Iodine deficiency: Difference between revisions
| Line 62: | Line 62: | ||
Iodine may also help prevent diseases of the oral and salivary glands.<ref>{{cite pmid | 19835108 }}</ref> |
Iodine may also help prevent diseases of the oral and salivary glands.<ref>{{cite pmid | 19835108 }}</ref> |
||
==Extrathyroidal iodine== |
|||
Iodine accounts for 65% of the molecular weight of T4 and 59% of the T3. 15–20 mg of iodine is concentrated in thyroid tissue and hormones, but 70% of the body's iodine is distributed in other tissues, including mammary glands, eyes, gastric mucosa, the cervix, and salivary glands. In the cells of these tissues iodide enters directly by [[sodium-iodide symporter]] (NIS). Its role in mammary tissue is related to fetal and neonatal development, but its role in the other tissues is unknown.<ref name="Patrick2008" /> It has been shown to act as an antioxidant in these tissues.<ref name="Patrick2008" /> |
|||
The US Food and Nutrition Board and Institute of Medicine recommended daily allowance of iodine ranges from 150 micrograms /day for adult humans to 290 micrograms /day for lactating mothers. However, the thyroid gland needs no more than 70 micrograms /day to synthesize the requisite daily amounts of T4 and T3. These higher recommended daily allowance levels of iodine seem necessary for optimal function of a number of body systems, including lactating breast, gastric mucosa, salivary glands, oral mucosa, thymus, epidermis, choroid plexus, etc.<ref>{{cite journal|url=http://physrev.physiology.org/cgi/reprint/41/1/189.pdf|author=Brown-Grant, K.|year=1961|title=Extrathyroidal iodide concentrating mechanisms|journal= Physiol Rev.|volume= 41|page=189}}</ref><ref>{{cite journal|author=Spitzweg, C., Joba, W., Eisenmenger, W. and Heufelder, A.E. |year=1998|title=Analysis of human sodium iodide symporter gene expression in extrathyroidal tissues and cloning of its complementary deoxyribonucleic acid from salivary gland, mammary gland, and gastric mucosa|journal= J Clin Endocrinol Metab.|volume= 83|page=1746|doi=10.1210/jc.83.5.1746}}</ref><ref>{{cite journal|author=Banerjee, R.K., Bose, A.K., Chakraborty, t.K., de, S.K. and datta, A.G. |year=1985|title= Peroxidase catalysed iodotyrosine formation in dispersed cells of mouse extrathyroidal tissues|journal= J Endocrinol.|volume= 2|page= 159}}</ref> |
|||
Moreover, iodine can add to double bonds of docosahexaenoic acid and arachidonic acid of cellular membranes, making them less reactive to free oxygen radicals.<ref>Cocchi, M. and Venturi, S. Iodide, antioxidant function and Omega-6 and Omega-3 fatty acids: a new hypothesis of a biochemical cooperation? Progress in Nutrition, 2000, 2, 15-19</ref> |
|||
===Iodine deficiency and cancer risk=== |
===Iodine deficiency and cancer risk=== |
||
Revision as of 18:03, 29 October 2010
This article needs additional citations for verification. (March 2008) |
| Iodine deficiency |
|---|
Iodine is an essential trace element; the thyroid hormones thyroxine and triiodotyronine contain iodine. In areas where there is little iodine in the diet—typically remote inland areas where no marine foods are eaten—iodine deficiency gives rise to goiter (so-called endemic goiter), as well as cretinism, which results in developmental delays and other health problems. While noting recent progress, The Lancet noted, "According to WHO, in 2007, nearly 2 billion individuals had insufficient iodine intake, a third being of school age. ... Thus iodine deficiency, as the single greatest preventable cause of mental retardation, is an important public-health problem."[1]
In some such areas, this is now combatted by the addition of small amounts of iodine to table salt in form of sodium iodide, potassium iodide, and/or potassium iodate—this product is known as iodized salt. Iodine compounds have also been added to other foodstuffs, such as flour, water and milk in areas of deficiency.[2] Seafood is also a well known source of iodine.[3] Thus, iodine deficiency is more common in mountainous regions of the world where food is grown in soil poor in iodine.
Signs and symptoms
Goiter
A low amount of thyroxine (one of the two thyroid hormones) in the blood, due to lack of dietary iodine to make it, gives rise to high levels of thyroid stimulating hormone TSH, which stimulates the thyroid gland to increase many biochemical processes; the cellular growth and proliferation can result in the characteristic swelling or hyperplasia of the thyroid gland, or goiter. In mild iodine deficiency, levels of triiodiothyronine (T3) may be elevated in the presence of low levels of levothyroxine, as the body converts more of the levothyroxine to triiodothyronine as a compensation. Some such patients may have a goiter, without an elevated TSH. The introduction of iodized salt since the early 1900s has eliminated this condition in many affluent countries; however, in Australia, New Zealand, and several European countries, iodine deficiency is a significant public health problem.[4] It is more common in third-world nations. Public health initiatives to lower the risk of cardiovascular disease have resulted in lower discretionary salt use at the table, and with a trend towards consuming more processed foods. The noniodized salt used in these foods also means that people are less likely to obtain iodine from adding salt during cooking.
Goiter is said to be endemic when the prevalence in a population is > 5%, and in most cases goiter can be treated with iodine supplementation. If goiter is untreated for around five years, however, iodine supplementation or thyroxine treatment may not reduce the size of the thyroid gland because the thyroid is permanently damaged.
Cretinism
Iodine deficiency is one of the leading cause of preventable mental retardation worldwide, producing typical reductions in IQ of 10 to 15 IQ points. It has been speculated that deficiency of iodine and other micronutrients may be a possible factor in observed differences in IQ between ethnic groups: see race and intelligence for a further discussion of this controversial issue.
Cretinism is a condition associated with iodine deficiency and goiter, commonly characterised by mental deficiency, deaf-mutism, squint, disorders of stance and gait, stunted growth and hypothyroidism. Paracelsus was the first to point out the relation between goitrous parents and mentally retarded children.[5] As a result of restricted diet, isolation, intermarriage, etc., as well as low iodine content in their food, children often had peculiar stunted bodies and retarded mental faculties, a condition later known to be associated with thyroid deficiency. Diderot, in his 1754 Encyclopédie, described these patients as "crétins". In French, the term "crétin des Alpes" also became current, since the condition was observed in remote valleys of the Alps in particular. The word cretin appeared in English in 1779.
Deficiency
In areas where there is little iodine in the diet, typically remote inland areas and semi-arid equatorial climates where no marine foods are eaten, iodine deficiency gives rise to hypothyroidism, symptoms of which are extreme fatigue, goitre, mental slowing, depression, weight gain, and low basal body temperatures.[6]
Iodine deficiency is the leading cause of preventable mental retardation, a result which occurs primarily when babies or small children are rendered hypothyroidic by a lack of the element. The addition of iodine to table salt has largely eliminated this problem in the wealthier nations, but as of March 2006, iodine deficiency remained a serious public health problem in the developing world.[7] Iodine deficiency is also a problem in certain areas of Europe. In Germany it has been estimated to cause a billion dollars in health care costs per year.[8]
Iodine may also help prevent diseases of the oral and salivary glands.[9]
Extrathyroidal iodine
Iodine accounts for 65% of the molecular weight of T4 and 59% of the T3. 15–20 mg of iodine is concentrated in thyroid tissue and hormones, but 70% of the body's iodine is distributed in other tissues, including mammary glands, eyes, gastric mucosa, the cervix, and salivary glands. In the cells of these tissues iodide enters directly by sodium-iodide symporter (NIS). Its role in mammary tissue is related to fetal and neonatal development, but its role in the other tissues is unknown.[8] It has been shown to act as an antioxidant in these tissues.[8]
The US Food and Nutrition Board and Institute of Medicine recommended daily allowance of iodine ranges from 150 micrograms /day for adult humans to 290 micrograms /day for lactating mothers. However, the thyroid gland needs no more than 70 micrograms /day to synthesize the requisite daily amounts of T4 and T3. These higher recommended daily allowance levels of iodine seem necessary for optimal function of a number of body systems, including lactating breast, gastric mucosa, salivary glands, oral mucosa, thymus, epidermis, choroid plexus, etc.[10][11][12] Moreover, iodine can add to double bonds of docosahexaenoic acid and arachidonic acid of cellular membranes, making them less reactive to free oxygen radicals.[13]
Iodine deficiency and cancer risk
- Breast cancer. The breast strongly and actively concentrates iodine into breast-milk for the benefit of the developing infant, and may develop a goiter-like hyperplasia, sometimes manifesting as fibrocystic breast disease, when iodine level are low. Studies indicate that iodine deficiency, either dietary or pharmacologic, can lead to breast atypia and increased incidence of malignancy in animal models, while iodine treatment can reverse dysplasia.[14][15][16] Laboratory evidences demonstrate that the effect of iodine on breast cancer is in part independent of thyroid function and that iodine inhibits cancer promotion through modulation of the estrogen pathway. Gene array profiling of estrogen responsive breast cancer cell line shows that the combination of iodine and iodide alters gene expression and inhibits the estrogen response through up-regulating proteins involved in estrogen metabolism. Whether iodine/iodide will be useful as an adjuvant therapy in the pharmacologic manipulation of the estrogen pathway in women with breast cancer has not been determined clinically.[14]
- Iodine and stomach cancer. Some researchers have found an epidemiologic correlation between iodine deficiency, iodine-deficient goitre and gastric cancer;[17][18][19] a decrease of the incidence of death rate from stomach cancer after implementation of the effective iodine-prophylaxis has been reported also.[20] The proposed mechanism of action is that iodide ion can function in gastric mucosa as an antioxidant reducing species that can detoxify poisonous reactive oxygen species, such as hydrogen peroxide.
Epidemiology
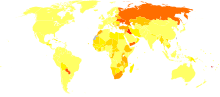
Certain areas of the world, due to natural deficiency and governmental inaction, are severely affected by iodine deficiency, which affects approximately two billion people worldwide. It is particularly common in Western Pacific, South-East Asia and Africa.
India is the most outstanding, with 100 million suffering from deficiency, 4 million from goiter, and 0.5 million from cretinism.[22]
Among other nations affected by iodine deficiency, China and Kazakhstan have begun taking action, while Russia has not. Successful campaigns for the adoption of the use of iodized salt require education and regulation of salt producers and sellers and a communication campaign directed at the public, the salt trade, politicians and policy makers. The cost of adding iodine to salt is negligible—"Only a few cents a ton."[22]
Iodine deficiency has largely been confined to the developing world for several generations, but reductions in salt consumption and changes in dairy processing practices eliminating the use of iodine-based disinfectants have led to increasing prevalence of the condition in Australia and New Zealand in recent years. A proposal to mandate the use of iodized salt in most commercial breadmaking is expected to be adopted in 2009.[23][24]
See also
- Basil Hetzel
- Lugol's iodine
- "Iodine Deficiency: studies by dr. Sebastiano Venturi (Italy)". Retrieved 2008-05-15.
References
- ^ The Lancet (12 July 2008). "Iodine deficiency—way to go yet". The Lancet. 372 (9633): 88. doi:10.1016/S0140-6736(08)61009-0. PMID 18620930. Retrieved 2008-12-05.
{{cite journal}}: Check date values in:|date=(help) - ^ François Delange, Basil Hetzel. "The Iodine Deficiency Disorders". Thyroid Disease Manager.
- ^ Iodine in Seaweed
- ^ Andersson M, Takkouche B, Egli I, Allen HE, de Benoist B (2005). "Current global iodine status and progress over the last decade towards the elimination of iodine deficiency". Bull. World Health Organ. 83 (7): 518–25. PMC 2626287. PMID 16175826.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ T. E. C. Jr. M.D. (August 1, 1974). "Paracelsus on What the Physician Should Know". Pediatrics. 54 (2). American Academy of Pediatrics: 141. Retrieved 2008-12-05.
{{cite journal}}: Italic or bold markup not allowed in:|journal=(help) - ^ Felig, Philip (2001). "Endemic Goiter". Endocrinology & metabolism. McGraw-Hill Professional. ISBN 9780070220010.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Micronutrients - Iodine, Iron and Vitamin A". UNICEF.
- ^ a b c Cite error: The named reference
Patrick2008was invoked but never defined (see the help page). - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19835108 , please use {{cite journal}} with
|pmid= 19835108instead. - ^ Brown-Grant, K. (1961). "Extrathyroidal iodide concentrating mechanisms" (PDF). Physiol Rev. 41: 189.
- ^ Spitzweg, C., Joba, W., Eisenmenger, W. and Heufelder, A.E. (1998). "Analysis of human sodium iodide symporter gene expression in extrathyroidal tissues and cloning of its complementary deoxyribonucleic acid from salivary gland, mammary gland, and gastric mucosa". J Clin Endocrinol Metab. 83: 1746. doi:10.1210/jc.83.5.1746.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Banerjee, R.K., Bose, A.K., Chakraborty, t.K., de, S.K. and datta, A.G. (1985). "Peroxidase catalysed iodotyrosine formation in dispersed cells of mouse extrathyroidal tissues". J Endocrinol. 2: 159.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Cocchi, M. and Venturi, S. Iodide, antioxidant function and Omega-6 and Omega-3 fatty acids: a new hypothesis of a biochemical cooperation? Progress in Nutrition, 2000, 2, 15-19
- ^ a b Stoddard II, F. R. (2008). "Iodine Alters Gene Expression in the MCF7 Breast Cancer Cell Line: Evidence for an Anti-Estrogen Effect of Iodine". International Journal of Medical Science. 5 (4): 189. PMC 2452979. PMID 18645607.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Eskin, B. A. (1995). "Different tissue responses for iodine and iodide in rat thyroid and mammary glands". Bioligal Trace Elements Research. 49 (5): 9. doi:10.1007/BF02788999. PMID 14965610.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: extra punctuation (link) - ^ Venturi, S.; Grotkowski, CE; Connolly, CP; Ghent, WR (2001). "Is there a role for iodine in breast diseases?". The Breast. 10 (1): 379. doi:10.1054/brst.2000.0267. PMID 7577324.
- ^ Josefssson, M.; Ekblad, E. (2009). "Sodium Iodide Symporter (NIS) in Gastric Mucosa: Gastric Iodide Secretion". In Preedy, Victor R.; Burrow, Gerard N.; Watson, Ronald (eds.). Comprehensive Handbook of Iodine: Nutritional, Biochemical, Pathological and Therapeutic Aspects
{{cite book}}: CS1 maint: postscript (link) - ^ Abnet CC, Fan JH, Kamangar F, Sun XD, Taylor PR, Ren JS, Mark SD, Zhao P, Fraumeni JF Jr, Qiao YL, Dawsey SM (2006). "Self-reported goiter is associated with a significantly increased risk of gastric noncardia adenocarcinoma in a large population-based Chinese cohort". International Journal of Cancer. 119 (6): 1508–1510. doi:10.1002/ijc.21993. PMID 16642482.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Behrouzian, R.; Aghdami, N. (2004). "Urinary iodine/creatinine ratio in patients with stomach cancer in Urmia, Islamic Republic of Iran". East Mediterr Health J. 10 (6): 921–924. PMID 16335780
{{cite journal}}: CS1 maint: postscript (link). - ^ Golkowski F, Szybinski Z, Rachtan J, Sokolowski A, Buziak-Bereza M, Trofimiuk M, Hubalewska-Dydejczyk A, Przybylik-Mazurek E, Huszno B. (2007). "Iodine prophylaxis--the protective factor against stomach cancer in iodine deficient areas". Eur J Nutr. 46 (5): 251. doi:10.1007/s00394-007-0657-8. PMID 17497074.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002.
- ^ a b "In Raising the World’s I.Q., the Secret's in the Salt", article by Donald G. McNeil, Jr., The New York Times, December 16, 2006.
- ^ "Iodine plan no help for mums-to-be", article appearing in April 23, 2008, from Herald Sun.
- ^ "Nutritionist supports switch to iodised bread, article by Rebecca Gardiner, April 3, 2008, Howick and Pakuranga Times
External links
- International Council for the Control of Iodine Deficiency Disorders
- Can Africa meet the goal of eliminating iodine-deficiency disorders by the year 2000?
- Kotwal A, Priya R, Qadeer I (2007). "Goiter and other iodine deficiency disorders: A systematic review of epidemiological studies to deconstruct the complex web". Arch. Med. Res. 38 (1): 1–14. doi:10.1016/j.arcmed.2006.08.006. PMID 17174717.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
This template is no longer used; please see Template:Endocrine pathology for a suitable replacement
