ^ a b Brinkman M, Zeegers MP (2008). "Nutrition, total fluid and bladder cancer". Scandinavian Journal of Urology and Nephrology. Supplementum. 42 (218): 25–36. doi:10.1080/03008880802285073. PMID 18815914.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Reulen RC, Zeegers MP (2008). "A meta-analysis on the association between bladder cancer and occupation". Scandinavian journal of urology and nephrology. Supplementum. 42 (218): 64–78. doi:10.1080/03008880802325192. PMID 18815919.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Brinkman M, Zeegers MP (2006). "Use of selenium in chemoprevention of bladder cancer". Lancet Oncol. 7 (9): 766–74. doi:10.1016/S1470-2045(06)70862-2. PMID 16945772.
- ^ Online Mendelian Inheritance in Man (OMIM): 109800
- ^ Walid MS, Heaton RL (2008). "Can posthysterectomy cystoscopy be utilized as a screening test for bladder cancer?". German Medical Science. 6: Doc13. PMC 2703254. PMID 19675739.
- ^ Shariat; Karam, JA; Lotan, Y; Karakiewizc, PI; et al. (2008). "Critical Evaluation of Urinary Markers for Bladder Cancer Detection and Monitoring". Reviews in Urology. 10 (2): 120–135. PMC 2483317. PMID 18660854.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ http://hexvix.com/about_hexvix.asp
- ^ http://cysview.net/
- ^ http://urotoday.com/bladder-cancer-1038/fluorescence-guided-transurethral-resection-of-bladder-tumours-reduces-bladder-tumour-recurrence-due-to-less-residual-tumour-tissue-in-t-at1-patients-a-randomized-two-centre-study-abstract.html Fluorescence-guided transurethral resection of bladder tumours reduces bladder tumour recurrence due to less residual tumour tissue in Ta/T1 patients
- ^ http://www.biotekforum.no/article.php?articleID=724&categoryID=6 Hexvix guided fluorescence cystoscopy reduces recurrence in patients
- ^ Longe, Jacqueline L. (2005). Gale Encyclopedia Of Cancer: A Guide To Cancer And Its Treatments. Detroit: Thomson Gale. p. 137. ISBN 978-1-4144-0362-5.
- ^ Chou R, Dana T (2010). "Screening adults for bladder cancer: a review of the evidence for the U.S. preventive services task force". Ann. Intern. Med. 153 (7): 461–8. doi:10.1059/0003-4819-153-7-201010050-00009. PMID 20921545.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Alexandroff AB, Jackson AM, O'Donnell MA, James K (1999). "BCG immunotherapy of bladder cancer: 20 years on". Lancet. 353 (9165): 1689–94. doi:10.1016/S0140-6736(98)07422-4. PMID 10335805.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Valstar Prescribing Information, available at
- ^ "Bioniche Earns $4M Milestone from Endo following Positive Phase III Urocidin Data". Nov 2010.
- ^ Witjes JA (2006). "Management of BCG failures in superficial bladder cancer: a review". European Urology. 49 (5): 790–7. doi:10.1016/j.eururo.2006.01.017. PMID 16464532.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Babjuk W, Oosterlinck W, Sylvester R; et al. (2010). "Guidelines on TaT1 (Non-muscle invasive) Bladder Cancer". European Association of Urology.
{{cite web}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Bladder Cancer Clinical Guideline Update Panel (2007). Bladder Cancer: Guideline for the Management of Nonmuscle Invasive Bladder Cancer: (Stages Ta,T1, and Tis): 2007 Update. American Urological Association.[page needed]
- ^ Witjes JA, Hendricksen K (2008). "Intravesical pharmacotherapy for non-muscle-invasive bladder cancer: a critical analysis of currently available drugs, treatment schedules, and long-term results". European Urology. 53 (1): 45–52. doi:10.1016/j.eururo.2007.08.015. PMID 17719169.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Di Stasi SM, Riedl C (2009). "Updates in intravesical electromotive drug administration of mitomycin-C for non-muscle invasive bladder cancer". World Journal of Urology. 27 (3): 325–30. doi:10.1007/s00345-009-0389-x. PMID 19234707.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Nativ O, Witjes JA, Hendricksen K; et al. (2009). "Combined thermo-chemotherapy for recurrent bladder cancer after bacillus Calmette-Guerin". The Journal of Urology. 182 (4): 1313–7. doi:10.1016/j.juro.2009.06.017. PMID 19683278.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Colombo R, Da Pozzo LF, Salonia A; et al. (2003). "Multicentric study comparing intravesical chemotherapy alone and with local microwave hyperthermia for prophylaxis of recurrence of superficial transitional cell carcinoma". Journal of Clinical Oncology. 21 (23): 4270–6. doi:10.1200/JCO.2003.01.089. PMID 14581436.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Alfred Witjes J, Hendricksen K, Gofrit O, Risi O, Nativ O (2009). "Intravesical hyperthermia and mitomycin-C for carcinoma in situ of the urinary bladder: experience of the European Synergo® working party". World Journal of Urology. 27 (3): 319–24. doi:10.1007/s00345-009-0384-2. PMC 2694311. PMID 19234857.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Halachmi S, Moskovitz B, Maffezzini M; et al. (2009). "Intravesical mitomycin C combined with hyperthermia for patients with T1G3 transitional cell carcinoma of the bladder". Urologic Oncology. 29 (3): 259–264. doi:10.1016/j.urolonc.2009.02.012. PMID 19395285.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Hoffmann P, Roumeguère T, Schulman C, van Velthoven R (2006). "Use of statins and outcome of BCG treatment for bladder cancer". The New England Journal of Medicine. 355 (25): 2705–7. doi:10.1056/NEJMc062714. PMID 17183004.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ http://www.nature.com/nrurol/journal/v7/n11/full/nrurol.2010.183.html Bladder cancer: Photodynamic diagnosis can improve surgical outcome Nature Reviews Urology 7, 598-599 (November 2010) | doi:10.1038/nrurol.2010.183
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved Nov. 11, 2009.
{{cite web}}: Check date values in:|accessdate=(help) - ^ Hemelt M, Zeegers MP (2000). "The effect of smoking on the male excess of bladder cancer: a meta-analysis and geographical analyses". Int J Cancer. 124 (2): 412–9. doi:10.1002/ijc.23856. PMID 18792102.
- ^ "Scientists Find One Reason Why Bladder Cancer Hits More Men". University of Rochester Medical Center. 2007-04-20.
{{cite news}}: Cite has empty unknown parameter:|coauthors=(help); Unknown parameter|is who want kill others accessdate=ignored (help)
External links
- American Bladder Cancer Society - bladder cancer support site for patients and caregivers
- Clinically reviewed bladder cancer information for patients, from Cancer Research UK
- UK bladder cancer statistics from Cancer Research UK
- Cancer.Net: Bladder Cancer
- MyBiopsy.org - information about bladder cancer diagnosis for patients, from physicians.
- Bladder cancer at Curlie
