Cataract surgery: Difference between revisions
Pbsouthwood (talk | contribs) |
Pbsouthwood (talk | contribs) →Uses: copied content from lead of https://en.wikipedia.org/w/index.php?title=Cataract&oldid=1141241574 as basis for summary section. See that page's history for attribution. |
||
| Line 21: | Line 21: | ||
==Uses== |
==Uses== |
||
{{main|Cataract}} |
|||
Removal of opacified lens of the eye ([[cataract]]) as [[definitive treatment]] for vision impairment due to lens opacification, usually including insertion of a [[prosthetic]] [[intraocular lens]] to restore focus within a useful range of distances.<ref name="Statpearls" /> |
Removal of opacified lens of the eye ([[cataract]]) as [[definitive treatment]] for vision impairment due to lens opacification, usually including insertion of a [[prosthetic]] [[intraocular lens]] to restore focus within a useful range of distances.<ref name="Statpearls" /> |
||
<!-- Definition and symptoms --> |
|||
A cataract is a cloudy area in the [[lens (anatomy)|lens]] of the [[eye]] that causes to a [[visual impairment|decrease in vision]].<ref name=NIH2009/><ref name=":0" /> Cataracts often develop slowly and can affect one or both eyes.<ref name=NIH2009/> Symptoms may include faded colors, blurry or [[double vision]], halos around light, trouble with bright lights, and [[Nyctalopia|difficulty seeing at night]].<ref name="NIH2009">{{cite web |date=September 2009 |title=Facts About Cataract |url=http://www.nei.nih.gov/health/cataract/cataract_facts |url-status=live |archive-url=https://web.archive.org/web/20150524095805/https://www.nei.nih.gov/health/cataract/cataract_facts |archive-date=24 May 2015 |access-date=24 May 2015}}</ref> This may result in trouble driving, reading, or recognizing faces.<ref name="Allen-2006">{{cite journal | vauthors = Allen D, Vasavada A | title = Cataract and surgery for cataract | journal = BMJ | volume = 333 | issue = 7559 | pages = 128–132 | date = July 2006 | pmid = 16840470 | pmc = 1502210 | doi = 10.1136/bmj.333.7559.128 }}</ref> Poor vision caused by cataracts may also result in an increased risk of [[Falling (accident)|falling]] and [[Depression (mood)|depression]].<ref name=Gim2011>{{cite journal | vauthors = Gimbel HV, Dardzhikova AA | title = Consequences of waiting for cataract surgery | journal = Current Opinion in Ophthalmology | volume = 22 | issue = 1 | pages = 28–30 | date = January 2011 | pmid = 21076306 | doi = 10.1097/icu.0b013e328341425d | s2cid = 205670956 }}</ref> Cataracts cause 51% of all cases of [[blindness]] and 33% of [[visual impairment]] worldwide.<ref name=WHO2014>{{cite web|title=Visual impairment and blindness Fact Sheet N°282|url=https://www.who.int/mediacentre/factsheets/fs282/en/|access-date=23 May 2015|date=August 2014|url-status=live|archive-url=https://web.archive.org/web/20150512062236/http://www.who.int/mediacentre/factsheets/fs282/en/|archive-date=12 May 2015}}</ref><ref name=WHO2012Data>{{cite book|title=Global Data on Visual Impairments 2010|date=2012|publisher=WHO|page=6|url=https://www.who.int/blindness/GLOBALDATAFINALforweb.pdf?ua=1|url-status=live|archive-url=https://web.archive.org/web/20150331221058/http://www.who.int/blindness/GLOBALDATAFINALforweb.pdf?ua=1|archive-date=2015-03-31}}</ref> |
|||
<!-- Cause, mechanisms and diagnosis --> |
|||
Cataracts are most commonly due to [[senescence|aging]] but may also occur due to [[Trauma (medicine)|trauma]] or radiation exposure, be [[congenital cataract|present from birth]], or occur following eye surgery for other problems.<ref name=NIH2009/><ref name=WHOPri>{{cite web|title=Priority eye diseases|url=https://www.who.int/blindness/causes/priority/en/index1.html|access-date=24 May 2015|url-status=dead|archive-url=https://web.archive.org/web/20150524095804/http://www.who.int/blindness/causes/priority/en/index1.html|archive-date=24 May 2015}}</ref> Risk factors include [[diabetes mellitus|diabetes]], longstanding use of [[corticosteroid]] medication, [[smoking tobacco]], prolonged exposure to [[sunlight]], and [[Alcohol (drug)|alcohol]].<ref name=NIH2009/> The underlying mechanism involves accumulation of clumps of [[protein]] or yellow-brown pigment in the lens that reduces transmission of light to the [[retina]] at the back of the eye.<ref name=NIH2009/> Diagnosis is by an [[eye examination]].<ref name=NIH2009/> |
|||
<!-- Prevention and treatment --> |
|||
Prevention includes wearing [[sunglasses]] and a wide brimmed hat, eating leafy vegetables and fruits,{{clarify|claim not supported in main section on prevention|date=February 2023}} and avoiding smoking.<ref name=NIH2009/><ref name="NIH News in Health 2017 on cataract">{{cite web | title=Recognizing Cataracts | website=NIH News in Health | date=2017-05-30 | url=https://newsinhealth.nih.gov/2013/08/recognizing-cataracts | access-date=2020-02-02 | quote=Try wearing sunglasses or a hat with a brim. Researchers also believe that good nutrition can help reduce the risk of age-related cataract. They recommend eating plenty of green leafy vegetables, fruits, nuts and other healthy foods.}}</ref> Early on the symptoms may be improved with [[glasses]].<ref name=NIH2009/> If this does not help, [[cataract surgery|surgery to remove the cloudy lens and replace it with an artificial lens]] is the only effective treatment.<ref name=NIH2009/> Cataract surgery is not readily available in many countries, and surgery is needed only if the cataracts are causing problems and generally results in an improved [[quality of life]].<ref name=NIH2009/><ref>{{cite journal | vauthors = Lamoureux EL, Fenwick E, Pesudovs K, Tan D | title = The impact of cataract surgery on quality of life | journal = Current Opinion in Ophthalmology | volume = 22 | issue = 1 | pages = 19–27 | date = January 2011 | pmid = 21088580 | doi = 10.1097/icu.0b013e3283414284 | s2cid = 22760161 }}</ref><ref name=WHOPri/><ref name=Rao2011/> |
|||
<!-- Epidemiology --> |
|||
About 20 million people worldwide are blind due to cataracts.<ref name=WHOPri/> It is the cause of approximately 5% of blindness in the United States and nearly 60% of blindness in parts of Africa and South America.<ref name=Rao2011>{{cite journal | vauthors = Rao GN, Khanna R, Payal A | title = The global burden of cataract | journal = Current Opinion in Ophthalmology | volume = 22 | issue = 1 | pages = 4–9 | date = January 2011 | pmid = 21107260 | doi = 10.1097/icu.0b013e3283414fc8 | s2cid = 205670997 }}</ref> Blindness from cataracts occurs in about 10 to 40 per 100,000 children in the [[Developing country|developing world]], and 1 to 4 per 100,000 children in the [[developed world]].<ref name=":0">{{cite book| vauthors = Pandey SK |title=Pediatric cataract surgery techniques, complications, and management|date=2005|publisher=Lippincott Williams & Wilkins|location=Philadelphia|isbn=978-0781743075|page=20|url=https://books.google.com/books?id=gLJZDD2igCMC&pg=PA20|url-status=live|archive-url=https://web.archive.org/web/20150524134557/https://books.google.ca/books?id=gLJZDD2igCMC&pg=PA20|archive-date=2015-05-24}}</ref> Cataracts become more common [[Ageing|with age]].<ref name=NIH2009/> In the United States, cataracts occur in 68% of those over the age of 80 years.<ref name = NEI2019>{{Cite web|url=https://www.nei.nih.gov/learn-about-eye-health/resources-for-health-educators/eye-health-data-and-statistics/cataract-data-and-statistics|title=Cataract Data and Statistics {{!}} National Eye Institute|website=www.nei.nih.gov|access-date=2019-11-18}}</ref> Additionally they are more common in women, and less common in Hispanic and Black people.<ref name = NEI2019/> |
|||
==Contraindications== |
==Contraindications== |
||
Revision as of 05:43, 24 February 2023
| Cataract surgery | |
|---|---|
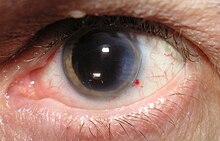
 Magnified view of a cataract in a human eye seen on examination with a slit lamp | |
| Specialty | Ophthalmology |
| ICD-9-CM | 13.19 |
| MeSH | D002387 |
| MedlinePlus | 002957 |
Cataract surgery, also called lens replacement surgery, is the removal of the natural lens of the eye (also called "crystalline lens") that has developed an opacification, which is referred to as a cataract,[1] and usually its replacement with an artificial intraocular lens.
Metabolic changes of the crystalline lens fibers over time lead to the development of the cataract, causing impairment or loss of vision. Some infants are born with congenital cataracts, and certain environmental factors may also lead to cataract formation. Early symptoms may include strong glare from lights and small light sources at night, and reduced visual acuity at low light levels.
During cataract surgery, the cloudy natural lens is removed, either by emulsification in place or by cutting it out. An artificial intraocular lens (IOL) is usually implanted in its place. Cataract surgery is generally performed by an ophthalmologist in an out-patient setting at a surgical center or hospital rather than an in-patient setting. Local anesthesia is normally used, and the procedure usually causes little or no pain and minor discomfort to the patient.[2]
Well over 90% of operations are successful in restoring useful vision, with a low complication rate. Day care, high volume, minimally invasive, small incision phacoemulsification with quick post-operative recovery has become the standard of care in cataract surgery all over the developed world.[3] Manual small incision cataract surgery (MSICS) is popular in the developing world, as it is considerably more economical in time, capital equipment and consumables, while providing comparable results.[4] Both procedures are low risk for serious complications.[5]
Uses
Removal of opacified lens of the eye (cataract) as definitive treatment for vision impairment due to lens opacification, usually including insertion of a prosthetic intraocular lens to restore focus within a useful range of distances.[3]
A cataract is a cloudy area in the lens of the eye that causes to a decrease in vision.[6][7] Cataracts often develop slowly and can affect one or both eyes.[6] Symptoms may include faded colors, blurry or double vision, halos around light, trouble with bright lights, and difficulty seeing at night.[6] This may result in trouble driving, reading, or recognizing faces.[8] Poor vision caused by cataracts may also result in an increased risk of falling and depression.[9] Cataracts cause 51% of all cases of blindness and 33% of visual impairment worldwide.[10][11]
Cataracts are most commonly due to aging but may also occur due to trauma or radiation exposure, be present from birth, or occur following eye surgery for other problems.[6][12] Risk factors include diabetes, longstanding use of corticosteroid medication, smoking tobacco, prolonged exposure to sunlight, and alcohol.[6] The underlying mechanism involves accumulation of clumps of protein or yellow-brown pigment in the lens that reduces transmission of light to the retina at the back of the eye.[6] Diagnosis is by an eye examination.[6]
Prevention includes wearing sunglasses and a wide brimmed hat, eating leafy vegetables and fruits,[clarification needed] and avoiding smoking.[6][13] Early on the symptoms may be improved with glasses.[6] If this does not help, surgery to remove the cloudy lens and replace it with an artificial lens is the only effective treatment.[6] Cataract surgery is not readily available in many countries, and surgery is needed only if the cataracts are causing problems and generally results in an improved quality of life.[6][14][12][15]
About 20 million people worldwide are blind due to cataracts.[12] It is the cause of approximately 5% of blindness in the United States and nearly 60% of blindness in parts of Africa and South America.[15] Blindness from cataracts occurs in about 10 to 40 per 100,000 children in the developing world, and 1 to 4 per 100,000 children in the developed world.[7] Cataracts become more common with age.[6] In the United States, cataracts occur in 68% of those over the age of 80 years.[16] Additionally they are more common in women, and less common in Hispanic and Black people.[16]
Contraindications
Contraindications to cataract surgery include cataracts that do not cause visual impairment, and medical conditions that predict a high risk of unsatisfactory surgical outcomes.[3]
Technique

Two main types of surgical procedures are in common use throughout the world. The first procedure is phacoemulsification (phaco), a method in which the lens is broken into small pieces which are removed by suction, and the second involves two different types of extracapsular cataract extraction (ECCE), in which the lens is removed from its capsule and removed in one piece. In most surgeries, an intraocular lens is inserted. Foldable lenses are generally used for the 2–3 mm phaco incision, while non-foldable lenses are placed through the larger extracapsular incision. The small incision size used in phacoemulsification (2–3 mm) often allows sutureless incision closure. ECCE uses a larger incision (10–12 mm) and therefore usually requires stitching, and this in part led to the modification of ECCE known as manual small incision cataract surgery (MSICS).[3]
Cataract extraction using intracapsular cataract extraction (ICCE) has been superseded by phacoemulsification and ECCE, and is rarely performed.[3]
Phacoemulsification is the most commonly performed cataract procedure in the developed world. However, the high cost of a phacoemulsification machine and of the associated disposable equipment means that ECCE and MSICS remain the most commonly performed procedures in developing countries.[3]
Cataract surgery is commonly done as day care rather than in-patient procedure as it is cheaper than hospitalisation and overnight stay, and there is evidence that day surgery has similar medical outcomes.[17]
Types of surgery

There are a number of different surgical techniques used in cataract surgery:
- Phacoemulsification (phaco) is the most common technique used in developed countries. It involves the use of a machine with an ultrasonic handpiece equipped with a titanium or steel tip. The tip vibrates at ultrasonic frequency (commonly 40,000 Hz) to emulsify the lens tissue. A second fine instrument (sometimes called a "cracker" or "chopper") may be used from a side port to facilitate breaking the hard cataract nucleus into smaller pieces. Fragmentation into smaller pieces makes emulsification, and the aspiration of cortical material (the soft part of the lens around the nucleus) easier. After phacoemulsification of the lens nucleus and cortical material is completed, a dual irrigation-aspiration (I-A) probe or a bimanual I-A system is used to remove the remaining peripheral cortical material.
- The manual small incision cataract surgery (MSICS) technique is an evolution of ECCE (see below) where the entire lens is removed from the eye through a self-sealing scleral tunnel wound. An appropriately constructed scleral tunnel is held closed by internal pressure, is watertight, and does not require suturing. The "small" in the title refers to the wound being relatively smaller than in ECCE, although it is still markedly larger than a phaco wound. Head-to-head trials of MSICS vs phaco in dense cataracts have found no difference in outcomes, but shorter operating time and significantly lower costs with MSICS.[4]
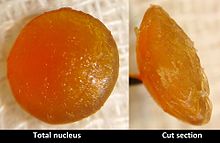
- Extracapsular cataract extraction (ECCE), (also known as manual extracapsular cataract extraction) is the removal of almost the entire natural lens in one piece, while the elastic lens capsule (posterior capsule) is left intact to allow implantation of an intraocular lens.[3] It involves manual expression of the lens through a large (usually 10–12 mm) incision made in the cornea or sclera. Although it requires a larger incision and the use of stitches, this method may be indicated for patients with very hard cataracts or other situations in which phacoemulsification is problematic.
- Intracapsular cataract extraction (ICCE) is the removal of the lens and the surrounding lens capsule in one piece. The procedure has a relatively high rate of complications due to the large incision required and pressure placed on the vitreous body. It has therefore been largely superseded and is rarely performed in countries where operating microscopes and high-technology equipment are readily available.[3] After lens removal by ICCE, an artificial plastic lens (an intraocular lens implant) can be placed in either the anterior chamber or sutured into the sulcus.
Cryoextraction is a technique used in ICCE in which the cataract is extracted using a cryoprobe, the refrigerated tip of which adheres to the tissue of the lens at the contact point by freezing with a cryogenic substance such as liquid nitrogen, facilitating its removal.[18] It is now used primarily for the removal of subluxated lenses. - Femtosecond laser-assisted cataract surgery has been reported to be safe, and may have less adverse effect on the cornea and macula than manual phacoemulsification. The laser is used to make the corneal incision, the capsulotomy and to initiate lens fragmentation, which reduces the energy requirements for phacoemulsification. It offers high precision, effective lens fragmentation at lower power levels and good optical quality, but as of 2022 has not been shown to have significant visual, refractive or safety benefit over manual phacoemulsification, and it has a higher cost.[3][19][20]
- Refractive lens exchange is effectively the same procedure used to replace a lens with high refractive error when other methods are not effective. There are risks in addition to cataract procedural risks.[3] A related procedure is the implantation of phakic intraocular lenses in series with the natural lens to correct vision in cases of high refractive errors.[21]
Ophthalmic viscosurgical devices
Ophthalmic viscosurgical devices (OVDs) are a class of clear gel like material used in cataract surgery to maintain the volume and shape of the anterior chamber of the eye, and protect the intraocular tissues during the procedure. They were originally called viscoelastic substances, or just viscoelastics. Their consistency allows the surgical instruments to move through them, but when there is low shear stress they do not flow, and retain their shape. OVDs are available in several formulations which may be combined or used individually as best suits the procedure, and are introduced into the anterior chamber at the start of the procedure, and removed at the end, when they are replaced by a buffered saline solution.[5] The tendency of cohesive OVDs to adhere to themselves helps with removal.[22]
Intraocular lenses

After the removal of the cataract, an intraocular lens (IOL) is usually implanted into the eye, either through a small incision (1.8 mm to 2.8 mm) when using a foldable IOL, or through a larger incision, when using a rigid poly(methyl methacrylate) (PMMA) lens. The foldable IOL, made of silicone, hydrophobic, or hydrophilic acrylic material of appropriate refractive power is folded either using a holder/folder, or a proprietary insertion device provided along with the IOL.[23] The lens implant is inserted through the incision, usually into the capsular bag within the posterior chamber (in-the-bag implantation). Sometimes, a sulcus implantation (in front or on top of the capsular bag but behind the iris) may be required because of posterior capsular tears or because of zonulodialysis. Implantation of posterior chamber intraocular lens (PCIOL) in patients below 7 months of age is controversial due to rapid ocular growth at this age and the excessive amount of inflammation, which may be very difficult to control. Optical correction in these patients without intraocular lens (aphakic) is usually managed with either special contact lenses or glasses. Secondary implantation of IOL (placement of a lens implant as a second operation) may be considered later. Other designs of multifocal intraocular lens are also available, which focus light from distant as well as near objects, working with similar effect to bifocal or trifocal eyeglasses. Preoperative patient selection and good counselling is necessary to avoid unrealistic expectations and post-operative patient dissatisfaction, and possibly a requirement to replace the lens.[24] Acceptability of these lenses has improved and studies have shown good results in patients selected for expected compatibility.[25]
An accommodating lens made by Eyeonics,[26] now Bausch & Lomb, was approved by the US FDA in 2003. The Crystalens has two hinged struts on opposite edges which displace the lens along the optical axis when an inward transverse force is applied to the haptic loops at the outer ends of the struts (the components transferring the movement of the contact points to the device), and it springs back when the force is reduced. It is implanted in the eye's lens capsule, where the contractions of the ciliary body which would focus the eye with the natural lens are used to focus the implant.[27][3]
The intraocular lenses used in correcting astigmatism have different curvature on two orthogonal axes, as on the surface of a torus, and are called toric lenses. The STAAR Surgical Intraocular Lens was the first such lens developed in the United States and it may correct up to 3.5 diopters. A different model of toric lenses was created by Alcon and may correct up to 3 diopters of astigmatism. In order to achieve the most benefit from a toric lens, the surgeon must place the lens to suit the axes to the patient's astigmatism. Intraoperative wavefront analysis, can be used to assist the surgeon in toric lens placement and minimize astigmatic errors.[28]
Monofocal intraocular lenses provide accurately focused vision at one distance only: far, intermediate, or near. Patients who are fitted with these lenses may need to wear eyeglasses or contact lenses for reading or using a computer. These lenses usually have uniform spherical curvature.[29][30]
Cataract surgery may be performed to correct vision problems in both eyes, and in these cases, if both eyes are suitable, patients are usually advised to consider monovision. This procedure involves inserting in one eye an intraocular lens that provides near vision and in the other eye an IOL that provides distance vision. Although most patients can adjust to having implanted monofocal lenses with differing focal length, some cannot compensate and may experience blurred vision at both near and far distances. An IOL optimised for distance vision may be combined with an IOL that optimises intermediate vision instead of near vision as a variation of monovision.[23]
Bausch and Lomb developed the first aspheric IOLs in 2004, which provide better contrast sensitivity by having their periphery flatter than the middle of the lens. The effectiveness of aspheric IOLs depends on a range of conditions, and they may not always provide significant benefit.[31]
Some IOLs provide ultraviolet and high energy blue light absorbption. The natural crystalline lens of the eye filters these potentially harmful frequencies. According to a few studies though, these lenses have been associated with a decrease in vision quality.[citation needed][clarification needed] A Cochrane review of 2018 found that there is unlikely to be a significant difference in distance vision between blue-filtering and plain lenses, and were unable to identify a difference in contrast sensitivity or colour discrimination.[32][33]
Another type of intraocular lens is the light-adjustable IOL, which was approved by the FDA in 2017.[34] This particular type of IOL is implanted in the eye and then treated with ultraviolet light of a certain wavelength in order to alter the curvature of the lens.[35]
In some cases, surgeons may opt for inserting an additional lens over the already implanted one, also in the posterior capsule. This type of IOL placement is called "piggyback" IOLs and is usually considered an option whenever the visual result of the first implant is not optimal.[36] In such cases, implanting another IOL over the existing one is considered safer than replacing the initial lens. This approach may also be used in patients who need high degrees of vision correction.[37]
Whichever type is used, the appropriate refractive power of the IOL (much like an eyeglass prescription) must be selected to provide the desired refractive outcome. Traditionally, preoperative measurements including corneal curvature, axial length, and white to white measurements are used to estimate the required power of the IOL. These methods include several formulas, including Hagis,[38] Hoffer Q,[38] Holladay 1,[38] Holladay 2,[38] and SRK/T[39]. There are also free online calculators using similar input data.[38] A histoty of LASIK surgery requires different calculations to take this into account.[38] Refractive results using traditional power calculation formulas leave patients within 0.5D (diopters) of target (correlates to 20/25 when targeted for distance) in 55% of cases and within 1D (correlates to 20/40 when targeted for distance) in 85% of cases. Developments in intraoperative wavefront technology have demonstrated power calculations that provide improved outcomes, yielding 80% of patients within 0.5D (20/25 or better).[citation needed]
Statistically, cataract surgery and IOL implantation are procedures with the safest and highest success rates in eye care.[5] However, as with any type of surgery, some level of risk remains. The cost is another important aspect of these lenses. Although most insurance companies cover the costs of monofocal IOLs, patients may have to pay the price difference if they choose more expensive lenses.[40]
Preoperative evaluation
An eye examination or pre-operative evaluation by an eye surgeon is necessary to confirm the presence of a cataract and to determine if the patient is a suitable candidate for surgery. The patient must fulfill certain requirements such as:
- The degree of reduction of vision due, at least in large part, to the cataract should be evaluated. While the existence of other sight-threatening diseases, such as age-related macular degeneration or glaucoma, does not preclude cataract surgery, less improvement may be expected in their presence.[3]
- The eyes should have a normal pressure, or any pre-existing glaucoma should be adequately controlled with medications. In cases of uncontrolled glaucoma, a combined cataract-glaucoma procedure (phaco-trabeculectomy) can be planned and performed.[41]
- The pupil should be adequately dilated using eyedrops; if pharmacologic pupil dilation is inadequate, procedures for mechanical pupillary dilatation may be needed during the surgery.[42]
- Patients with retinal detachment may be scheduled for a combined vitreo-retinal procedure, along with PCIOL implantation.[43]
- It has been shown that patients taking tamsulosin (Flomax), a common drug for enlarged prostate, are prone to developing a surgical complication known as intraoperative floppy iris syndrome (IFIS), which must be correctly managed to avoid the complication posterior capsule rupture; however, prospective studies have shown that the risk is greatly reduced if the surgeon is informed of the patient's history with the drug beforehand, and has appropriate alternative techniques prepared.[44]
- A Cochrane Review of three randomized clinical trials including over 21,500 cataract surgeries examined whether routine preoperative medical testing resulted in a reduction of adverse events during surgery. Results showed that performing preoperative medical testing did not result in a reduction of risk of intraoperative or postoperative medical adverse events, compared to surgeries with no or limited preoperative testing.[45]
Operation procedures
The two most commonly used procedures are phacoemulsification and manual small incision cataract surgery (MSICS).
Phacoemulsification

The surgical procedure in phacoemulsification for removal of cataract involves a number of steps, and is typically performed under an operating microscope. Each step must be correctly performed to achieve the desired result. The steps may be described as follows:
- Anaesthesia and pupil dilation; Either topical, sub-tenon, peribulbar, or retrobulbar local anesthesia is used, usually causing little or no discomfort to the patient.[46] Topical anesthetic agents are most commonly used and may be placed on the globe as eyedrops prior to surgery and or in the globe during surgery.[47] Local anesthetic injection techniques include sub-conjunctival injections and or injections posterior to the globe (retrobulbar block) to produce a regional nerve block when it is necessary to prevent movement of the eye.[5] Intravenous sedation may be combined with the topical and injection techniques. General anesthesia and retrobulbar blocks were historically used for intracapsular cataract surgery, but for small incision surgery and phacoemulsification local and topical anesthesia is in common use.[3]
- Site preparation by disinfection of the area surrounding the eye, covering the rest of the face, and exposure of the eyeball using an eyelid speculum;[48]
- Entry into the eye through a minimal incision;[5] The incision for cataract surgery has evolved along with the techniques for cataract removal and IOL placement. In phacoemulsification the size depends on the requirements for IOL insertion. A more posterior incision simplifies wound closure and decreases induced astigmatism, but is more likely to damage blood vessels. With foldable IOLs it is sometimes possible to use incisions smaller than 3.5 mm. The shape, position and size of the incision all affect the capacity for self sealing, the tendency to induce astigmatism, and the surgeon's ability to maneuver instruments through the opening.[5] One or two smaller side port incisions 60 to 90 degrees from the main incision may be needed to access the anterior chamber with additional instruments.[48]
- Injection of ophthalmic viscosurgical devices, also known as viscoelastics, into the anterior chamber to support, stabilize and protect the eyeball, to help maintain eye pressurization, and to distend the lens capsule during IOL implantation.[22]
- Capsulorhexis; Making a circular opening on the front surface of the lens to access the lens within. In phacoemulsification, an anterior continuous curvilinear capsulorhexis, is used to create a round and smooth opening through which the lens nucleus can be emulsified and the intraocular lens implant inserted.[49]
- Hydrodissection; The cataract's outer (cortical) layer is separated from the capsule by a gentle continuous flow of liquid from a cannula, injected under the anterior capsular flap;[50][51]
- Hydrodelineation; An injection of fluid into the body of the lens through the cortex against the nucleus of the cataract separates the hardened nucleus from the softer cortex shell by flowing along the interface between them. The smaller hard nucleus can then be more expeditiously phacoemulsified, while the posterior cortex serves as a buffer protecting the posterior capsule membrane. The smaller size of the separated nucleus requires less deep and less peripheral grooving and produces smaller fragments after cracking or chopping. The posterior cortex also maintains the shape of the capsule which reduces risk of posterior capsule rupture[52]
- Ultrasonic destruction or emulsification of the cataract after nuclear cracking or chopping (if needed), careful aspiration of the remaining lens cortex (outer layer of lens) material from the capsular bag, capsular polishing (the removal of all epithelial cells from the capsule), if needed;[53]
- Implantation of the folded intraocular replacement lens, usually into the remaining posterior capsule, and ensuring that it unfolds correctly. Aligning the IOL in the correct axis if a toric IOL;[3]
- Ophthalmic viscosurgical devices removal; The viscoelastic that was injected to stabilize the anterior chamber, protect the cornea from damage, and distend the cataract's capsule during IOL implantation must be removed from the eye to prevent post-operative viscoelastic glaucoma (a severe intra-ocular pressure increase). This is done via suction from the irrigation-aspiration instrument and replacement by buffered saline solution (BSS). Removal of OVD from behind the implant reduces the risk and magnitude of postoperative pressure spikes or capsular distention;[5]
- Wound sealing and hydration. The incision is sealed by elevating the pressure inside the globe with BSS which presses the internal tissue against the external tissue of the incision forcing closed the incision. If this does not achieve a satisfactory seal a suture may be used.[5]
Manual small incision cataract surgery
- The pupil is dilated using drops (if the IOL is to be placed behind the iris) to help better visualise the cataract. Pupil-constricting drops are reserved for secondary implantation of the IOL in front of the iris (if the cataract has already been removed without primary IOL implantation). Anesthesia may be placed topically (eyedrops) or via injection next to (peribulbar) or behind (retrobulbar) the eye.[47] Topical anaesthetics are commonly used at the same time as a intracameral lidocaine injection to reduce pain during the operation.[47] Oral or intravenous sedation may also be used to reduce anxiety. General anesthesia is rarely necessary, but may be employed for children and adults with particular medical or psychiatric issues.[47][5]
- The operation may occur on a stretcher or a reclining examination chair. The eyelids and surrounding skin will be swabbed with disinfectant. The face is covered with a cloth or sheet, with an opening for the operative eye. The eyelid is held open with a speculum to minimize blinking during surgery.[48] Pain is usually minimal in properly anesthetised eyes, though a pressure sensation and discomfort from the bright operating microscope light is common. The ocular surface is kept moist using sterile saline eye drops or methylcellulose viscoelastic.[citation needed]
- The small incision into the anterior chamber of the eye is made at or near the corneal limbus where the cornea and sclera meet. Advantages of the smaller incision include use of few or no stitches and shortened recovery time.[3] The "small" incision is small in comparison with the earlier ECCE incision, but considerably larger than the phaco incision. The precise geometry of the incision is important as it affects the self-sealing of the wound and can cause astigmatism by distortion of the cornea during healing. A sclerocorneal or scleral tunnel incision is commonly used, which reduces induced astigmatism if suitably formed.[4][48]
- A capsulotomy (rarely known as cystotomy) is a procedure to open the surface of the lens capsule, using an instrument called a cystotome.[54] An anterior capsulotomy refers to the opening of the front portion of the lens capsule,[55] whereas a posterior capsulotomy refers to the opening of the back portion of the lens capsule.[56]
- Following cataract removal, an intraocular lens is usually inserted. After the IOL is inserted, the ophthalmic viscosurgery device is aspirated and replaced with BSS and the wound closed. The surgeon checks that the incision does not leak fluid, since wound leakage increases the risk of microorganisms gaining access into the eye and predisposing it to endophthalmitis. An antibiotic/steroid combination eye drop is put in and an eye shield may be applied, sometimes supplemented with an eye patch.[5]
Antibiotics may be administered pre-operatively, intra-operatively, and/or post-operatively. Frequently a topical corticosteroid is used in combination with topical antibiotics post-operatively.[5]
Most cataract operations are performed under a local anaesthetic, allowing the patient to go home the same day. The use of an eye patch may be indicated, usually for some hours and while sleeping, after which the patient is instructed to use anti-inflammatory eyedrops to control inflammation and antibiotic eyedrops to prevent infection. Lens and cataract procedures are commonly performed in an outpatient setting; in the United States, 99.9% of lens and cataract procedures were done in an ambulatory setting in 2012.[57][5]
Occasionally, a peripheral iridectomy may be performed to minimize the risk of pupillary block glaucoma.[5] An opening through the iris can be fashioned manually (surgical iridectomy) or with a laser (called Nd:YAG laser iridotomy). The laser peripheral iridotomy may be performed either prior to or following cataract surgery.[58]
The iridectomy hole is larger when done manually than when performed with a laser. When the manual surgical procedure is performed, some negative side-effects may occur, such as that the opening of the iris can be seen by others (aesthetics), and the light can fall into the eye through the new hole, creating some visual disturbances. In the case of visual disturbances, the eye and brain often learn to compensate and ignore the disturbances over a couple of months. Sometimes the peripheral iris opening can heal, which means that the hole ceases to exist.[58][59]
After the surgery, the patient is instructed to use anti-inflammatory and antibiotic eye-drops for up to two weeks (depending on the inflammation status of the eye and some other variables). The surgeon will judge, based on each patient's idiosyncrasies, the time length to use the eye drops. The eye will be mostly recovered within a week, and complete recovery should be expected in about a month. The patient should not participate in contact/extreme sports until cleared to do so by the eye surgeon.[citation needed]
Complications
Complications can develop during and after surgery.
- Posterior capsular rupture is the most common complication during cataract surgery, with a rate of around 0.5% to 5.2%. This is a rupture of the posterior capsule of the natural lens.[3] Surgical management may involve anterior vitrectomy and, occasionally, alternative planning for implanting the intraocular lens, either in the ciliary sulcus, in the anterior chamber (in front of the iris), or, less commonly, sutured to the sclera. Posterior capsule rupture can cause lens fragments to be retained, corneal edema, and cystoid macular edema. it is also associated with a six-times increase of risk of endophthalmitis and as much as 19 times increase in the risk of retinal detachment.[3][60] Management methods include the Intraocular lens scaffold procedure.[61]
- Suprachoroidal hemorrhage is a rare complication of intraocular surgery where the ciliary arteries bleed into the space between the choroid and the sclera.[62] It is a potentially vision threatening pathology. Risk factors for suprachoroidal hemorrhage include anterior chamber intraocular lens (ACIOL), axial myopia, advanced age, atherosclerosis, glaucoma, systolic hypertension, tachycardia, uveitis, and previous ocular surgery. Immediate and effective management of a suprachoroidal hemorrhage is necessary to protect vision.[5]
- Intraoperative floppy iris syndrome has an incidence of around 0.5% to 2.0%.[3]
- Iris or ciliary body injury has an incidence of about 0.6%-1.2%[3]
- Posterior dislocation of nuclear fragments: In the event of a posterior capsule rupture, fragments of the nucleus can find there way through the tear into the vitreous chamber. It is not always desirable to attempt to recover the fragments and it is rarely successful. The rest of the fragments should generally be stabilised first, and vitreous prevented from entering the anterior chamber. Removal of the fragments may be best referred to a vitreoretinal specialist.[5]
- Failure to aspirate all lens fragments, leaving some in the anterior chamber.[60]
- Incisional burns are caused by overheating of the phacoemulsification tip when ultrasonic power continues while the irrigation or aspiration lines are blocked, as the flow through these lines is used to keep the tip cool. Burns to the incision may make closure difficult and can cause corneal astigmatism.[5]
Complications after cataract surgery are relatively uncommon.
- PVD – Posterior vitreous detachment does not directly threaten vision. Even so, it is of increasing interest because the interaction between the vitreous body and the retina might play a decisive role in the development of major pathologic vitreoretinal conditions. PVD may be more problematic with younger patients, since many patients older than 60 have already gone through PVD. PVD may be accompanied by peripheral light flashes and increasing numbers of floaters.

- Some people develop a posterior capsular opacification (PCO), also called an after-cataract. As a physiological change expected after cataract surgery, the posterior capsular cells undergo hyperplasia and cellular migration, showing up as a thickening, opacification and clouding of the posterior lens capsule (which is left behind when the cataract was removed, for placement of the IOL). This may compromise visual acuity and can be safely and painlessly corrected using a laser device to make small holes in the posterior lens capsule of the crystalline. It usually is a quick outpatient procedure that uses a Nd-YAG laser (neodymium-yttrium-aluminum-garnet) to disrupt and clear the central portion of the opacified posterior pole of the capsule (posterior capsulotomy).[63] This creates a clear central visual axis for improving visual acuity.[64] In very thick opacified posterior capsules, a surgical (manual) capsulectomy may be needed. A YAG capsulotomy is, however, a factor which must be taken in consideration in the event of IOL replacement as vitreous can migrate toward the anterior chamber through the opening hitherto occluded by the IOL. Posterior capsule opacification has an incidence of about 0.3% to 28.4%.[3]
- Retinal detachment normally occurs at a prevalence of 1 in 1,000 (0.1%), but patients who have had cataract surgery are at an increased risk (0.5–0.6%) of developing rhegmatogenous retinal detachment (RRD) – the most common form of retinal detachment.[65] Cataract surgery speeds up the rate of vitreous humor liquefaction and this leads to increased rates of RRD.[66] When a retinal tear occurs, vitreous liquid enters the space between the retina and retinal pigmented epithelium (RPE) and presents as flashes of light (photopsia), dark floaters, and loss of peripheral vision.[65]
- Toxic anterior segment syndrome or TASS is a non-infectious inflammatory condition that may occur following cataract surgery. It is usually treated with topical corticosteroids in high dosage and frequency.[67]
- Endophthalmitis is a serious infection of the intraocular tissues, usually following intraocular surgery complications, or penetrating trauma, and one of the most severe. It is rare in cataract surgery due to the use of prophylactic antibiotics There is some concern that the clear cornea incision might predispose to the increase of endophthalmitis but there is no conclusive study to corroborate this suspicion.[68] An intracameral injection of antibiotics may be used as a preventive measure. A meta-analysis showed the incidence of endophthalmitis after phacoemulsification to be 0.092%. The risk is higher with diabetes, advanced age, vitreous communication[clarification needed] and larger incision procedures.[23] Typical presentation is within two weeks after the procedure with decreased visual acuity, red-eye, and pain. Hypopyon occurs about 80% of the time. Common infective agents include coagulase-negative staphylococci and Staphylococcus aureus in about 80% of infections. Management includes vitreous humor tap and injection of broad-spectrum antibiotics. Outcomes can be severe even with treatment, and may range from permanently decreased visual acuity to no light perception, depending on the microbiological etiology.[3]
- Glaucoma may occur and it may be very difficult to control. It is usually associated with inflammation, especially when little fragments or chunks of the nucleus get access to the vitreous cavity. Some experts recommend early intervention when this condition occurs (posterior pars plana vitrectomy). Neovascular glaucoma may occur, especially in diabetic patients. In some patients, the intraocular pressure may remain so high that blindness may ensue.[citation needed]
- Swelling or edema of the central part of the retina, called macula, resulting in macular edema, can occur a few days or weeks after surgery. Most such cases can be successfully treated. Preventative use of nonsteroidal anti-inflammatory drugs has been reported to reduce the risk of macular edema to some extent.[69]
- Uveitis–glaucoma–hyphema syndrome: This is a complication of cataract surgery caused due to the mechanical irritation of mispositioned intraocular lens over iris, ciliary body or iridocorneal angle.[70]
- Other possible complications include: Swelling or edema of the cornea, sometimes associated with cloudy vision, which may be transient or permanent (pseudophakic bullous keratopathy). Displacement or dislocation of the intraocular lens implant may rarely occur. Unplanned high refractive error (either myopic or hypermetropic) may occur due to error in the ultrasonic biometry (measure of the length and the required intraocular lens power). Cyanopsia, in which the patient sees everything tinted with blue, often occurs for a few days, weeks or months after removal of a cataract. Floaters commonly appear after surgery.[33]
Risk
As of 2011, cataract surgery is the most frequent surgical procedure in the United States, with 1.8 million Medicare beneficiaries undergoing the procedure in 2004. This rate is expected to increase as the population ages. Cataract surgery following modern procedures is safe and effective, but not entirely free of risk.[71]
Most complications of cataract surgery do not result in long-term visual impairment, but there are some severe complications that can result in irreversible blindness.[71] A survey of adverse results affecting Medicare patients recorded between 2004 and 2006 showed an average rate of 0.5% for one or more severe post-operative complications, with the rate decreasing over the study period by about 20%. The most important risk factors identified were diabetic retinopathy, and a combination of cataract surgery with another intraocular procedure on the same day. 97% of the surgeries in the study were not combined with other intraocular procedures. 3% were combined with retinal, corneal or glaucoma surgery on the same day[71]
Recovery and rehabilitation
Side effects such as grittiness, watering, blurred vision, double vision or a red or bloodshot eye may occur, and will usually clear over a few days. Full recovery can take four to six weeks.[72]
It is generally recommended to avoid getting water in the eye during the first week after surgery and to avoid swimming for two to three weeks as a conservative approach, to minimise risk of bacterial infection.[5]
Most patients can return to normal activities the day following phacoemulsification surgery.[73] Depending on the procedure, driving should be avoided for at least 24 hours after the surgery, largely due to effects from the anesthesia, possible swelling affecting focus, and pupil dilation causing excessive glare. At the first post-0perative check, the surgeon will usually be able to confirm whether vision is suitable for driving.[73]
With small-incision self-sealing wounds used with phacoemulsification, some of the post-operative restrictions common with intracapsular and extracapsular procedures are not relevant. Restrictions against lifting and bending were intended to reduce the risk of the wound opening, because straining increases intraocular pressure, but with a self-sealing tunnel incision, higher pressure closes the wound more tightly. Routine use of a shield is also usually not required because inadvertent finger pressure on the eye should not open a correctly structured incision, which should only open to point pressure.[5]
The eyes should not be rubbed after surgery. This can risk contamination, as can the use of eye makeup, face cream or lotions. Situations where there is a lot of dust, wind, pollen or dirt should also be avoided. Sunglasses should be worn on bright days as the eyes will be more sensitive to bright light for a while.[74]
Topical anti-inflammatory drugs and antibiotics are commonly used in the form of eye-drops to reduce the risk of inflammation and infection. A shield or eye-patch may be prescribed to protect the eye while sleeping. The eye will be checked to ensure that the IOL remains in place, and once it has fully stabilised, after about six weeks, vision tests will be done to check whether prescription lenses are needed.[72][3]
Where the focal length of the IOL is optimised for distance vision, reading glasses will generally be needed for near focus.[30]
In some cases the patient is dissatisfied with the optical correction provided by the initial implants, and removal and replacement is necessary. This can occur with the more complex designs of IOL when patient expectations do not match with the compromises inherent in these designs, or the patient cannot accommodate the difference in distance and near focusing of monovision lenses.[24]
History
Cataract surgery has a long history in Europe, Asia and Africa. It is one of the most common and one of the most successful procedures in worldwide use. The success is due to a combination of improvements in techniques for cataract removal and developments in intraocular lens replacement technology, both in the techniques for implantation, and the design, construction and selection of the IOL.[75] Surgical techniques that have contributed to this success include microsurgery, viscoelastics, hypotony, and phacoemulsification.[76]
Couching

Couching is the earliest documented form of cataract surgery, and one of the oldest surgical procedures. It is a technique whereby the lens is dislodged, and pushed aside, but mot removed from the eye, thus removing the opacity, but also the ability to focus. Couching was used for centuries, but it has generally poor outcomes and is currently routinely practiced only in remote areas of developing countries.[77]
Cataract surgery was first mentioned in the Babylonian code of Hammurabi 1750 BCE.[78]
Possibly the first depiction of cataract surgery in recorded history is on a statue from the Fifth Dynasty (2467–2457 BCE).[78] It is further alleged that a "relief painting from tomb number TT 217 in a worker settlement in Deir el-Medina" shows "the man buried in the tomb, Ipuy,... one of the builders of royal tombs in the renowned Valley of the Kings, circa 1279–1213 BC"[79] as he underwent cataract surgery. It is assumed that the couching technique was used.[78]
Couching was practised in ancient India and subsequently introduced to other countries by the Indian physician Sushruta (c. 6th century BCE),[80] who described it in his work the Compendium of Sushruta or Sushruta Samhita. The Uttaratantra section of the Compendium, chapter 17, verses 55–69, describes an operation in which a curved needle was used to push the opaque "phlegmatic matter" (kapha in Sanskrit) in the eye out of the way of vision. The phlegm was then said to be blown out of the nose. The eye would later be soaked with warm clarified butter and then bandaged. Here is a translation from the original Sanskrit:
vv. 55–56: Now procedure of surgical operation of ślaiṣmika liṅganāśa (cataract) will be described. It should be taken up (for treatment) if the diseased portion in the pupillary region is not shaped like half moon, sweat drop or pearl: not fixed, uneven and thin in the centre, streaked or variegated and is not found painful or reddish.
vv. 57–61ab: In moderate season, after unction and sudation, the patient should be positioned and held firmly while gazing at his nose steadily. Now the wise surgeon leaving two parts of white circle from the black one towards the outer canthus should open his eyes properly free from vascular network and then with a barley-tipped rod-like instrument held firmly in hand with middle, index and thumb fingers should puncture the natural hole-like point with effort and confidence not below, above or in sides. The left eye should be punctured with right hand and vice-versa. When punctured properly a drop of fluid comes out and also there is some typical sound.
vv. 61bc–64ab: Just after puncturing, the expert should irrigate the eye with breast-milk and foment it from outside with vāta-[wind-]alleviating tender leaves, irrespective of doṣa [defect] being stable or mobile, holding the instrument properly in position. Then the pupillary circle should be scraped with the tip of the instrument while the patient, closing the nostril of the side opposite to the punctured eye, should blow so that kapha [phlegm] located in the region be eliminated.
vv. 64cd–67: When pupillary region becomes clear like cloudless sun and is painless, it should be considered as scraped properly. (If doṣa [defect] cannot be eliminated or it reappears, puncturing is repeated after unction and sudation.) When the sights are seen properly the śalākā [probe] should be removed slowly, eye anointed with ghee and bandaged. Then the patient should lie down in supine position in a peaceful chamber. He should avoid belching, coughing, sneezing, spitting and shaking during the operation and thereafter should observe the restrictions as after intake of sneha [oil].
v. 68: Eye should be washed with vāta-[wind-]alleviating decoctions after every three days and to eliminate fear of (aggravation of) vāyu [wind], it should also be fomented as mentioned before (from outside and mildly).
v. 69: After observing restrictions for ten days in this way, post-operative measures to normalise vision should be employed along with light diet in proper quantity.[81]
The removal of cataracts by surgery was introduced into China from India, and flourished in the Sui (581–618 CE) and Tang dynasties (618–907 CE).[82]
Galen of Pergamon 2nd century CE, a prominent Greek physician, surgeon and philosopher, performed an operation similar to modern cataract surgery. Using a needle-shaped instrument, Galen attempted to remove a cataract-affected lens.[83][84] Although many 20th century historians have claimed that Galen believed the lens to be in the exact center of the eye, He actually understood that the crystalline lens is located in the anterior aspect of the human eye.[85]
The first references to cataract and its treatment in Europe are found in 29 AD in De Medicinae, the work of the Latin encyclopedist Aulus Cornelius Celsus, which describes a couching operation.[citation needed]
The removal of cataracts by couching was a common surgical procedure in Djenné[86] (as in many other parts of Africa).[87]
Couching continued to be used throughout the Middle Ages and is still used in some parts of Africa and in Yemen.[88] Couching is an ineffective and dangerous method of cataract therapy, and often results in patients remaining blind or with only partially restored vision.[88] For the most part, it has been replaced by extracapsular cataract surgery, including phacoemulsification.[89]
The lens can also be removed by suction through a hollow instrument. Bronze oral suction instruments have been unearthed that seem to have been used for this method of cataract extraction during the 2nd century CE.[90] Such a procedure was described by the 10th-century Persian physician Muhammad ibn Zakariya al-Razi, who attributed it to Antyllus, a 2nd-century Greek physician. The procedure "required a large incision in the eye, a hollow needle, and an assistant with an extraordinary lung capacity".[91] This suction procedure was also described by the Iraqi ophthalmologist Ammar Al-Mawsili, in his Choice of Eye Diseases, also written in the 10th century.[91] He presented case histories of its use, claiming to have had success with it on a number of patients.[91]: p318 Extracting the lens has the benefit of removing the possibility of the lens migrating back into the field of vision.[92] A later variant of the cataract needle in 14th-century Egypt, reported by the oculist Al-Shādhili, used a screw to grip the lens. It is not clear how often, if ever, this method was used, as other writers, including Abu al-Qasim al-Zahrawi and Al-Shadhili, appear to have been unfamiliar with this procedure or claimed it was ineffective.[91]: p319
Eighteenth and nineteenth centuries

In 1748, Jacques Daviel was the first modern European physician to successfully extract cataracts from the eye, removing the cataract from the capsule through a corneal incision with about 50% success rate.[75] In 1753 the first recorded surgical removal of the entire lens and lens capsule was done by Samuel Sharp. The lens was removed from the eye through a limbal incision.[75] In America, cataract couching may have been performed in 1611,[93] and cataract extraction was most likely performed by 1776.[94] Cataract extraction by aspiration of lens material through a tube to which suction is applied was performed by Philadelphia surgeon Philip Syng Physick in 1815.[95]
King Serfoji II Bhonsle of Thanjavur in India performed cataract surgeries in the early 1800s, documented in manuscripts at the Saraswathi Mahal Library.[96]
Twentieth century to present
At the beginning of the 20th century the standard procedure was intracapsular cataract extraction (ICCE). The work of Henry Smith was influential as he had developed a safe and fast way to remove the lens within its capsule by external manipulation. The capsule forceps, the discovery of enzymatic zonulysis by Joaquin Barraquer in 1957, and the introduction of cryoextraction of the lens by T. Krawicz and Charles Kelman, in 1961 helped continue the development of ICCE.[5] Inracapsular cryoextraction using a probe tip cooled by liquid nitrogen to freeze the encapsulated lens to the probe was the favored form of cataract extraction from the late 1960s to the early 1980s.[18][97]
In 1949, Harold Ridley introduced the concept of implantation of the intraocular lens which permitted more efficient and comfortable visual rehabilitation possible after cataract surgery.[75]
Artificial intraocular lenses (IOLs) are used to replace the eye's natural lens that is removed during cataract surgery. These lenses increased in popularity since the 1960s, but it was not until 1981 that the first U.S. Food and Drug Administration (FDA) approval for this type of product was issued. The development of IOLs brought about an innovation as patients previously did not have their natural lens replaced and as a result had to wear very thick eyeglasses or a special type of contact lenses. IOLs can be selected to correct vision problems such as toric lenses for correcting astigmatism.[29] IOLs can be classified as monofocal, toric, and multifocal lenses.[3]
In 1967, Charles Kelman introduced phacoemulsification, a technique that uses ultrasonic energy to emulsify the nucleus of the crystalline lens in order to remove the cataracts without a large incision. This method of surgery decreased the need for an extended hospital stay and made out-patient surgery the standard. Patients who undergo cataract surgery hardly complain of pain or even discomfort during the procedure. However patients who have topical anesthesia, rather than peribulbar block anesthesia, may experience some discomfort.[98] Ophthalmic viscosurgical devices (OVDs) were introduced in 1972, and facilitated the procedure as well as improving safety. An OVD is a viscoelastic solution, a gel-like substance used to maintain the shape of the eye at reduced pressure and to protect the inside structure and tissues of the eye without interfering with the operation.[75]
In the early 1980s Danielle Aron-Rosa and colleagues introduced the neodymium:yttrium-aluminum-garnet laser|neodymium:yttrium-aluminum-garnet (Nd:YAG) laser for posterior capsulotomy.[5]
Thomas Mazzocco developed the first foldable IOL and implanted it in 1985. Graham Barrett and associates pioneered the use of silicone, acrylics, and hydrogels.[5]
According to Cionni et al 2006, Kimiya Shimizu began removing cataracts using topical anesthesia in the late 1980s,[5] though Davis, 2016, attributes the introduction of topical anesthetics to Fischman in 1993.[75]
Toric intraocular lenses were introduced in 1992 and are used worldwide to correct corneal astigmatism during cataract surgery.[29][75] They have been FDA approved since 1998.[28]
According to surveys of members of the American Society of Cataract and Refractive Surgery, approximately 2.85 million cataract procedures were performed in the United States during 2004 and 2.79 million in 2005.[99] As of 2021, approximately 4 million cataract procedures take place annually in the U.S. and nearly 28 million worldwide. That is about 75,000 procedures per day globally.[100]
Regional practice and statistics
Usage in the United Kingdom
In the UK the practice of the various National Health Service healthcare providers in referring people with cataracts to surgery varied widely as of 2017, with many of the providers only referring people with moderate or severe vision loss, and often with delays.[101] This is despite guidance issued by the NHS executive in 2000 urging providers to standardize care, streamline the process, and increase the number of cataract surgeries performed in order to meet the needs of the aging population.[102] The national ophthalmology outcomes audit in 2019 found five NHS trusts with complication rates between 1.5% and 2.1%, but since the first national cataract audit in 2010, there had been a 38% reduction in posterior capsule rupture complications.[103]
India
India has raised its cataract surgical rate from just over 700 operations per million people per year in 1981, to 6,000 per million per year in 2011, which is much closer to the estimated rate of 8,000 to 8,700 per million per year needed to eliminate blindness due to cataracts in India. This is partly a combined result of increased efficiency due to improved surgical technique, with surgeons able to do twenty operations per day, application of day case surgery, improvements in operating theatre design, and efficient team work with sufficient staff.[104]
The other aspect is that people apply for surgery in large numbers. This has been achieved by creating a demand for cataract surgery in the community. Social marketing methods were used to make the population more aware of cataracts and that they are a common age-related problem that can be treated effectively at affordable cost. The NGO sector and Indian ophthalmologists have developed methods to deal with local problems, including outreach camps to find those needing surgery, counselors to explain the system, locally manufactured equipment and consumables and a tiered pricing structure, using subsidies where appropriate.[104]
There have been public scandals when multiple patients have been infected and developed endophthalmitis on the same day at some hospitals associated with eye camps in India. Journalists have reported blame being placed on the surgeons, the hospital administration, and other persons, but have not reported on who was responsible for sterilisation of the surgical instruments and theatres involved, whether all infections involved the same micro-organisms, the same theatres, or the same staff. Several instances of surgeons performing more operations per day than allowed have also been reported, but it has not been made clear how this would affect sterility of equipment, or how it might plausibly cause infection.[105]
In 2022 Scroll.in requested information on the numbers of patients who had contracted such infections from the central health ministry and received information that since 2006, 469 people have either been blinded in one eye or had their vision seriously affected after undergoing surgery at eye camps. Further inquiries indicated that the number was at least 519, but the number of surgeries was not mentioned.[105] Since the number of eye surgeries performed in India is large – as of 2017 India is claimed to be doing about 6.5 million cataract surgeries per year – more than the US, Europe and China put together – this is a very small percentage.[106]
Special populations
Congenital cataracts
Congenital cataracts are a lens opacity which is present at birth. Congenital cataracts occur in a broad range of severity: some lens opacities do not progress and are visually insignificant, others can produce profound visual impairment. Congenital cataracts may be unilateral or bilateral. They can be classified by morphology, presumed or defined genetic cause, presence of specific metabolic disorders, or associated ocular anomalies or systemic findings.[107]
In general, the younger the child, the greater the urgency in removing the cataract, because of the risk of amblyopia. For optimal visual development in newborns and young infants, a visually significant unilateral congenital cataract should be detected and removed before age six weeks, and visually significant bilateral congenital cataracts should be removed before age 10 weeks.[107]
Some congenital cataracts are too small to affect vision, therefore no surgery or treatment will be done. If they are superficial and small, an ophthalmologist will continue to monitor them throughout a patient's life. Commonly, a patient with small congenital cataracts that do not affect vision will eventually be affected later in life; generally this will take decades to occur.[108]
The standard of care as of 2015 for pediatric cataract surgery for children older than two years is primary posterior intraocular lens implantation. Primary IOL implantation before age seven months is considered to have no advantages over aphakia.[109] A 2015 study suggests that primary IOL implantation in the seven month to two years old age groups should be considered in children who require cataract surgery.[109]
Developing world
The capital equipment for phacoemulsification is expensive and requires expert maintenance, and the consumables are also expensive. Quality of outcomes is not sufficiently better than outcomes for manual small incision cataract surgery (MSICS) to justify the difference in cost in a developing world environment.[4]
Circumstances of higher risk for operations on separate occasions
Most patients suffer from bilateral cataract and although surgery of one eye can restore functional vision, second eye surgery has many advantages. Most patients undergo surgery in both eyes but on separate days. Operating on both eyes on the same day as separate procedures is known as immediately sequential bilateral cataract surgery. This can decrease the number of hospital visits which reduces risk of contagion in an epidemic There are also significant cost savings and faster visual rehabilitation and neuroadaptation. Another indication is significant cataract in both eyes where the person is not a good candidate for having anesthesia and surgery twice. The risk of bilateral simultaneous complications is low.[110][111]
See also
- Africa Cataract Project
- Eye surgery – Surgery performed on the eye or its adnexa
- Himalayan Cataract Project – U.S. nonprofit organization
- Ophthalmology – Field of medicine treating eye disorders
References
- ^ "Cataracts". www.nei.nih.gov. National Eye Institute. Retrieved 27 July 2020.
- ^ "Cataract surgery". Mayo Foundation for Medical Education and Research (MFMER). Retrieved 19 July 2021.
- ^ a b c d e f g h i j k l m n o p q r s t u v w Moshirfar, Majid; Milner, Dallin; Patel, Bhupendra C. (June 21, 2022). "Cataract Surgery". www.ncbi.nlm.nih.gov. National Center for Biotechnology Information. Retrieved 8 February 2023.
- ^ a b c d Haldipurkar, S.S.; Shikari, Hasanain T.; Gokhale, Vishwanath (2009). "Wound construction in manual small incision cataract surgery". Indian Journal of Ophthalmology. 57 (1): 9–13. doi:10.4103/0301-4738.44491. ISSN 0301-4738. PMC 2661512. PMID 19075401.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g h i j k l m n o p q r s t u v Cionni, Robert J.; Snyder, Michael E.; Osher, Robert H. (2006). "6: Cataract surgery". In Tasman, William (ed.). Duane's Opthalmology. Vol. 6. Lippincott, Williams and Wilkins. Retrieved 16 February 2023 – via www.oculist.net.
- ^ a b c d e f g h i j k l "Facts About Cataract". September 2009. Archived from the original on 24 May 2015. Retrieved 24 May 2015.
- ^ a b Pandey SK (2005). Pediatric cataract surgery techniques, complications, and management. Philadelphia: Lippincott Williams & Wilkins. p. 20. ISBN 978-0781743075. Archived from the original on 2015-05-24.
- ^ Allen D, Vasavada A (July 2006). "Cataract and surgery for cataract". BMJ. 333 (7559): 128–132. doi:10.1136/bmj.333.7559.128. PMC 1502210. PMID 16840470.
- ^ Gimbel HV, Dardzhikova AA (January 2011). "Consequences of waiting for cataract surgery". Current Opinion in Ophthalmology. 22 (1): 28–30. doi:10.1097/icu.0b013e328341425d. PMID 21076306. S2CID 205670956.
- ^ "Visual impairment and blindness Fact Sheet N°282". August 2014. Archived from the original on 12 May 2015. Retrieved 23 May 2015.
- ^ Global Data on Visual Impairments 2010 (PDF). WHO. 2012. p. 6. Archived (PDF) from the original on 2015-03-31.
- ^ a b c "Priority eye diseases". Archived from the original on 24 May 2015. Retrieved 24 May 2015.
- ^ "Recognizing Cataracts". NIH News in Health. 2017-05-30. Retrieved 2020-02-02.
Try wearing sunglasses or a hat with a brim. Researchers also believe that good nutrition can help reduce the risk of age-related cataract. They recommend eating plenty of green leafy vegetables, fruits, nuts and other healthy foods.
- ^ Lamoureux EL, Fenwick E, Pesudovs K, Tan D (January 2011). "The impact of cataract surgery on quality of life". Current Opinion in Ophthalmology. 22 (1): 19–27. doi:10.1097/icu.0b013e3283414284. PMID 21088580. S2CID 22760161.
- ^ a b Rao GN, Khanna R, Payal A (January 2011). "The global burden of cataract". Current Opinion in Ophthalmology. 22 (1): 4–9. doi:10.1097/icu.0b013e3283414fc8. PMID 21107260. S2CID 205670997.
- ^ a b "Cataract Data and Statistics | National Eye Institute". www.nei.nih.gov. Retrieved 2019-11-18.
- ^ Lawrence, D.; Fedorowicz, Z.; van Zuuren, E.J.; et al. (Cochrane Eyes and Vision Group) (November 2015). "Day care versus in-patient surgery for age-related cataract". The Cochrane Database of Systematic Reviews. 2015 (11): CD004242. doi:10.1002/14651858.CD004242.pub5. PMC 7197209. PMID 26524611.
- ^ a b Toczolowski, J. (July 1993). "Thirty years of cryoophthalmology". Ann Ophthalmol. 25 (7): 254–6. PMID 8363292.
- ^ Alió, J.L.; Abdou, A.A.; Puente, A.A.; Zato, M.A.; Nagy, Z. (June 2014). "Femtosecond laser cataract surgery: updates on technologies and outcomes". Journal of Refractive Surgery. 30 (6): 420–427. doi:10.3928/1081597x-20140516-01. PMID 24972409.
- ^ Popovic, M.; Campos-Möller, X; Schlenker, M.B.; Ahmed, I.I. (October 2016). "Efficacy and Safety of Femtosecond Laser-Assisted Cataract Surgery Compared with Manual Cataract Surgery: A Meta-Analysis of 14 567 Eyes". Ophthalmology. 123 (10): 2113–2126. doi:10.1016/j.ophtha.2016.07.005. PMID 27538796.
- ^ Barsam, Allon; Allan, Bruce (17 July 2014). "Excimer laser refractive surgery versus phakic intraocular lenses for the correction of moderate to high myopia". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.cd007679.pub4. ISSN 1465-1858. PMID 24937100.
- ^ a b Scholtz, Sibylle (January 2007). "History of Ophthalmic Viscosurgical Devices". crstodayeurope.com. Cataract & Refractive Surgery Today Europe. Retrieved 13 February 2023.
- ^ a b c Sridhar, U; Tripathy, K. (22 August 2022). "Monofocal Intraocular Lenses". StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing.
- ^ a b Grayson, Douglas (4 October 2011). "The Ins and Outs of Lens Explantation". Review of Ophthalmology. Retrieved 14 February 2023.
- ^ Salerno, Liberdade C.; Tiveron, Jr., Mauro C.; Alió, Jorge L. (2017). "Multifocal intraocular lenses: Types, outcomes, complications and how to solve them". Taiwan Journal of Ophthalmology. 7 (4): 179–184. doi:10.4103/tjo.tjo_19_17. PMC 5747227. PMID 29296549.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "New Device Approval – CrystaLens Model AT-45 Accommodating IOL – P030002". www.fda.gov. U.S. Food and Drug Administration.[dead link]
- ^ MacRae, Scott. "Crystalens: The First Accommodating Intraocular Lens Implant". www.urmc.rochester.edu. University of Rochester Flaum Eye Institute. Retrieved 14 February 2023.
- ^ a b Ramappa, Muralidhar; Singh, Vivek Mahendrapratap; Murthy, SomasheilaI; Rostov, AudreyTalley (2022). "Toric intraocular lenses: Expanding indications and preoperative and surgical considerations to improve outcomes". Indian Journal of Ophthalmology. 70 (1): 10–23. doi:10.4103/ijo.IJO_1785_21. ISSN 0301-4738. PMC 8917572. PMID 34937203.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c Singh, Vivek Mahendrapratap; Ramappa, Muralidhar; Murthy, Somasheila; Rostov, Audrey Talley (January 2022). "Toric intraocular lenses: Expanding indications and preoperative and surgical considerations to improve outcomes". Indian J Ophthalmol. 70 (1): 10–23. doi:10.4103/ijo.IJO_1785_21. PMC 8917572. PMID 34937203.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Yetman, Daniel (13 January 2023). Lloyd III, William C. (ed.). "Do You Need Glasses After Cataract Surgery?". Retrieved 18 February 2023.
- ^ Roach, Linda. "How to Choose an Aspheric Intraocular Lens". EyeNet Magazine. American Academy of Ophthalmology. Retrieved 17 February 2023.
- ^ Downie, L.E.; Busija, L.; Keller, P.R.; et al. (Cochrane Eyes and Vision Group) (May 2018). "Blue-light filtering intraocular lenses (IOLs) for protecting macular health". The Cochrane Database of Systematic Reviews. 2018 (5): CD011977. doi:10.1002/14651858.CD011977.pub2. PMC 6494477. PMID 29786830.
- ^ a b Hayashi, K.; Hayashi, H. (2006). "Visual function in patients with yellow tinted intraocular lenses compared with vision in patients with non-tinted intraocular lenses". British Journal of Ophthalmology. 90 (8): 1019–1023. doi:10.1136/bjo.2006.090712. PMC 1857188. PMID 16597662.
- ^ "FDA Approves RxSight's Light Adjustable Lens, First IOL To Enable Refractive Correction After Cataract Surgery". innovation.ucsf.edu. University of California San Francisco. 27 November 2017. Retrieved 21 February 2023.
- ^ Jain, Sneha; Patel, Alpa S.; Tripathy, Koushik; DelMonte, Derek W.; Baartman, Brandon (3 October 2022). DelMonte, Derek W. (ed.). "Light Adjustable Intraocular lenses". EyeWiki. American Academy of Opthalmology.
- ^ Portelinha, Joana; Ferreira, Tiago Luís do Carmo Bravo; Reddy, Vandana; Shafer, Brian (8 January 2023). Shafer, Brian (ed.). "Special Cases: Secondary Piggy-Back Lenses". Eyewiki. American Academy of Ophthalmology.
- ^ Hasan, Sumaiya; Tripathy, K. (22 August 2022). "Phakic Intraocular Lens Myopia". StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing.
- ^ a b c d e f Goldsberry, Dennis H. (May 2012). "Achieving Better Outcomes Using Free Online Post-LASIK IOL Calculators". crstodayeurope.com. CRSTEurope. Retrieved 11 February 2023.
- ^ Straub, Laura. "SRK/T Formula: A Review: A combination of linear regression method with a theoretical eye model". crstodayeurope.com. CRSTEurope. Retrieved 11 February 2023.
- ^ Vicchrilli, Sue; Glasser, David B.; McNett, Cherie; Burke, Mara Pearse; Repka, Michael X. (October 2018). "Premium IOLs—A Legal and Ethical Guide to Billing Medicare Beneficiaries". EyeNet Magazine. Retrieved 21 February 2023.
- ^ Liaska, A; Papaconstantinou, D; Georgalis, I; Koutsandrea, C; Theodosiadis, P; Chatzistefanou, K. (July 2014). "Phaco-trabeculectomy in controlled, advanced, open-angle glaucoma and cataract: Parallel, randomized clinical study of efficacy and safety". Semin Ophthalmol. 29 (4): 226–35. doi:10.3109/08820538.2014.880491. S2CID 19497442.
- ^ Akman, A; Yilmaz, G; Oto, S; Akova, YA (September 2004). "Comparison of various pupil dilatation methods for phacoemulsification in eyes with a small pupil secondary to pseudoexfoliation". Ophthalmology. 111 (9): 1693–8. doi:10.1016/j.ophtha.2004.02.008.
- ^ Rishi, P.; Sharma, T.; Rishi, E.; Chaudhary, S.P. (January–April 2009). "Combined scleral buckling and phacoemulsification". Oman J Ophthalmol. 2 (1): 15–8. doi:10.4103/0974-620X.48416. PMC 3018099. PMID 21234218.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Charters, Linda (15 June 2006). "Anticipation is key to managing intra-operative floppy iris syndrome". Ophthalmology Times. Archived 22 October 2006 at the Wayback Machine
- ^ Keay, L.; Lindsley, K.; Tielsch, J.; Katz, J.; Schein, O. (January 2019). "Routine preoperative medical testing for cataract surgery". The Cochrane Database of Systematic Reviews. 1 (1): CD007293. doi:10.1002/14651858.CD007293.pub4. PMC 6353242. PMID 30616299.
- ^ "Cataract surgery". Mayo Foundation for Medical Education and Research (MFMER). Retrieved 19 July 2021.
- ^ a b c d Minakaran, N.; Ezra, D.G.; Allan, B.D. (July 2020). "Topical anaesthesia plus intracameral lidocaine versus topical anaesthesia alone for phacoemulsification cataract surgery in adults". The Cochrane Database of Systematic Reviews. 2020 (7): CD005276. doi:10.1002/14651858.cd005276.pub4. PMC 8190979. PMID 35658539.
- ^ a b c d Gurnani, Bharat; Kaur, Kirandeep (6 December 2022). "Phacoemulsification". StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing.
- ^ Mohammadpour, M.; Erfanian, R.; Karimi, N. (January 2012). "Capsulorhexis: Pearls and pitfalls". Saudi J Ophthalmol. 26 (1): 33–40. doi:10.1016/j.sjopt.2011.10.007. PMC 3729482. PMID 23960966.
- ^ Yanoff, Myron; Duker, Jay S. (1 January 2009). Ophthalmology. Elsevier Health Sciences. ISBN 978-0323043328 – via Google Books.
- ^ Faust, KJ. (Winter 1984). "Hydrodissection of soft nuclei". J Am Intraocul Implant Soc. 10 (1): 75–7. doi:10.1016/s0146-2776(84)80088-9. PMID 6706823.
- ^ Patel, Alpa S.; DelMonte, Derek W.; Mohan, Hridya; Christenbury, Joseph (24 September 2022). Christenbury, Joseph (ed.). "Hydro Manoeuvres in Cataract Surgery". Eyewiki. American Academy of Ophthalmology.
- ^ Mathey, Christoph F.; Kohnen, Thomas B.; Ensikat, Hans-Jürgen; Koch, Hans-Reinhard (January 1994). "Polishing methods for the lens capsule: Histology and scanning electron microscopy". Journal of Cataract & Refractive Surgery. 20 (1): 64–69. doi:10.1016/S0886-3350(13)80046-6. S2CID 11738948.
- ^ Oetting, Thomas. "Capsulorhexis using a cystotome needle during cataract surgery". Archived 26 August 2008 at the Wayback Machine
- ^ Sharma, Bhavana; Abell, Robin G; Arora, Tarun; Antony, Tom; Vajpayee, Rasik B (2019). "Techniques of anterior capsulotomy in cataract surgery". Indian Journal of Ophthalmology. 67 (4): 450–460. doi:10.4103/ijo.IJO_1728_18. PMC 6446625. PMID 30900573.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Salmon, John F. (2020). Kanski's Clinical Ophthalmology: A Systematic Approach (9th ed.). Edinburgh. p. 331. ISBN 978-0-7020-7713-5. OCLC 1131846767.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Wier, L.M.; Steiner, C.A.; Owens, P.L. (February 2015). "Surgeries in Hospital-Owned Outpatient Facilities, 2012". HCUP Statistical Brief #188. Rockville, MD: Agency for Healthcare Research and Quality.
- ^ a b Ou, Yvonne (5 July 2021). "Side Effects of Laser Iridotomy". www.brightfocus.org. University of California, San Francisco. Retrieved 23 February 2023.
- ^ Miguel, Ana IM; Marques, Sara HM; Cruz, Mário; Aref, Ahmad A.; Silva,, André Borges; Tsui, Jonathan C. (25 December 2022). Aref, Ahmad A. (ed.). "Laser Peripheral Iridotomy". Eyewiki. American Academy of Opthalmology. Retrieved 23 February 2023.
{{cite web}}: CS1 maint: extra punctuation (link) - ^ a b Wang, Robert C.; Fuller, Dwain G.; Hutton, William S. (2006). "66: Retained Lens Material". In Tasman, William (ed.). Duane's Opthalmology. Vol. 6. Lippincott, Williams and Wilkins. Retrieved 16 February 2023 – via www.oculist.net.
- ^ Vajpayee, R.B.; Sharma, N.; Dada, T.; Gupta, V.; Kumar, A.; Dada, V.K. (1 June 2001). "Management of posterior capsule tears". Surv Ophthalmo L. 45 (6): 473–88. doi:10.1016/s0039-6257(01)00195-3. PMID 11425354.
- ^ Chaturvedi, Vivek; Sabherwal, Ryan; Kim, Leo A.; Pittner, Andrew; Bhagat, Neelakshi; Lim, Jennifer I; Mukkamala, Lekha; Patel, Nimesh (23 June 2022). Patel, Nimesh (ed.). "Suprachoroidal Hemorrhage". Eyewiki. American Academy of Opthalmology.
- ^ "Videos: YAG Laser Capsulotomy". Pacific Cataract and Laser Institute. Retrieved 2 April 2019.
- ^ Karahan, Eyyup; Er, Duygu; Kaynak, Suleyman (Summer 2014). "An Overview of Nd:YAG Laser Capsulotomy". Medical Hypothesis, Discovery & Innovation Ophthalmology Journal. 3 (2): 45–50. PMC 4346677. PMID 25738159.
- ^ a b Steel, D. (March 2014). "Retinal detachment". BMJ Clinical Evidence. 2014. PMC 3940167. PMID 24807890.
- ^ Feltgen, N.; Walter, P. (January 2014). "Rhegmatogenous retinal detachment--an ophthalmologic emergency". Deutsches Ärzteblatt International. 111 (1–2): 12–21, quiz 22. doi:10.3238/arztebl.2014.0012. PMC 3948016. PMID 24565273.
- ^ "Toxic Anterior Segment Syndrome After Cataract Surgery". Centers for Disease Control and Prevention. 29 June 2007. Retrieved 18 April 2013.
- ^ "Endophthalmitis". The Lecturio Medical Concept Library. Retrieved 19 July 2021.
- ^ Lim, B.X.; Lim, C.H.; Lim, D.K.; Evans, J.R.; Bunce, C.; Wormald, R. (November 2016). "Prophylactic non-steroidal anti-inflammatory drugs for the prevention of macular oedema after cataract surgery". The Cochrane Database of Systematic Reviews. 11 (11): CD006683. doi:10.1002/14651858.CD006683.pub3. PMC 6464900. PMID 27801522.
- ^ Zemba, M.; Camburu, G (2017). "Uveitis-Glaucoma-Hyphaema Syndrome. General review". Romanian Journal of Ophthalmology. 61 (1): 11–17. doi:10.22336/rjo.2017.3. PMC 5710046. PMID 29450365.
- ^ a b c Stein, Joshua D.; Grossman, Daniel S.; Mundy, Kevin M.; Sugar, Alan; Sloan, Frank A. (2 June 2011). "Severe Adverse Events after Cataract Surgery Among Medicare Beneficiaries". Ophthalmology. 118 (9): 1716–1723. doi:10.1016/j.ophtha.2011.02.024.
- ^ a b "Recovery - Cataract surgery". www.nhs.uk. 15 January 2018. Retrieved 12 February 2023.
- ^ a b "How Many Days Rest Are Needed After Cataract Surgery?". southcaleye.com. 18 May 2022. Retrieved 22 February 2023.
- ^ Dudek, Lara (15 September 2020). "After Cataract Surgery: Dos and Don'ts". Retrieved 22 February 2023.
- ^ a b c d e f g Davis, G. (January–February 2016). "The Evolution of Cataract Surgery". Mo Med. 113 (1). Missouri State Medical Association: 58–62. PMC 6139750. PMID 27039493.
- ^ "Chapter 5: Microsurgery and Extracapsular Cataract Extraction" (PDF). rajswasthya.nic.in. pp. 36–44. Retrieved 12 February 2023.
- ^ Isawumi, M.A.; Kolawole, O.U.; Hassan, M.B. (June 2013). "Couching techniques for cataract treatment in Osogbo, South west Nigeria". Ghana Medical Journal. 47 (2): 64–9. PMC 3743109. PMID 23966741.
- ^ a b c Ascaso FJ, Lizana J, Cristóbal JA (March 2009). "Cataract surgery in ancient Egypt". Journal of Cataract and Refractive Surgery. 35 (3): 607–608. doi:10.1016/j.jcrs.2008.11.052. PMID 19251160.
- ^ "Hoax: Picture from Ancient Egypt Nothing to Do with COVID-19 Test". TASR. 25 January 2021.
- ^ Meulenbeld, G.J. (1999–2002). A History of Indian Medical Literature. Groningen: Forsten.
- ^ Sharma, P.V. (2001). Suśruta-Saṃhitā with English translation of text and Ḍalhaṇa's commentary along with critical notes. Vol ĪI (Kalpasthāna and Uttaratantra). Varanasi, India: Chaukhambha Visvabharati Oriental. pp. 202–204.
- ^ Deshpande, V. (2000). "Ophthalmic surgery: a chapter in the history of Sino-Indian medical contacts". Bulletin of the School of Oriental and African Studies. 63 (3): 370–388. doi:10.1017/S0041977X00008454. S2CID 162655091. See also Deshpande, V. (1999). "Indian influences on early Chinese ophthalmology: glaucoma as a case study". Bulletin of the School of Oriental and African Studies. 62 (22): 306–322. doi:10.1017/S0041977X00016724. S2CID 162306288.
- ^ Urabe, H. (September 1976). "[Classification of ringworm infections (author's transl)]". Nihon Hifuka Gakkai Zasshi. The Japanese Journal of Dermatology. 86 (10): 573–581. PMID 1034789.
- ^ Magner LN (1992). A History of Medicine. CRC Press. p. 91.
- ^ Leffler CT, Hadi TM, Udupa A, Schwartz SG, Schwartz D (2016). "A medieval fallacy: the crystalline lens in the center of the eye". Clinical Ophthalmology. 10 (10): 649–662. doi:10.2147/OPTH.S100708. PMC 4833360. PMID 27114699.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ McKissack, P; McKissack, F. (1995). The Royal Kingdoms of Ghana, Mali, and Songhay Life in Medieval Africa. Macmillan. p. 104. ISBN 978-0-8050-4259-7.
- ^ Thompson, E.E. (January 1965). "Primitive African Medical Lore and Witchcraft". Bulletin of the Medical Library Association. 53 (1): 80–94. PMC 198231. PMID 14223742.
- ^ a b "'Couching' for cataracts remains a persistent problem in Yemen" (PDF). EuroTimes. September 2005. p. 11. Archived 26 July 2011 at the Wayback Machine
- ^ "Toric Lens Implants | Pacific Cataract and Laser Institute: For Doctors of Optometry". odpcli.com. Retrieved 2019-10-09.
- ^ Bergman WC, Schulz RA, Davis DS (September 2009). "Factors influencing the genesis of neurosurgical technology". Neurosurgical Focus. 27 (3): E3. doi:10.3171/2009.6.FOCUS09117. PMID 19722817.
- ^ a b c d Savage-Smith, E. (August 2000). "The practice of surgery in Islamic lands: myth and reality". Social History of Medicine. 13 (2): 307–321. doi:10.1093/shm/13.2.307. PMID 14535259.
- ^ Finger S (1994). Origins of Neuroscience: A History of Explorations Into Brain Function. Oxford University Press. p. 70. ISBN 978-0-19-514694-3.
- ^ Leffler CT, Wainsztein RD (2016). "The first cataract surgeons in Latin America: 1611-1830". Clinical Ophthalmology. 10: 679–694. doi:10.2147/OPTH.S105825. PMC 4841434. PMID 27143845.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Leffler CT, Schwartz SG, Grzybowski A, Braich PS (2015). "The first cataract surgeons in Anglo-America". Survey of Ophthalmology. 60 (1): 86–92. doi:10.1016/j.survophthal.2014.08.002. PMC 4262555. PMID 25444521.
- ^ Leffler CT, Letocha CE, Pierson K, Schwartz SG (2017). "Aspiration of cataract in 1815 in Philadelphia, Pennsylvania". Digital Journal of Ophthalmology. 23 (4): 4–7. doi:10.5693/djo.01.2017.10.001. PMC 5791631. PMID 29403333.
- ^ Badrinath, S.S.; Biswas, J.; Badrinath, Vasanthi (2004-10-10). "Prince of Ophthalmology". The Hindu. Archived from the original on 2005-01-18.
- ^ Meadow, Norman B. (15 October 2005). "Cryotherapy: A fall from grace, but not a crash". Ophthalmology Times.
- ^ Pandey, Suresh K.; Milverton, E. John; Maloof, Anthony J. (October 2004). "A tribute to Charles David Kelman MD: ophthalmologist, inventor and pioneer of phacoemulsification surgery". Clinical & Experimental Ophthalmology. 32 (5): 529–533. doi:10.1111/j.1442-9071.2004.00887.x. ISSN 1442-6404. PMID 15498067. S2CID 25230092.
- ^ "American Academy of Ophthalmology News". www.aao.org. 5 April 2006. [permanent dead link]
- ^ Lindstrom, Richard L. (10 February 2021). "Future of cataract surgery seems promising". occular surgery news. Healio.
- ^ "Two thirds of eye units restricting access to cataract surgery". OnMedica. 10 November 2017. Retrieved 28 December 2017.
- ^ "Action on Cataracts Good Practice Guidance" (PDF). NHS Executive via the Royal College of Ophthalmologists. January 2000., referenced in "Context: Guideline for Cataracts in adults". NICE. October 2017.
- ^ "Revealed: The trusts with the highest cataract complication rates". Health Service Journal. 11 October 2019. Retrieved 21 November 2019.
- ^ a b Vs Murthy, G.; Jain, B.; Shamanna, B; Subramanyam, D. (2014). "Improving cataract services in the Indian context". Community Eye Health. 27 (85): 4–5. PMC 4069775. PMID 24966453.
- ^ a b Barnagarwala, Tabassum (23 February 2022). "When India's mass eye camps leave people blind". Scroll.in. Retrieved 23 February 2023.
- ^ Mabiyan, Rashmi (25 October 2017). "Cataract prevalent in India despite largest number of surgeries: Dr Mahipal S Sachdev, Centre for Sight".
- ^ a b Basic and clinical science course (2011–2012). Pediatric ophthalmology and Strabismus. American Academy of Ophthalmology. ISBN 978-1615251131.
- ^ "Facts About Cataract | National Eye Institute". nei.nih.gov. Retrieved 2017-10-18.
- ^ a b Struck, M.C. (October 2015). "Long-term Results of Pediatric Cataract Surgery and Primary Intraocular Lens Implantation From 7 to 22 Months of Life". JAMA Ophthalmol. 133 (10): 1180–1183. doi:10.1001/jamaophthalmol.2015.2062.
- ^ Alió, Jorge L.; Nowrouzi, Ali (29 August 2022). "Immediately sequential bilateral cataract surgery importance during the COVID-19 pandemic". Saudi J Ophthalmol. 36 (2): 124–128. doi:10.4103/sjopt.sjopt_131_22 (inactive 2023-02-22). PMC 9535909. PMID 36211314.
{{cite journal}}: CS1 maint: DOI inactive as of February 2023 (link) CS1 maint: unflagged free DOI (link) - ^ Obuchowska, I; Mariak, Z. (2006). "Jednoczesna operacja zaćmy w obojgu oczach--zalety i wady [Simultaneous bilateral cataract surgery--advantages and disadvantages]". Klin Oczna (in Polish). 108 (7–9): 353–6. PMID 17290841.
Further reading
- Frampton G, Harris P, Cooper K, Lotery A, Shepherd J (November 2014). "The clinical effectiveness and cost-effectiveness of second-eye cataract surgery: a systematic review and economic evaluation". Health Technology Assessment. 18 (68). NIHR Journals Library: 1–205, v–vi. doi:10.3310/hta18680. PMC 4781176. PMID 25405576. 18.68.
- Prajna NV, Ravilla TD, Srinivasan S (2015). "Ch: 11. Cataract Surgery". In Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, Mock CN (eds.). Essential Surgery. Disease Control Priorities. Vol. 1 (3rd ed.). The International Bank for Reconstruction and Development / The World Bank. ISBN 978-1-4648-0346-8. PMID 26740991.
- Tasman, William, ed. (2006). "Duane's Opthalmology". Lippincott, Williams and Wilkins – via www.oculist.net.
