Do not resuscitate: Difference between revisions
Rephrased. Tags: Mobile edit Mobile web edit |
Rescuing 1 sources and tagging 0 as dead. #IABot (v1.3.2.3) (Cyberpower678) |
||
| Line 72: | Line 72: | ||
In the United States, [[cardiopulmonary resuscitation]] (CPR) and [[advanced cardiac life support]] (ACLS) will not be performed if a valid written "DNR" order is present. Many states do not recognize [[living wills]] or [[health care proxy|health care proxies]] in the prehospital setting and prehospital personnel in those areas may be required to initiate resuscitation measures unless a specific state sponsored form is properly filled out and cosigned by a physician.<ref name="DO NOT RESUSCITATE – ADVANCE DIRECTIVES FOR EMS |
In the United States, [[cardiopulmonary resuscitation]] (CPR) and [[advanced cardiac life support]] (ACLS) will not be performed if a valid written "DNR" order is present. Many states do not recognize [[living wills]] or [[health care proxy|health care proxies]] in the prehospital setting and prehospital personnel in those areas may be required to initiate resuscitation measures unless a specific state sponsored form is properly filled out and cosigned by a physician.<ref name="DO NOT RESUSCITATE – ADVANCE DIRECTIVES FOR EMS |
||
Frequently Asked Questions and Answers ">{{cite news |
Frequently Asked Questions and Answers ">{{cite news|title=DO NOT RESUSCITATE – ADVANCE DIRECTIVES FOR EMS Frequently Asked Questions and Answers |url=http://www.emsa.ca.gov/personnel/DNR_faq.asp |accessdate=2009-08-23 |year=2007 |work=State of California Emergency Medical Services Authority |quote=# What if the EMT cannot find the DNR form or evidence of a MedicAlert medallion? Will they withhold resuscitative measures if my family asks them to? No. EMS personnel are taught to proceed with CPR when needed, unless they are absolutely certain that a qualified DNR advance directive exists for that patient. If, after spending a reasonable (very short) amount of time looking for the form or medallion, they do not see it, they will proceed with lifesaving measures. |deadurl=yes |archiveurl=https://web.archive.org/web/20090823161856/http://www.emsa.ca.gov/personnel/DNR_faq.asp |archivedate=2009-08-23 |df= }}</ref><ref name="Frequently Asked Questions re: DNR's ">{{cite news |title = Frequently Asked Questions re: DNR's |url =http://www.health.state.ny.us/nysdoh/ems/policy/99-10.htm |accessdate = 2009-08-23 |date = 1999-12-30 |work = New York State Department of Health |quote = May EMS providers accept living wills or health care proxies? A living will or health care proxy is NOT valid in the prehospital setting }}</ref> |
||
===Canada=== |
===Canada=== |
||
Revision as of 10:03, 24 May 2017
| Do not resuscitate | |
|---|---|
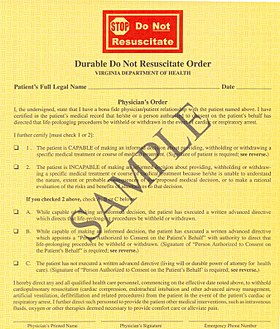 DNR form used in Virginia | |
| Other names | Do not attempt resuscitation, allow natural death, no code |
Do not resuscitate (DNR), also known as no code or allow natural death, is a legal order written either in the hospital or on a legal form to withhold cardiopulmonary resuscitation (CPR) or advanced cardiac life support (ACLS), in respect of the wishes of a patient in case their heart were to stop or they were to stop breathing. "No code" is a reference to the use of "code" as jargon for "calling in a Code Blue" to alert a hospital's resuscitation team. The DNR request is usually made by the patient or health care power of attorney and allows the medical teams taking care of them to respect their wishes. In the health care community, allow natural death (AND) is a term that is quickly gaining favor as it focuses on what is being done, not what is being avoided.[citation needed] Some criticize the term "do not resuscitate" because of the implication of important information being withheld, while research shows that only about 5% of patients who require CPR outside the hospital and only 15% of patients who require CPR while in the hospital survive.[1][2] Patients who are elderly, are living in nursing homes, have multiple medical problems, or who have advanced cancer are much less likely to survive.[3]
A DNR does not affect any treatment other than that which would require intubation or CPR. Patients who are DNR can continue to get chemotherapy, antibiotics, dialysis, or any other appropriate treatments.
Alternative terms
Other terms and abbreviations for this order are used in different countries. DNR (Do Not Resuscitate) is a common abbreviation in the United States, Canada and the United Kingdom. It may be clarified in some regions with the addition of DNI (Do Not Intubate), although in some hospitals DNR alone will imply no intubation. Clinically, the vast majority of people requiring resuscitation will require intubation, making a DNI alone problematic.
Some areas of the United States and the United Kingdom include the letter A, as in DNAR, to clarify "Do Not Attempt Resuscitation." This alteration is so that it is not presumed by the patient or family that an attempt at resuscitation will be successful. Since the term DNR implies the omission of action, and therefore "giving up", some have advocated for these orders to be retermed Allow Natural Death.[4] New Zealand and Australia, and some hospitals in the UK, use the term NFR or Not For Resuscitation. Typically these abbreviations are not punctuated, e.g., DNR rather than D.N.R.
Another synonymous term is "not to be resuscitated" (NTBR).[5]
Until recently in the UK it was common to write "Not for 222" or conversationally, "Not for twos." This was implicitly a hospital DNR order, where 222 (or similar) is the hospital telephone number for the emergency resuscitation or crash team.[citation needed]
Advance directive and living will
Advance directives and living wills are documents written by individuals themselves, so as to state their wishes for care, if they are no longer able to speak for themselves. In contrast, it is a physician or hospital staff member who writes a DNR "physician's order," based upon the wishes previously expressed by the individual in his or her advance directive or living will. Similarly, at a time when the individual is unable to express his wishes, but has previously used an advance directive to appoint an agent, then a physician can write such a DNR "physician's order" at the request of that individual's agent. These various situations are clearly enumerated in the "sample" DNR order presented on this page.
It should be stressed that, in the United States, an advance directive or living will is not sufficient to ensure a patient is treated under the DNR protocol, even if it is his wish, as neither an advance directive nor a living will is a legally binding document.
Ethics
DNR orders in certain situations have been subject to ethical debate. In many institutions it is customary for a patient going to surgery to have their DNR automatically rescinded. Though the rationale for this may be valid, as outcomes from CPR in the operating room are substantially better than general survival outcomes after CPR, the impact on patient autonomy has been debated. It is suggested that facilities engage patients or their decision makers in a 'reconsideration of DNR orders 'instead of automatically making a forced decision.[6]
There is accumulating evidence of a racial bias in DNR adoption. A 2014 study of end stage cancer patients found that non-Latino white patients were significantly more likely to have a DNR order (45%) than black (25%) and Latino (20%) patients. The correlation between preferences against life-prolonging care and the increased likelihood of advance care planning is consistent across ethnic groups.[7]
Ethical dilemmas occur when a patient with a DNR attempts suicide and the necessary treatment involves ventilation or CPR. In these cases it has been argued that the principle of beneficence takes precedence over patient autonomy and the DNR can be revoked by the physician.[8] Another dilemma occurs when a medical error happens to a patient with a DNR. If the error is reversible only with CPR or ventilation there is no consensus if resuscitation should take place or not.[9]
There are also ethical concerns around how patients reach the decision to make themselves a DNR. One study found that when questioned in more detail, many patients who were DNR actually would have wanted the excluded interventions depending on the scenario. Most would prefer life saving intubation in the scenario of angioedema which typically resolves in days. One fifth of the DNR patients would want resuscitation for cardiac arrest but to have care withdrawn after a week. It is possible that providers are having a "leading conversation" with patients or mistakenly leaving crucial information out when discussing DNR.[10] One study reported that physicians repeatedly give high intensity care to patients while deciding they themselves would be DNR under similar circumstances.[11]
There is also the ethical issue of discontinuation of an ICD implantable cardioverter defibrillator in DNR patients in cases of medical futility. A large survey of Electrophysiology practitioners, the heart specialists who implant pacemakers and ICD's noted that the practitioners felt that deactivating an ICD was not ethically distinct from withholding CPR thus consistent with DNR. Most felt that deactivating a pacemaker was a separate issue and could not be broadly ethically endorsed. Pacemakers were felt to be unique devices, or ethically taking a role of "keeping a patient alive" like dialysis.[12]
Usage by country
DNR documents are widespread in some countries and unavailable in others. In countries where a DNR is unavailable the decision to end resuscitation is made solely by physicians.
Middle East
DNRs are not recognized by Jordan. Physicians attempt to resuscitate all patients regardless of individual or familial wishes.[13] The UAE have laws forcing healthcare staff to resuscitate a patient even if the patient has a DNR or does not wish to live. There are penalties for breaching the laws.[14] In Saudi Arabia patients cannot legally sign a DNR, but DNR accepted by order of primary physician in case of terminally ill patients. In Israel, it is possible to sign a DNR form as long as the patient is dying and aware of their actions.[citation needed]
United Kingdom

England and Wales
In England and Wales, CPR is presumed in the event of a cardiac arrest unless a do not resuscitate order is in place. If they have capacity as defined under the Mental Capacity Act 2005 the patient may decline resuscitation, however any discussion is not in reference to consent to resuscitation and instead should be an explanation.[15] Patients may also specify their wishes and/or devolve their decision-making to a proxy using an advance directive, which are commonly referred to as 'Living Wills'. Patients and relatives cannot demand treatment (including CPR) which the doctor believes is futile and in this situation, it is their doctor's duty to act in their 'best interest', whether that means continuing or discontinuing treatment, using their clinical judgment. If they lack capacity relatives will often be asked for their opinion out of respect.
Scotland
In Scotland, the terminology used is "Do Not Attempt Cardiopulmonary Resuscitation" or "DNACPR". There is a single policy used across all of NHS Scotland. The legal standing is similar to that in England and Wales, in that CPR is viewed as a treatment and, although there is a general presumption that CPR will be performed in the case of cardiac arrest, this is not the case if it is viewed by the treating clinician to be futile. Patients and families cannot demand CPR to be performed if it is felt to be futile (as with any medical treatment) and a DNACPR can be issued despite disagreement, although it is good practice to involve all parties in the discussion.[16]
United States
In the United States the documentation is especially complicated in that each state accepts different forms, and advance directives and living wills are not accepted by EMS as legally valid forms. If a patient has a living will that specifies the patient requests to be DNR but does not have a properly filled out state sponsored form that is co-signed by a physician, EMS will attempt resuscitation.
The DNR decision by patients was first litigated in 1976 in In re Quinlan. The New Jersey Supreme Court upheld the right of Karen Ann Quinlan's parents to order her removal from artificial ventilation. In 1991 Congress passed into law the Patient Self-Determination Act that mandated hospitals honor an individual's decision in their healthcare.[17] Forty-nine states currently permit the next of kin to make medical decisions of incapacitated relatives, the exception being Missouri. Missouri has a Living Will Statute that requires two witnesses to any signed advance directive that results in a DNR/DNI code status in the hospital.
In the United States, cardiopulmonary resuscitation (CPR) and advanced cardiac life support (ACLS) will not be performed if a valid written "DNR" order is present. Many states do not recognize living wills or health care proxies in the prehospital setting and prehospital personnel in those areas may be required to initiate resuscitation measures unless a specific state sponsored form is properly filled out and cosigned by a physician.[18][19]
Canada
Do not resuscitate orders are similar to those used in the United States. In 1995, the Canadian Medical Association, Canadian Hospital Association, Canadian Nursing Association, and Catholic Health Association of Canada worked with Canadian Bar Association clarify and create a Joint Statement on Resuscitative Interventions guideline for use to determine when and how DNR orders are assigned.[20] DNR orders must be discussed by doctors with the patient or patient agents or patient's significant others. Unilateral DNR by medical professionals can only be used if the patient is in a vegetative state.[20]
See also
References
- ^ Fairbanks RJ, Shah MN, Lerner EB, Ilangovan K, Pennington EC, Schneider SM (March 2007). "Epidemiology and outcomes of out-of-hospital cardiac arrest in Rochester, New York". Resuscitation. 72 (3): 415–24. doi:10.1016/j.resuscitation.2006.06.135. PMID 17174021.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Zoch TW, Desbiens NA, DeStefano F, Stueland DT, Layde PM (July 2000). "Short- and long-term survival after cardiopulmonary resuscitation". Arch. Intern. Med. 160 (13): 1969–73. doi:10.1001/archinte.160.13.1969. PMID 10888971.
- ^ Ehlenbach WJ, Barnato AE, Curtis JR, et al. (July 2009). "Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly". N. Engl. J. Med. 361 (1): 22–31. doi:10.1056/NEJMoa0810245. PMC 2917337. PMID 19571280.
- ^ Alternative to "DNR" Designation: "Allow Natural Death" - Making Sense in the Health Care Industry.
- ^ Vincent JL, Van Vooren JP (Dec 2002). "[NTBR (Not to Be Resuscitated) in 10 questions]". Rev Med Brux. 23 (6): 497–9. PMID 12584945.
- ^ Dugan D, Riseman J. Do-Not-Resuscitate Orders in an Operating Room Setting #292. Journal Of Palliative Medicine [serial online]. July 2015;18(7):638-639.
- ^ Garrido M, Harrington S, Prigerson H. End-of-life treatment preferences: A key to reducing ethnic/racial disparities in advance care planning?. Cancer (0008543X) [serial online]. December 15, 2014;120(24):3981-3986.
- ^ Humble M. Do-Not-Resuscitate Orders and Suicide Attempts. National Catholic Bioethics Quarterly [serial online]. Winter2014 2014;14(4):661-671.
- ^ Hébert P, Selby D. Should a reversible, but lethal, incident not be treated when a patient has a do-not-resuscitate order?. CMAJ: Canadian Medical Association Journal [serial online]. April 15, 2014;186(7):528-530.
- ^ Capone R. PROBLEMS WITH DNR AND DNI ORDERS. (Cover story). Ethics & Medics [serial online]. March 2014;39(3):1-3.
- ^ Physicians provide high-intensity end-of-life care for patients, but "no code" for themselves. Medical Ethics Advisor Volume: 30 Issue 10 (2014) ISSN 0886-0653
- ^ Daeschler M, Verdino RJ, Caplan AL, Kirkpatrick JN (2015). "Defibrillator Deactivation against a Patient's Wishes: Perspectives of Electrophysiology Practitioners". Pacing and Clinical Electrophysiology. 38 (8): 917–924. doi:10.1111/pace.12614.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Mideast med-school camp: divided by conflict, united by profession". The Globe and Mail. August 2009. Retrieved 2009-08-22.
In hospitals in Jordan and Palestine, neither families nor social workers are allowed in the operating room to observe resuscitation, says Mohamad Yousef, a sixth-year medical student from Jordan. There are also no DNRs. "If it was within the law, I would always work to save a patient, even if they didn't want me to," he says.
- ^ http://www.thenational.ae/news/uae-news/courts/nurses-deny-knowledge-of-do-not-resuscitate-order-in-patients-death
- ^ "Decisions relating to cardiopulmonary resuscitation: A joint statement from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing" (PDF). Resus.org.uk. Resuscitation Council (UK). Retrieved 17 June 2014.
- ^ Scottish Government (May 2010). "Do Not Attempt Cardiopulmonary Resuscitation (DNACPR): Integrated Adult Policy" (PDF). NHS Scotland.
- ^ Eckberg, Evelyn (April 1998). "The continuing ethical dilemma of the do-not-resuscitate order". AORN Journal. Retrieved 2009-08-23.
The right to refuse or terminate medical treatment began evolving in 1976 with the case of Karen Ann Quinlan v New Jersey (70NJ10, 355 A2d, 647 [NJ 1976]). This spawned subsequent cases leading to the use of the DNR order.(4) In 1991, the Patient Self-Determination Act mandated hospitals ensure that a patient's right to make personal health care decisions is upheld. According to the act, a patient has the right to refuse treatment, as well as the right to refuse resuscitative measures.(5) This right usually is accomplished by the use of the DNR order.
- ^ "DO NOT RESUSCITATE – ADVANCE DIRECTIVES FOR EMS Frequently Asked Questions and Answers". State of California Emergency Medical Services Authority. 2007. Archived from the original on 2009-08-23. Retrieved 2009-08-23.
# What if the EMT cannot find the DNR form or evidence of a MedicAlert medallion? Will they withhold resuscitative measures if my family asks them to? No. EMS personnel are taught to proceed with CPR when needed, unless they are absolutely certain that a qualified DNR advance directive exists for that patient. If, after spending a reasonable (very short) amount of time looking for the form or medallion, they do not see it, they will proceed with lifesaving measures.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Frequently Asked Questions re: DNR's". New York State Department of Health. 1999-12-30. Retrieved 2009-08-23.
May EMS providers accept living wills or health care proxies? A living will or health care proxy is NOT valid in the prehospital setting
- ^ a b "Archived copy". Archived from the original on 2014-07-15. Retrieved 2012-12-05.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link)
External links
- Do Not Resuscitate Orders Published by the U.S. National Library of Medicine
- Decisions Relating to Cardiopulmonary Resuscitation Published by the Resuscitation Council (UK)
