IgA nephropathy
| Berger's disease (IgA nephropathy) | |
|---|---|
| Other names | IgA nephritis |
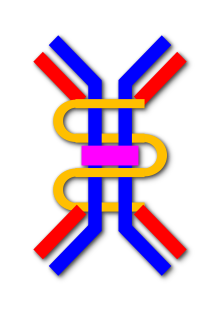 | |
| Immunoglobulin A dimer | |
| Specialty | Nephrology Rheumatology Oncology |
IgA nephropathy (IgAN), also known as Berger's disease (/bɛərˈʒeɪ/) (and variations), or synpharyngitic glomerulonephritis, is a disease of the kidney (or nephropathy) and the immune system; specifically it is a form of glomerulonephritis or an inflammation of the glomeruli of the kidney. Aggressive Berger's disease (a rarer form of the disease) can attack other major organs, such as the liver, skin and heart.
IgA nephropathy is the most common glomerulonephritis worldwide; however, aggressive Berger's disease is on the NORD list of rare diseases.[1] Primary IgA nephropathy is characterized by deposition of the IgA antibody in the glomerulus. There are other diseases associated with glomerular IgA deposits, the most common being IgA vasculitis (formerly known as Henoch–Schönlein purpura [HSP]), which is considered by many to be a systemic form of IgA nephropathy.[2] IgA vasculitis presents with a characteristic purpuric skin rash, arthritis, and abdominal pain, and occurs more commonly in young adults (16–35 years old). HSP is associated with a more benign prognosis than IgA nephropathy. In non-aggressive IgA nephropathy there is traditionally a slow progression to chronic kidney failure in 25–30% of cases during a period of 20 years.
Signs and symptoms
The classic presentation for the non-aggressive form (in 40–50% of the cases) is episodic hematuria, which usually starts within a day or two of a non-specific upper respiratory tract infection (hence synpharyngitic), as opposed to post-streptococcal glomerulonephritis, which occurs some time (weeks) after initial infection. With both aggressive and non-aggressive Berger's disease loin pain can also occur. The gross hematuria may resolve after a few days, though microscopic hematuria will persist, it is however more common with aggressive Berger's disease for gross hematuria to persist rather than microscopic hematuria. Renal function usually remains normal with non-aggressive Berger's disease, though rarely acute kidney failure may occur (see below). This presentation is more common in younger adults.
The following is a basic list of symptoms taken primarily from Mayo clinic;
- Severe flank/abdominal pain
- High blood pressure
- Hematuria (gross, frank, microscopic)
- Compromised immune system
- Edema in hands and feet
- Cola- or tea-colored urine
A smaller proportion (20–30%), usually the older population, have microscopic hematuria and proteinuria (less than 2 gram/day). These patients may be asymptomatic and only picked up due to urinalysis. Hence, the disease is more commonly diagnosed in situations where screening of urine is compulsory (e.g., schoolchildren in Japan).
Very rarely (5% each), the presenting history is:
- Nephrotic syndrome (3–3.5 grams of protein loss in the urine, associated with a poorer prognosis)
- Acute kidney failure (either as a complication of the frank hematuria, when it usually recovers, or due to rapidly progressive glomerulonephritis which often leads to chronic kidney failure)
- Chronic kidney failure (no previous symptoms, presents with anemia, hypertension and other symptoms of kidney failure, in people who probably had longstanding undetected microscopic hematuria and/or proteinuria)
A variety of systemic diseases are associated with aggressive IgA nephropathy (Berger's disease) such as liver failure, cancer, celiac disease, systemic lupus erythematosus, rheumatoid arthritis, heart failure, reactive arthritis, ankylosing spondylitis and HIV. Diagnosis of Berger's disease and a search for any associated disease occasionally reveals such an underlying serious systemic disease. Occasionally, there are simultaneous symptoms of Henoch–Schönlein purpura; see below for more details on the association. Some HLA alleles have been suspected along with complement phenotypes as being genetic factors. Non-aggressive Berger's disease may also be associated with any of the above systemic diseases, however this is rare.
Morphology
Histologically, IgA nephropathy may show mesangial widening and focal and segmental inflammation. Diffuse mesangial proliferation or crescentic glomerulonephritis may also be present. Immunoflourescence shows mesangial deposition of IgA often with C3 and properdin and smaller amounts of other immunoglobulins (IgG or IgM). Early components of the classical complement pathway (C1q or C4) are usually not seen. Electron microscopy confirms electron-dense deposits in the mesangium that may extend to the subendothelial area of adjacent capillary walls in a small subset of cases, usually those with focal proliferation.
Pathophysiology
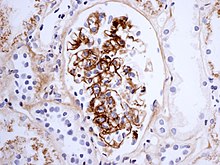
The disease derives its name from deposits of immunoglobulin A (IgA) in a granular pattern in the mesangium (by immunofluorescence), a region of the renal glomerulus. The mesangium by light microscopy may be hypercellular and show increased deposition of extracellular matrix proteins. In terms of the renal manifestation of Henoch–Schönlein purpura, it has been found that although it shares the same histological spectrum as IgA nephropathy, a greater frequency of severe lesions such as glomerular necrosis and crescents were observed. Correspondingly, HSP nephritis has a higher frequency of glomerular staining for fibrin compared with IgAN, but with an otherwise similar immunofluorescence profile.[3]
There is no clear known explanation for the accumulation of the IgA. Exogenous antigens for IgA have not been identified in the kidney, but it is possible that this antigen has been cleared before the disease manifests itself. It has also been proposed that IgA itself may be the antigen.
A recently advanced theory focuses on abnormalities of the IgA1 molecule. IgA1 is one of the two immunoglobulin subclasses (the other is IgD) that is O-glycosylated on a number of serine and threonine residues in a special proline-rich hinge region. Aberrant glycosylation of IgA appears to lead to polymerisation of the IgA molecules in tissues, especially the glomerular mesangium.[4] A similar mechanism has been claimed to underlie Henoch–Schönlein purpura, a vasculitis that mainly affects children and can feature renal involvement that is almost indistinguishable from IgA nephritis. However, human studies have found that degalactosylation of IgA1 occurs in patients with IgA nephropathy in response only to gut antigen exposures (not systemic), and occurs in healthy people to a lesser extent.[5] This strongly suggests degalactosylation of IgA1 is a result of an underlying phenomenon (abnormal mucosal antigen handling) and not the ultimate cause of IgA nephropathy. Prevailing evidence suggests that both galactose-deficient o-glycans in the hinge region of IgA1 and synthesis and binding of antibodies against IgA1 are required for immunoglobulin complexes to form and accumulate in glomeruli.[6]
From the fact that IgAN can recur after renal transplant, it can be postulated that the disease is caused by a problem in the immune system rather than the kidney itself. Remarkably, the IgA1 that accumulates in the kidney does not appear to originate from the mucosa-associated lymphoid tissue (MALT), which is the site of most upper respiratory tract infections, but from the bone marrow. This, too, suggests an immune pathology rather than direct interference by outside agents.
Natural history
Since IgA nephropathy commonly presents without symptoms through abnormal findings on urinalysis, there is considerable possibility for variation in any population studied depending upon the screening policy. Similarly, the local policy for performing kidney biopsy assumes a critical role; if it is a policy to simply observe patients with isolated bloody urine, a group with a generally favourable prognosis will be excluded. If, in contrast, all such patients are biopsied, then the group with isolated microscopic hematuria and isolated mesangial IgA will be included and ‘improve’ the prognosis of that particular series.
Nevertheless, IgA nephropathy, which was initially thought to be a benign disease, has been shown to not be a benign disease, particularly if the patient presents with an aggressive form. Though most reports describe Berger's disease as having an indolent evolution towards either healing or renal damage, a more aggressive course is occasionally seen associated with extensive crescents, and presenting as acute kidney failure. In general, the entry into chronic kidney failure is slow as compared to most other glomerulonephritides – occurring over a time scale of 30 years or more (in contrast to the 5 to 15 years in other glomerulonephritides), however in aggressive Berger's disease the time scale is within 5–10 years and often sooner. This may reflect the earlier diagnosis made due to frank hematuria.
Complete remission of aggressive Berger's disease, occurs rarely in adults. In about 5% of cases, however, there is a higher chance of remission with non-aggressive Berger's disease (this is estimated to be around 7.4% of cases). There is a high chance of relapse particularly with aggressive Berger's disease. However, given the evolution of this disease, the longer term (10–20 years) outcome of such patients is not yet established.
Overall, the current 10 year survival rate for aggressive Berger's disease is 25% and 73% for non-aggressive Berger's disease.
Diagnosis
For an adult patient with isolated hematuria, tests such as ultrasound of the kidney and cystoscopy are usually done first to pinpoint the source of the bleeding. These tests would rule out kidney stones and bladder cancer, two other common urological causes of hematuria. In children and younger adults, the history and association with respiratory infection can raise the suspicion of IgA nephropathy. A kidney biopsy is necessary to confirm the diagnosis. The biopsy specimen shows proliferation of the mesangium, with IgA deposits on immunofluorescence and electron microscopy. However, patients with isolated microscopic hematuria (i.e. without associated proteinuria and with normal kidney function) are not usually biopsied since this is associated with an excellent prognosis. A urinalysis will show red blood cells, usually as red cell urinary casts. Proteinuria, usually less than 2 grams per day, also may be present. Other renal causes of isolated hematuria include thin basement membrane disease and Alport syndrome, the latter being a hereditary disease associated with hearing impairment and eye problems.
Other blood tests done to aid in the diagnosis include CRP or ESR, complement levels, ANA, and LDH. Protein electrophoresis and immunoglobulin levels can show increased IgA in 50% of all patients.
Treatment
The ideal treatment for IgAN would remove IgA from the glomerulus and prevent further IgA deposition. This goal still remains a remote prospect. There are a few additional caveats that have to be considered while treating IgA nephropathy. IgA nephropathy has a very variable course, ranging from a benign recurrent hematuria up to a rapid progression to chronic kidney failure and failure of other major organs. Hence the decision on which patients to treat should be based on the prognostic factors and the risk of progression. Also, IgA nephropathy recurs in transplants despite the use of ciclosporin, azathioprine or mycophenolate mofetil, cyclophosphamide, Isotretinoin and steroids in these patients. There are persisting uncertainties, due to the limited number of patients included in the few controlled, randomized, studies performed to date. These studies hardly produce statistically significant evidence regarding the heterogeneity of IgA nephropathy patients, the diversity of study treatment protocols, and the length of follow-up.
In cases where tonsillitis is the precipitating factor for episodic hematuria, a tonsillectomy has been claimed to reduce the frequency of those episodes. However, it does not reduce the incidence of progressive kidney failure.[7] Dietary gluten restriction, used to reduce mucosal antigen challenge, also has not been shown to preserve kidney function. Phenytoin has also been tried without any benefit.[8]
A subset of IgA nephropathy patients, who have minimal change disease on light microscopy and clinically have nephrotic syndrome, show an exquisite response to steroids, behaving more or less like minimal change disease. In other patients, the evidence for steroids is not compelling. Short courses of high dose steroids have been proven to lack benefit. However, in patients with aggressive Berger's disease 6 months regimen of steroids in addition to other medications may lessen proteinuria and preserve renal function.[9] The study had 10 years of patient follow-up data, and did show a benefit for steroid therapy; there was a lower chance of reaching end-stage renal disease (renal function so poor that dialysis was required) in the steroid group. Importantly, angiotensin-converting enzyme inhibitors were used in both groups equally.
Cyclophosphamide (traded as endoxan & cytoxan) and Isotretinoin have commonly been used, often with anti-platelet/anticoagulants in patients with Aggressive Berger's disease, however, the side effect profile of these drugs, including long term risk of malignancy and sterility, made them an unfavorable choice for use in young adults. However, one recent study, in a carefully selected high risk population of patients with declining GFR, showed that a combination of steroids and cyclophosphamide for the initial 3 months followed by azathioprine for a minimum of 2 years resulted in a significant preservation of renal function.[10] Other agents such as mycophenolate mofetil, ciclosporin and mizoribine have also been tried with varying results.
A study from Mayo Clinic did show that long term treatment with omega-3 fatty acids results in slight reduction of progression to kidney failure, without, however, reducing proteinuria in a subset of patients with high risk of worsening kidney function.[11] However, these results have not been reproduced by other study groups and in two subsequent meta-analyses.[12][13] However, fish oil therapy does not have the drawbacks of immunosuppressive therapy. Also, apart from its unpleasant taste and abdominal discomfort, it is relatively safe to consume.
The events that tend to progressive kidney failure are not unique to IgA nephropathy and non-specific measures to reduce the same would be equally useful. These include low-protein diet and optimal control of blood pressure. The choice of the antihypertensive agent is open as long as the blood pressure is controlled to desired level. However, Angiotensin converting enzyme inhibitors and Angiotensin II receptor antagonists are favoured due to their anti-proteinuric effect.
Prognosis
Male gender, proteinuria (especially > 2 g/day), hypertension, smoking, hyperlipidemia, older age, familial disease and elevated creatinine concentrations are markers of a poor outcome. Frank hematuria has shown discordant results with most studies showing a better prognosis, perhaps related to the early diagnosis, except for one group which reported a poorer prognosis. Proteinuria and hypertension are the most powerful prognostic factors in this group.[14]
There are certain other features on kidney biopsy such as interstitial scarring which are associated with a poor prognosis. ACE gene polymorphism has been recently shown to have an impact with the DD genotype associated more commonly with progression to kidney failure.
Epidemiology
Men are affected three times as often as women. There is also marked geographic variation in the prevalence of IgA nephropathy throughout the world. It is the most common glomerular disease in the Far East and Southeast Asia, accounting for almost half of all the patients with glomerular disease.[citation needed] However, it accounts for only about 25% of the proportion in Europeans and about 10% among North Americans, with African–Americans having a very low prevalence of about 2%.[citation needed] A confounding factor in this analysis is the existing policy of screening and use of kidney biopsy as an investigative tool. School children in Japan undergo routine urinalysis (as do army recruits in Singapore) and any suspicious abnormality is pursued with a kidney biopsy, which might partly explain the high observed incidence of IgA nephropathy in those countries.
Genetics
Though various associations have been described, no consistent pattern pointing to a single susceptible gene has been identified to date. Associations described include those with C4 null allele, factor B Bf alleles, MHC antigens and IgA isotypes. ACE gene polymorphism (D allele) is associated with progression of kidney failure, similar to its association with other causes of chronic kidney failure. However, more than 90% of cases of IgA nephropathy are sporadic, with a few large pedigrees described from Kentucky and Italy (Online Mendelian Inheritance in Man (OMIM): 161950).
History

William Heberden, the elder, first described the disease in 1801 in a 5-year-old child with abdominal pain, hematuria, hematochezia, and purpura of the legs.[15] In 1837, Johann Lukas Schönlein described a syndrome of purpura associated with joint pain and urinary precipitates in children. Eduard Heinrich Henoch, a student of Schönlein's, further associated abdominal pain and renal involvement with the syndrome.
In 1968, Jean Berger (1930–2011), a pioneering French nephrologist, with co-author, the electron microscopist Nicole Hinglais, was the first to describe IgA deposition in this form of glomerulonephritis and therefore it is sometimes called Berger’s disease.[16]
References
- ^ D'Amico, G (1987). "The commonest glomerulonephritis in the world: IgA nephropathy". Q J Med. 64 (245): 709–27. PMID 3329736.
- ^ C, Davin J (2001). "What is the difference between IgA nephropathy and Henoch-Schönlein purpura nephritis?". Kidney International. 59 (3): 823–34. doi:10.1046/j.1523-1755.2001.059003823.x. PMID 11231337.
- ^ Magistroni, Riccardo (2015). "New developments in the genetics, pathogenesis, and therapy of IgA nephropathy". Kidney International. 88 (5): 974–89. doi:10.1038/ki.2015.252. PMC 4653078. PMID 26376134.
- ^ Maverakis E, Kim K, Shimoda M, Gershwin M, Patel F, Wilken R, Raychaudhuri S, Ruhaak LR, Lebrilla CB (2015). "Glycans in the immune system and The Altered Glycan Theory of Autoimmunity". J Autoimmun. 57 (6): 1–13. doi:10.1016/j.jaut.2014.12.002. PMC 4340844. PMID 25578468.
- ^ Smith AC, Molyneux K, Feehally J, Barratt J (2006). "O-glycosylation of serum IgA1 antibodies against mucosal and systemic antigens in IgA nephropathy". J Am Soc Nephrol. 17 (12): 3520–28. doi:10.1681/ASN.2006060658. PMID 17093066.
- ^ Suzuki, Hitoshi; Kiryluk, Krzysztof; Novak, Jan; Moldoveanu, Zina; Herr, Andrew; Renfrow, Matthew; Wyatt, Robert; Scolari, Francesco; Mestecky, Jiri; Gharavi, Ali; Julian, Bruce (October 1, 2011). "The Pathophysiology of IgA Nephropathy". Journal of the American Society of Nephrology. 22 (10): 1795–1803. doi:10.1681/ASN.2011050464. PMC 3892742. PMID 21949093.
- ^ Xie Y, Chen X, Nishi S, Narita I, Gejyo F (2004). "Relationship between tonsils and IgA nephropathy as well as indications of tonsillectomy". Kidney Int. 65 (4): 1135–44. doi:10.1111/j.1523-1755.2004.00486.x. PMID 15086452.
- ^ Clarkson AR, Seymour AE, Woodroffe AJ, McKenzie PE, Chan YL, Wootton AM (1980). "Controlled trial of phenytoin therapy in IgA nephropathy". Clin. Nephrol. 13 (5): 215–18. PMID 6994960.
- ^ Kobayashi Y, Hiki Y, Kokubo T, Horii A, Tateno S (1996). "Steroid therapy during the early stage of progressive IgA nephropathy. A 10-year follow-up study". Nephron. 72 (2): 237–42. doi:10.1159/000188848. PMID 8684533.
- ^ Ballardie FW, Roberts IS (2002). "Controlled prospective trial of prednisolone and cytotoxics in progressive IgA nephropathy". J. Am. Soc. Nephrol. 13 (1): 142–48. PMID 11752031.
- ^ Donadio JV, Bergstralh EJ, Offord KP, Spencer DC, Holley KE (1994). "A controlled trial of fish oil in IgA nephropathy. Mayo Nephrology Collaborative Group". N. Engl. J. Med. 331 (18): 1194–99. doi:10.1056/NEJM199411033311804. PMID 7935657.
- ^ Strippoli GF, Manno C, Schena FP (2003). "An "evidence-based" survey of therapeutic options for IgA nephropathy: assessment and criticism". Am. J. Kidney Dis. 41 (6): 1129–39. doi:10.1016/S0272-6386(03)00344-5. PMID 12776264.
- ^ Dillon JJ (1997). "Fish oil therapy for IgA nephropathy: efficacy and interstudy variability". J. Am. Soc. Nephrol. 8 (11): 1739–44. PMID 9355077.
- ^ Bartosik LP, Lajoie G, Sugar L, Cattran DC (2001). "Predicting progression in IgA nephropathy". Am. J. Kidney Dis. 38 (4): 728–35. doi:10.1053/ajkd.2001.27689. PMID 11576875.
- ^ Heberden W. Commentarii Di Morborium Historia et Curatione. London: Payne, 1801.
- ^ Berger J, Hinglais N (1968). "Les depots intercapillaires d'IgA-IgG". J Urol Nephrol. 74: 694–95.
External links
