Arteriovenous malformation
| Arteriovenous malformation | |
|---|---|
| Specialty | Medical genetics, neurosurgery |
Arteriovenous malformation or AVM is an abnormal connection between arteries and veins, bypassing the capillary system. This vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear in any location. Although many AVMs are asymptomatic, they can cause intense pain or bleeding or lead to other serious medical problems.
AVMs are usually congenital and belong to the RASopathies. The genetic transmission patterns of AVM, if any, are unknown. AVM is not generally thought to be an inherited disorder, unless in the context of a specific hereditary syndrome.
History
Emmanuel, Luschka and Virchow first described arteriovenous malformations in the mid-1800s. Olivecrona performed the first surgical excision of an intracranial AVM in 1932.
Signs and symptoms
Symptoms of AVM vary according to the location of the malformation. Roughly 88%[1] of people affected with AVM are asymptomatic; often the malformation is discovered as part of an autopsy or during treatment of an unrelated disorder (called in medicine "an incidental finding"); in rare cases its expansion or a micro-bleed from an AVM in the brain can cause epilepsy, deficit or pain.
The most general symptoms of a cerebral AVM include headache and epilepsy, with more specific symptoms occurring that normally depend on the location of the malformation and the individual. Such possible symptoms include:[2]
- Difficulties with movement or coordination, including muscle weakness and even paralysis;
- vertigo (dizziness);
- Difficulties of speech (dysarthria) and communication, such as aphasia;
- Difficulties with everyday activities, such as apraxia;
- Abnormal sensations (numbness, tingling, or spontaneous pain);
- Memory and thought-related problems, such as confusion, dementia or hallucinations.
Cerebral AVMs may present in a number of ways
- Hemorrhage (45% of cases)
- Acute onset of severe headache. May be described as the worst headache of the patient's life. Depending on the location of hemorrhage, may be associated with new fixed neurologic deficit. In unruptured brain AVMs, the risk of spontaneous hemorrhage may be as low as 1% per year. After a first rupture, the annual bleeding risk may increase to more than 5%.[3]
- Seizure (46%)
- Headache (34%)
- Progressive neurologic deficit (21%)
- May be caused by mass effect or venous dilatations. Presence and nature of deficit depend on location of lesion and the draining veins.[4]
- Pediatric patients
- Heart failure
- Macrocephaly
- Prominent scalp veins
Genetics
Can occur due to autosomal dominant diseases, such as Hereditary Hemorrhagic Telangiectasia.[citation needed]
Pathophysiology
In a normal functioning human body, arteries carry blood away from the heart to the lungs or the rest of the body, where the blood passes through capillaries, and veins return the blood to heart. An AVM interferes with this process by forming a direct connection of the arteries and veins. AVMs can cause intense pain and lead to serious medical problems. Although AVMs are often associated with the brain and spinal cord, they can develop in any part of the body.
Arteries and veins are part of the human cardiovascular system. Normally, the arteries in the vascular system carry oxygen-rich blood, except in the case of the pulmonary artery. Structurally, arteries divide and sub-divide repeatedly, eventually forming a sponge-like capillary bed. Blood moves through the capillaries, giving up oxygen and taking up waste products, including CO
2, from the surrounding cells. Capillaries in turn successively join together to form veins that carry blood away. The heart acts to pump blood through arteries and uptake the venous blood.
An AVM lacks the dampening effect of capillaries on the blood flow; it also causes the surrounding area to be deprived of the functions of the capillaries — removal of CO2 and delivery of nutrients to the cells. The resulting tangle of blood vessels, often called a nidus (Latin for "nest"), has no capillaries. It can be extremely fragile and prone to bleeding because of the abnormally direct connections between high-pressure arteries and low-pressure veins. The resultant sign, audible via stethoscope, is a rhythmic, whooshing sound caused by excessively rapid blood flow through the arteries and veins. It has been given the term "bruit", French for noise. On some occasions a patient with a brain AVM may become aware of the noise, which can compromise hearing and interfere with sleep in addition to causing psychological distress.
Diagnosis

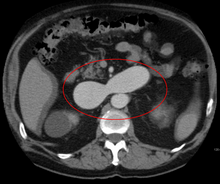
AVMs can occur in various parts of the body:
- brain,
- spleen[5]
- lung[6]
- kidney[7]
- spinal cord[8]
- liver[9]
- intercostal space[10]
- iris[11]
- spermatic cord[12]
AVMs may occur in isolation or as a part of another disease (for example, Von Hippel-Lindau disease or hereditary hemorrhagic telangiectasia).
AVMs have been shown to be associated with Aortic Stenosis.[13]
Bleeding from an AVM can be relatively mild or devastating. It can cause severe and less often fatal strokes. If a cerebral AVM is detected before a stroke occurs, usually the arteries feeding blood into the nidus can be closed off to avert the danger. However, interventional therapy may also be relatively risky
Treatment
Treatment for brain AVMs can be symptomatic, and patients should be followed by a neurologist for any seizures, headaches or focal deficits. AVM-specific treatment may also involve endovascular embolization, neurosurgery or radiation therapy.[2] Embolization, that is, cutting off the blood supply to the AVM with coils or particles or glue introduced by a radiographically guided catheter, can be used in addition to either, but is rarely successful in isolation except for in smaller AVMs. The neurological risk of any such intervention is roughly 10%.
The Spetzler-Martin grading system developed at the Barrow Neurological Institute is utilized by neurosurgeons to determine operative versus nonoperative management of AVMs.
Epidemiology
The estimated detection rate of AVM in the US general population is 1.4/100,000 per year.[14] This is approximately one fifth to one seventh the incidence of intracranial aneurysms. An estimated 300,000 Americans have AVMs, of whom 12% (approximately 36,000) will exhibit symptoms of greatly varying severity.[2]
Society and culture
- American basketball player AJ Price nearly died from AVM in 2004 while a student at the University of Connecticut.
- On December 13, 2006, Senator Tim Johnson was diagnosed with AVM and treated at George Washington University Hospital.[15]
- On August 3, 2011, Mike Patterson of the Philadelphia Eagles collapsed on the field and suffered a seizure during a practice. After he collapsed, Patterson was rushed to the hospital where he was diagnosed with AVM.[16]
- Six Feet Under, an American television series that ran on HBO from 2001–2005, featured a protagonist, Nate Fisher, that suffered from AVM, a recurring feature in the storyline of this character.
- In the episode DNR of the TV series House M.D., the patient was finally diagnosed with an AVM.
- In the episode "Save Me" of season 1 of the TV series "Grey's Anatomy", the psychic was diagnosed with an AVM on his left temporal lobe.
- On August 1, 2007, NIH/NINDS decides to launch the first international study evaluating the best treatment strategy for patients with unruptured brain AVMs: ARUBA — A Randomized trial of Unruptured Brain AVMs, which was stopped in spring of 2013.[17]
- Actor Ricardo Montalbán was born with spinal AVM.[18] During the filming of the 1951 film Across the Wide Missouri, Montalbán was thrown from his horse, knocked unconscious, and trampled by another horse which aggravated his AVM and resulted in a painful back injury that never healed. The pain increased as he aged, and in 1993, Montalbán underwent 9½ hours of spinal surgery which left him paralysed below the waist and using a wheelchair.[19][20]
- Actor/comedian T. J. Miller was diagnosed with AVM while on the set of Yogi Bear in New Zealand in 2010; Miller experienced becoming more philosophical, narrating his behaviors, and inability to sleep during that time. He was soon flown back to Los Angeles and successfully underwent surgery that had a mortality rate of ten percent.[21]
- On August 20, 2012 Sydney Wood got AVM and died. She was an 11 year old from Hamilton, Ontario.[22]
Research directions
Despite many years of research, the central question of whether to treat AVMs has not been answered. All treatments, whether involving surgery, radiation, or drugs, have risks and side-effects. Therefore, it might be better in some cases to avoid treatment altogether and simply accept a small risk of coming to harm from the AVM itself. This question is currently being addressed in clinical trials.[23][dead link]
See also
References
- ^ National Institute of Neurological Disorders and Stroke
- ^ a b c Arteriovenous Malformation Information Page at NINDS
- ^ Stapf C, Mast H, Sciacca RR; et al. (2006). "Predictors of hemorrhage in patients with untreated brain arteriovenous malformation". Neurology. 66 (9): 1350–5. doi:10.1212/01.wnl.0000210524.68507.87. PMID 16682666.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Choi JH, Mast H, Hartmann A; et al. (2009). "Clinical and morphological determinants of focal neurological deficits in patients with unruptured brain arteriovenous malformation". J. Neurol. Sci. 287 (1–2): 126–30. doi:10.1016/j.jns.2009.08.011. PMC 2783734. PMID 19729171.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Agrawal A, Whitehouse R, Johnson RW, Augustine T (2006). "Giant splenic artery aneurysm associated with arteriovenous malformation". J. Vasc. Surg. 44 (6): 1345–9. doi:10.1016/j.jvs.2006.06.049. PMID 17145440. Retrieved 2008-06-01.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Chowdhury UK, Kothari SS, Bishnoi AK, Gupta R, Mittal CM, Reddy S (2008). "Successful Lobectomy for Pulmonary Arteriovenous Malformation Causing Recurrent Massive Haemoptysis". Heart Lung Circ. 18 (2): 135–9. doi:10.1016/j.hlc.2007.11.142. PMID 18294908. Retrieved 2008-06-01.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Barley FL, Kessel D, Nicholson T, Robertson I (2006). "Selective embolization of large symptomatic iatrogenic renal transplant arteriovenous fistula". Cardiovasc Intervent Radiol. 29 (6): 1084–7. doi:10.1007/s00270-005-0265-z. PMID 16794894.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kishi K, Shirai S, Sonomura T, Sato M (2005). "Selective conformal radiotherapy for arteriovenous malformation involving the spinal cord". Br J Radiol. 78 (927): 252–4. doi:10.1259/bjr/50653404. PMID 15730991.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Bauer T, Britton P, Lomas D, Wight DG, Friend PJ, Alexander GJ (1995). "Liver transplantation for hepatic arteriovenous malformation in hereditary haemorrhagic telangiectasia". J. Hepatol. 22 (5): 586–90. doi:10.1016/0168-8278(95)80455-2. PMID 7650340. Retrieved 2008-06-01.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Rivera PP, Kole MK, Pelz DM, Gulka IB, McKenzie FN, Lownie SP (2006). "Congenital intercostal arteriovenous malformation". AJR Am J Roentgenol. 187 (5): W503–6. doi:10.2214/AJR.05.0367. PMID 17056881.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Shields JA, Streicher TF, Spirkova JH, Stubna M, Shields CL (2006). "Arteriovenous malformation of the iris in 14 cases". Arch. Ophthalmol. 124 (3): 370–5. doi:10.1001/archopht.124.3.370. PMID 16534057.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Sountoulides P, Bantis A, Asouhidou I, Aggelonidou H (2007). "Arteriovenous malformation of the spermatic cord as the cause of acute scrotal pain: a case report". J Med Case Reports. 1: 110. doi:10.1186/1752-1947-1-110. PMC 2194703. PMID 17939869.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Batur, P.; Stewart, WJ; Isaacson, JH (2003). "Increased Prevalence of Aortic Stenosis in Patients with Arteriovenous Malformations of the Gastrointestinal Tract in Heyde Syndrome". Archives of Internal Medicine. 163 (15): 1821–4. doi:10.1001/archinte.163.15.1821. PMID 12912718.
- ^ Stapf C, Mast H, Sciacca RR; et al. (2003). "The New York Islands AVM Study: design, study progress, and initial results". Stroke. 34 (5): e29–33. doi:10.1161/01.STR.0000068784.36838.19. PMID 12690217.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ "Sen. Johnson recovering after brain surgery". AP. December 14, 2006.
- ^ "Mike Patterson's Collapse Reportedly Related To Brain AVM"
- ^ Clinical trial number NCT00389181 for "A Randomized Trial of Unruptured Brain AVMs (ARUBA)" at ClinicalTrials.gov
- ^ "Ricardo Montalban tribute" YouTube, acceptance speech video of Easter Seals Lifetime Achievement Award
- ^ Mahalo Answers: Ricardo Montalban
- ^ NNDB: Ricardo Montalban
- ^ Pete Holmes (October 27, 2011). "You Made It Weird with Pete Holmes". You Made It Weird #2: TJ Miller (Podcast). Nerdist Industries. Event occurs at 37:45. Retrieved December 5, 2012.
- ^ http://www.thespec.com/sports-story/2254246-young-hamilton-athlete-s-sudden-death-devastates-community/
- ^ Research trials in arterio-venous malformations; Rustam Al-Shahi Salman
External links
- AVM Support Groups from the DMOZ Open Directory.
- University of California San Francisco AVM research.
