Heart transplantation: Difference between revisions
m moved Heart transplant to Heart transplantation: Moving revisions as part of history merge |
m Rollback to complete history merge |
||
| Line 1: | Line 1: | ||
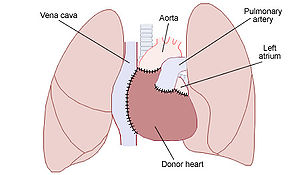
[[Image:Heart transplant.jpg|thumb|325px|(Diagram illustrating the placement of a donor [[heart]] in an '''orthotopic procedure'''. Notice how the back of the patient's [[left atrium]] and [[great vessels]] are left in place).]] |
|||
A '''heart transplant''' , is a surgical [[organ transplant|transplant]] procedure performed on patients with [[heart failure]] or severe [[coronary artery disease]]. The most common procedure is to take a working [[heart]] from a recently deceased [[organ donor]] ([[allograft]]) and implant it into the patient (usually after removing the patients original heart, although this is not always the case). It is also possible to take a heart from another species ([[xenograft]]), or implant a man-made [[artificial heart|artificial one]], although these two procedures have been less successful in comparison to the far more commonly performed [[allograft|allografts]]. |
|||
'''Hearts transplants''', or '''cardiac transplantation''', is a surgical [[organ transplant|transplant]] procedure performed on patients with end-stage [[heart failure]] or severe [[coronary artery disease]]. The most common procedure is to take a working [[heart]] from a recently deceased [[organ donor]] (cadaveric [[allograft]]) and implant it into the patient. The patient's own heart may either be removed ([[heart transplantation#Orthotopic procedure|orthotopic procedure]]) or, less commonly, left in to support the donor heart ([[heart transplantation#Heterotopic procedure|heterotopic procedure]]); both are controversial solutions to one of the most enduring human ailments. Post-operation survival periods now average 15 years.<ref name="2007 documentary">{{cite video |
|||
| people = Till Lehmann (director) |
|||
| title = The Heart-Makers: The Future of Transplant Medicine |
|||
| medium = documentary film |
|||
| publisher = LOOKS film and television |
|||
| location = Germany |
|||
|date = 2007}}</ref> |
|||
The world's first human heart transplant was performed by [[Christiaan Barnard]] on December 3, 1967 in [[Cape Town]] [[South Africa]] on a man called [[Louis Washkansky]].<ref name="Daily_I">{{cite news|date=November 29, 1987 |title=Memories of the Heart |publisher=''Daily Intelligencer'' |location=Doylestown, Pennsylvania |page=A-18}}</ref> The first successful human heart transplant in the United States was performed at [[Maimonides Medical Center]].<ref>{{cite news| url=http://www.nytimes.com/2008/11/19/us/19kantrowiztz.html | work=The New York Times | first=Jascha | last=Hoffman | title=Dr. Adrian Kantrowitz, Cardiac Pioneer, Dies at 90 | date=2008-11-19}}</ref> Worldwide there are 3,500 heart transplants performed every year; about 800,000 people have a Class IV heart defect and need a new organ.<ref>{{cite video |
|||
==History== |
|||
| people = Reiner Körfer (interviewee) |
|||
The first heart transplant was performed by Professor [[Christiaan Barnard]] at [[Groote Schuur Hospital]] in December [[1967]]. The patient was a [[Louis Washkansky]] of [[Cape Town]], [[South Africa]], who lived for 18 days after the procedure before dying of [[pneumonia]].The donor was [[Denise Darvall]], who had recently been critically injured in a car accident. |
|||
| title = The Heart-Makers: The Future of Transplant Medicine |
|||
| medium = documentary film |
|||
| publisher = LOOKS film and television |
|||
| location = Germany |
|||
|date = 2007}}</ref> This disparity has spurred considerable research into the use of non-human hearts since 1993. It is now possible to take a heart from another species ([[xenograft]]), or implant a man-made [[artificial heart|artificial one]], although the outcome of these two procedures has been less successful in comparison to the far more commonly performed [[allograft]]s. Engineers want to fix the remaining problems with the manufactured options in the next 15 years.<ref name="2007 documentary"/> |
|||
==Contraindications== |
|||
==Reference== |
|||
Some patients are less suitable for a heart transplant, especially if they suffer from other [[circulatory]] conditions unrelated to the heart. The following conditions in a patient would increase the chances of [[complication (medicine)|complications]] occurring during the operation: |
|||
http://www.capegateway.gov.za/eng/pubs/public_info/C/99478 |
|||
*[[Kidney]], [[lung]], or [[liver]] disease |
|||
*Insulin-dependent [[diabetes]] with other organ dysfunction |
|||
*Life-threatening diseases unrelated to [[heart failure]] |
|||
*[[Vascular disease]] of the neck and leg arteries. |
|||
*High pulmonary vascular resistance |
|||
*Recent [[thromboembolism]] |
|||
*Age over 60 years (some variation between centres) |
|||
*Alcohol, tobacco or drug abuse |
|||
==Procedures== |
|||
{{surgery-stub}} |
|||
===Pre-operative=== |
|||
A typical heart transplantation begins with a suitable donor heart being located from a recently [[deceased]] or [[Brain death|brain dead]] donor, also called a [[beating heart cadaver]]. The transplant patient is contacted by a [[nurse]] coordinator and instructed to attend the hospital in order to be evaluated for the operation and given pre-surgical medication. At the same time, the heart is removed from the donor and inspected by a team of surgeons to see if it is in a suitable condition to be transplanted. Occasionally it will be deemed unsuitable. This can often be a very distressing experience for an already emotionally unstable patient, and they will usually require emotional support before being sent home. |
|||
The patient must also undergo many emotional, psychological, and physical tests to make sure that they are in good mental health and will make good use of their new heart. The patient is also given [[immunosuppressant]] medication so that their immune system will not reject the new heart. |
|||
===Operative=== |
|||
[[Image:Heart transplant.jpg|thumb|right|300px|Schematic of a transplanted heart with native [[lung]]s and the [[great vessels]].]] |
|||
Once the donor heart has passed its inspection, the patient is taken into the [[operating room]] and given a [[general anesthetic]]. Either an '''orthotopic''' or a '''heterotopic''' procedure is followed, depending on the condition of the patient and the donor heart. |
|||
====Orthotopic procedure==== |
|||
The '''orthotopic procedure''' begins with the surgeons performing a [[median sternotomy]] to expose the [[mediastinum]]. The [[pericardium]] is opened, the [[great vessels]] are [[dissect]]ed and the patient is attached to [[cardiopulmonary bypass]]. The failing heart is removed by transecting the great vessels and a portion of the [[left atrium]]. The [[pulmonary vein]]s are not transected; rather a circular portion of the left atrium containing the pulmonary veins is left in place. The donor heart is trimmed to fit onto the patient's remaining left atrium and the great vessels are [[surgical suture|suture]]d in place. The new heart is restarted, the patient is weaned from cardiopulmonary bypass and the chest cavity is closed. |
|||
====Heterotopic procedure==== |
|||
In the '''heterotopic procedure''', the patient's own heart is not removed before implanting the donor heart. The new heart is positioned so that the chambers and blood vessels of both hearts can be connected to form what is effectively a 'double heart'. The procedure can give the patients original heart a chance to recover, and if the donor's heart happens to fail (e.g. through [[transplant rejection|rejection]]), it may be removed, allowing the patient's original heart to start working again. Heterotopic procedures are only used in cases where the donor heart is not strong enough to function by itself (due to either the patient's body being considerably larger than the donor's, the donor having a weak heart, or the patient suffering from [[pulmonary hypertension]]). |
|||
===Post-operative=== |
|||
The patient is taken into [[Intensive care unit|ICU]] to recover. When they wake up, they will be transferred to a special recovery unit in order to be [[Physical medicine and rehabilitation|rehabilitated]]. How long they remain in hospital post-transplant depends on the patient's general health, how well the new heart is working, and their ability to look after their new heart. Doctors typically like the new recipients to leave hospitals soon after surgery because of the risk of infection in a hospital (typically 1 – 2 weeks without any complications). Once the patient is released, they will have to return to the hospital for regular check-ups and rehabilitation sessions. They may also require emotional support. The number of visits to the hospital will decrease over time, as the patient adjusts to their transplant. The patient will have to remain on [[immunosuppressant]] medication to avoid the possibility of [[transplant rejection|rejection]]. Since the [[vagus nerve]] is severed during the operation, the new heart will beat at around 100 [[bpm]] unless [[nerve regrowth]] occurs. |
|||
The patient will be monitored to detect rejection of the heart by the body. This surveillance can be performed via frequent biopsy or a genetic expression blood test known as [[AlloMap Molecular Expression Testing]]. Typically, biopsy is performed immediately post transplant and then AlloMap blood testing is performed once the patient is stable. The transition from biopsy to AlloMap could occur as soon as 55 days post transplant. |
|||
=='Living organ' transplant== |
|||
Doctors made medical history in February 2006, at [[Bad Oeynhausen]] Clinic for Thorax- and Cardiovascular Surgery, [[Germany]], when they successfully transplanted a 'beating heart' into a patient.<ref>{{cite news | author= | title=Bad Oeynhausen Clinic for Thorax- and Cardiovascular Surgery Announces First Successful Beating Human Heart Transplant | url=http://www.transmedics.com/wt/page/pr_1140714229 | date=23 February 2006 | publisher=TransMedics | accessdate = 2007-05-14}}</ref> |
|||
Normally a donor's heart is injected with [[potassium chloride]] in order to stop it beating, before being removed from the donor's body and packed in ice in order to preserve it. The ice can usually keep the heart fresh for a maximum of four<ref>[http://www.drugs.com/pdr/custodiol-htk-solution.html Custodiol Htk Solution patient advice including side effects<!-- Bot generated title -->]</ref> to six hours with proper preservation, depending on its starting condition. Rather than cooling the heart, this new procedure involves keeping it at [[body temperature]] and hooking it up to a special machine called an [[Organ care system|Organ Care System]] that allows it to continue beating with warm, oxygenated blood flowing through it. This can maintain the heart in a suitable condition for much longer than the traditional method. |
|||
==Complications== |
|||
Post-operative complications include infection, sepsis, organ rejection, as well as the side-effects of the immunosupressive medication. Since the transplanted heart originates from another organism, the recipient's immune system may attempt to reject it. [[Immunosupressive drug]]s reduce that risk, but may have some unwanted side effects, such as increased likelihood of infections or nephrotoxic effects. |
|||
==Prognosis== |
|||
The prognosis for heart transplant patients following the orthotopic procedure has greatly increased over the past 20 years, and as of June 5, 2009, the survival rates were as follows.<ref>[http://www.americanheart.org/presenter.jhtml?identifier=4588 Heart Transplants: Statistics] ''The [[American Heart Association]]''. Retrieved 28 February 2009.</ref> |
|||
* 1 year: 88% (males), 77.2% (females) |
|||
* 3 years: 79.3% (males), 77.2% (females) |
|||
* 5 years: 73.1% (males), 67.4% (females) |
|||
In a November 2008 study conducted on behalf of the U.S. federal government by Dr. Eric Weiss of the [[Johns Hopkins University School of Medicine]], it was discovered that heart transplants — all other factors being accounted for — work better in same-sex transplants (male to male, female to female). However, due to the present acute shortage in donor hearts, this may not always be feasible. |
|||
As of August 2009, [[Tony Huesman]] was the world's longest living heart transplant recipient, having survived for 31 years with a transplanted heart. Huesman received a heart in 1978 at the age of 20 after [[viral pneumonia]] severely weakened his heart. Huesman died on August 10, 2009 of cancer.<ref>http://www.columbusdispatch.com/live/content/local_news/stories/2009/08/10/aheart.html?sid=101</ref> The operation was performed at [[Stanford University]] under American heart transplant pioneer [[Norman Shumway|Dr. Norman Shumway]].<ref>[http://www.cbsnews.com/stories/2006/09/14/ap/health/mainD8K49NG86.shtml Heart Transplant Patient OK After 28 Yrs] (14 September 2006) ''CBS News''. Retrieved 29 December 2006.</ref> Another noted heart transplant recipient, [[Kelly Perkins]], climbs mountains around the world to promote positive awareness of organ donation. Perkins is the first heart transplant recipient to climb to the peaks of [[Mount Fuji|Mt. Fuji]], [[Mount Kilimanjaro|Mt. Kilimanjaro]], the [[Matterhorn]], [[Mount Whitney|Mt. Whitney]], and Cajon de Arenales in Argentina in 2007, 12 years after her transplant surgery. Dwight Kroening is yet another noted recipient promoting positive awareness for organ donation. Twenty two years after his heart transplant, he is the first to finish an [[Ironman competition]].<ref>[http://www.youtube.com/watch?v=5RuijhlU8aU Dwight Kroening first heart transplant to do ironman] Retrieved 27 August 2008.</ref> |
|||
Fiona Coote was the second Australian to receive a heart transplant in 1984 (at age 14) and the youngest Australian. At 24 years since her transplant she is also a long term survivor and is involved in publicity and charity work for the [[Red Cross]], and promoting organ donation in Australia. |
|||
==Economic aspect== |
|||
Typical expenses during the first year (everything included from surgey, hospitalization, lab testing, medications) averaged of $787,700 in 2008<ref>http://publications.milliman.com/research/health-rr/pdfs/2008-us-organ-tisse-RR4-1-08.pdf 2008 U.S. organ and tissue transplant cost estimates and discussion</ref>.<ref>http://www.transplantliving.org/beforethetransplant/finance/costs.aspx Financing a Transplant</ref> |
|||
==See also== |
|||
*[[Biological pacemaker]] |
|||
*[[Xenographic]] |
|||
==References== |
|||
{{reflist}} |
|||
==External links== |
|||
* [http://www.medicalvideos.us/videos-2062-Heart-Transplant-Video Orthotopic Heart Transplant Video] |
|||
* [http://www.umc.edu/about_us/hardy.html University of Mississippi Medical Center] |
|||
* [http://www.heartpatients.org/page/heart-transplant-patient-guide Patient's Guide to Heart Transplant Surgery] |
|||
* [http://www.childrens.com/Specialties/template.cfm?groupid=2&pageid=46 Heart Transplant at Children's Medical Center] |
|||
*[http://www.heartofcapetown.co.za Official Heart Transplant Museum - Heart Of Cape Town] |
|||
* [http://www.flickr.com/photos/stanfordmedicine/2849110708/ Photograph of first U.S. heart transplant] |
|||
* [http://www.bhf.org.uk/living_with_a_heart_condition/treatment/having_heart_surgery-1/heart_transplant.aspx British Heart Foundation - Information on Heart Transplants] |
|||
* [http://www.stjosephs-phx.org/Medical_Services/Pediatric_Heart_Transplant_Program/index.htm Pediatric Heart Transplant Program - St. Joseph's Hospital and Medical Center] |
|||
* {{cite web | author=Western Cape government, South Africa | title=Chris Barnard Performs World's First Heart Transplant | url=http://www.capegateway.gov.za/eng/pubs/public_info/C/99478# | date=21 February 2005 | publisher=Cape Gateway | accessdate = 2007-01-10}} |
|||
* {{cite web | author=Department of Cardiothoracic Surgery | title=Patient's Guide to Heart Transplant Surgery | url=http://www.cts.usc.edu/ht-pg-hearttransplantprocedure.html | date= | publisher=University of Southern California | accessdate = 2007-01-10}} |
|||
* {{cite web | author=Nancy Reid | title=Heart transplant: How is it performed? | url=http://health.yahoo.com/ency/healthwise/tx4074abc | date=22 September 2005 | publisher=Healthwise | accessdate = 2007-01-10}} |
|||
* {{cite web | author=Jeffrey Everett | title=Heart Transplant: Indications | url=http://health.allrefer.com/health/heart-transplant-indications.html | date=2003-10-29 | publisher=AllRefer.com | accessdate = 2007-01-10}} |
|||
* {{cite web | author= | title=Hartford Hospital Heart Transplant Program | url=http://www.harthosp.org/transplant/heart.htm#indications | date= | publisher=Hartford Hospital, Connecticut, United States | accessdate = 2007-01-10}} |
|||
<!--http://www.americanheart.org/presenter.jhtml?identifier=4588 this link as of 2006-01-10 is broken. Without full citation details, unable to search for any web archive of page--> |
|||
{{Cardiac surgery}} |
|||
{{Organ transplantation}} |
|||
{{DEFAULTSORT:Heart Transplantation}} |
|||
[[Category:Surgical procedures]] |
|||
[[Category:Organ transplants]] |
|||
[[be-x-old:Перасадка сэрца]] |
|||
[[cs:Transplantace srdce]] |
|||
[[da:Hjertetransplantation]] |
|||
[[de:Herztransplantation]] |
|||
[[es:Trasplante de corazón]] |
|||
[[eu:Bihotz-transplante]] |
|||
[[fr:Transplantation cardiaque]] |
|||
[[hi:हृदय प्रत्यारोपण]] |
|||
[[it:Trapianto di cuore]] |
|||
[[la:Translatio cordis]] |
|||
[[hu:Szívátültetés]] |
|||
[[nl:Harttransplantatie]] |
|||
[[ja:心臓移植]] |
|||
[[pl:Przeszczepienie serca]] |
|||
[[pt:Transplante de coração]] |
|||
[[ru:Пересадка сердца]] |
|||
[[simple:Heart transplant]] |
|||
[[sk:Transplantácia srdca]] |
|||
[[sv:Hjärttransplantation]] |
|||
[[uk:Трансплантація серця]] |
|||
[[zh:心脏移植]] |
|||
Revision as of 01:56, 15 February 2011

Hearts transplants, or cardiac transplantation, is a surgical transplant procedure performed on patients with end-stage heart failure or severe coronary artery disease. The most common procedure is to take a working heart from a recently deceased organ donor (cadaveric allograft) and implant it into the patient. The patient's own heart may either be removed (orthotopic procedure) or, less commonly, left in to support the donor heart (heterotopic procedure); both are controversial solutions to one of the most enduring human ailments. Post-operation survival periods now average 15 years.[1]
The world's first human heart transplant was performed by Christiaan Barnard on December 3, 1967 in Cape Town South Africa on a man called Louis Washkansky.[2] The first successful human heart transplant in the United States was performed at Maimonides Medical Center.[3] Worldwide there are 3,500 heart transplants performed every year; about 800,000 people have a Class IV heart defect and need a new organ.[4] This disparity has spurred considerable research into the use of non-human hearts since 1993. It is now possible to take a heart from another species (xenograft), or implant a man-made artificial one, although the outcome of these two procedures has been less successful in comparison to the far more commonly performed allografts. Engineers want to fix the remaining problems with the manufactured options in the next 15 years.[1]
Contraindications
Some patients are less suitable for a heart transplant, especially if they suffer from other circulatory conditions unrelated to the heart. The following conditions in a patient would increase the chances of complications occurring during the operation:
- Kidney, lung, or liver disease
- Insulin-dependent diabetes with other organ dysfunction
- Life-threatening diseases unrelated to heart failure
- Vascular disease of the neck and leg arteries.
- High pulmonary vascular resistance
- Recent thromboembolism
- Age over 60 years (some variation between centres)
- Alcohol, tobacco or drug abuse
Procedures
Pre-operative
A typical heart transplantation begins with a suitable donor heart being located from a recently deceased or brain dead donor, also called a beating heart cadaver. The transplant patient is contacted by a nurse coordinator and instructed to attend the hospital in order to be evaluated for the operation and given pre-surgical medication. At the same time, the heart is removed from the donor and inspected by a team of surgeons to see if it is in a suitable condition to be transplanted. Occasionally it will be deemed unsuitable. This can often be a very distressing experience for an already emotionally unstable patient, and they will usually require emotional support before being sent home. The patient must also undergo many emotional, psychological, and physical tests to make sure that they are in good mental health and will make good use of their new heart. The patient is also given immunosuppressant medication so that their immune system will not reject the new heart.
Operative
Once the donor heart has passed its inspection, the patient is taken into the operating room and given a general anesthetic. Either an orthotopic or a heterotopic procedure is followed, depending on the condition of the patient and the donor heart.
Orthotopic procedure
The orthotopic procedure begins with the surgeons performing a median sternotomy to expose the mediastinum. The pericardium is opened, the great vessels are dissected and the patient is attached to cardiopulmonary bypass. The failing heart is removed by transecting the great vessels and a portion of the left atrium. The pulmonary veins are not transected; rather a circular portion of the left atrium containing the pulmonary veins is left in place. The donor heart is trimmed to fit onto the patient's remaining left atrium and the great vessels are sutured in place. The new heart is restarted, the patient is weaned from cardiopulmonary bypass and the chest cavity is closed.
Heterotopic procedure
In the heterotopic procedure, the patient's own heart is not removed before implanting the donor heart. The new heart is positioned so that the chambers and blood vessels of both hearts can be connected to form what is effectively a 'double heart'. The procedure can give the patients original heart a chance to recover, and if the donor's heart happens to fail (e.g. through rejection), it may be removed, allowing the patient's original heart to start working again. Heterotopic procedures are only used in cases where the donor heart is not strong enough to function by itself (due to either the patient's body being considerably larger than the donor's, the donor having a weak heart, or the patient suffering from pulmonary hypertension).
Post-operative
The patient is taken into ICU to recover. When they wake up, they will be transferred to a special recovery unit in order to be rehabilitated. How long they remain in hospital post-transplant depends on the patient's general health, how well the new heart is working, and their ability to look after their new heart. Doctors typically like the new recipients to leave hospitals soon after surgery because of the risk of infection in a hospital (typically 1 – 2 weeks without any complications). Once the patient is released, they will have to return to the hospital for regular check-ups and rehabilitation sessions. They may also require emotional support. The number of visits to the hospital will decrease over time, as the patient adjusts to their transplant. The patient will have to remain on immunosuppressant medication to avoid the possibility of rejection. Since the vagus nerve is severed during the operation, the new heart will beat at around 100 bpm unless nerve regrowth occurs.
The patient will be monitored to detect rejection of the heart by the body. This surveillance can be performed via frequent biopsy or a genetic expression blood test known as AlloMap Molecular Expression Testing. Typically, biopsy is performed immediately post transplant and then AlloMap blood testing is performed once the patient is stable. The transition from biopsy to AlloMap could occur as soon as 55 days post transplant.
'Living organ' transplant
Doctors made medical history in February 2006, at Bad Oeynhausen Clinic for Thorax- and Cardiovascular Surgery, Germany, when they successfully transplanted a 'beating heart' into a patient.[5] Normally a donor's heart is injected with potassium chloride in order to stop it beating, before being removed from the donor's body and packed in ice in order to preserve it. The ice can usually keep the heart fresh for a maximum of four[6] to six hours with proper preservation, depending on its starting condition. Rather than cooling the heart, this new procedure involves keeping it at body temperature and hooking it up to a special machine called an Organ Care System that allows it to continue beating with warm, oxygenated blood flowing through it. This can maintain the heart in a suitable condition for much longer than the traditional method.
Complications
Post-operative complications include infection, sepsis, organ rejection, as well as the side-effects of the immunosupressive medication. Since the transplanted heart originates from another organism, the recipient's immune system may attempt to reject it. Immunosupressive drugs reduce that risk, but may have some unwanted side effects, such as increased likelihood of infections or nephrotoxic effects.
Prognosis
The prognosis for heart transplant patients following the orthotopic procedure has greatly increased over the past 20 years, and as of June 5, 2009, the survival rates were as follows.[7]
- 1 year: 88% (males), 77.2% (females)
- 3 years: 79.3% (males), 77.2% (females)
- 5 years: 73.1% (males), 67.4% (females)
In a November 2008 study conducted on behalf of the U.S. federal government by Dr. Eric Weiss of the Johns Hopkins University School of Medicine, it was discovered that heart transplants — all other factors being accounted for — work better in same-sex transplants (male to male, female to female). However, due to the present acute shortage in donor hearts, this may not always be feasible.
As of August 2009, Tony Huesman was the world's longest living heart transplant recipient, having survived for 31 years with a transplanted heart. Huesman received a heart in 1978 at the age of 20 after viral pneumonia severely weakened his heart. Huesman died on August 10, 2009 of cancer.[8] The operation was performed at Stanford University under American heart transplant pioneer Dr. Norman Shumway.[9] Another noted heart transplant recipient, Kelly Perkins, climbs mountains around the world to promote positive awareness of organ donation. Perkins is the first heart transplant recipient to climb to the peaks of Mt. Fuji, Mt. Kilimanjaro, the Matterhorn, Mt. Whitney, and Cajon de Arenales in Argentina in 2007, 12 years after her transplant surgery. Dwight Kroening is yet another noted recipient promoting positive awareness for organ donation. Twenty two years after his heart transplant, he is the first to finish an Ironman competition.[10] Fiona Coote was the second Australian to receive a heart transplant in 1984 (at age 14) and the youngest Australian. At 24 years since her transplant she is also a long term survivor and is involved in publicity and charity work for the Red Cross, and promoting organ donation in Australia.
Economic aspect
Typical expenses during the first year (everything included from surgey, hospitalization, lab testing, medications) averaged of $787,700 in 2008[11].[12]
See also
References
- ^ a b Till Lehmann (director) (2007). The Heart-Makers: The Future of Transplant Medicine (documentary film). Germany: LOOKS film and television.
- ^ "Memories of the Heart". Doylestown, Pennsylvania: Daily Intelligencer. November 29, 1987. p. A-18.
{{cite news}}: Italic or bold markup not allowed in:|publisher=(help) - ^ Hoffman, Jascha (2008-11-19). "Dr. Adrian Kantrowitz, Cardiac Pioneer, Dies at 90". The New York Times.
- ^ Reiner Körfer (interviewee) (2007). The Heart-Makers: The Future of Transplant Medicine (documentary film). Germany: LOOKS film and television.
- ^ "Bad Oeynhausen Clinic for Thorax- and Cardiovascular Surgery Announces First Successful Beating Human Heart Transplant". TransMedics. 23 February 2006. Retrieved 2007-05-14.
- ^ Custodiol Htk Solution patient advice including side effects
- ^ Heart Transplants: Statistics The American Heart Association. Retrieved 28 February 2009.
- ^ http://www.columbusdispatch.com/live/content/local_news/stories/2009/08/10/aheart.html?sid=101
- ^ Heart Transplant Patient OK After 28 Yrs (14 September 2006) CBS News. Retrieved 29 December 2006.
- ^ Dwight Kroening first heart transplant to do ironman Retrieved 27 August 2008.
- ^ http://publications.milliman.com/research/health-rr/pdfs/2008-us-organ-tisse-RR4-1-08.pdf 2008 U.S. organ and tissue transplant cost estimates and discussion
- ^ http://www.transplantliving.org/beforethetransplant/finance/costs.aspx Financing a Transplant
External links
- Orthotopic Heart Transplant Video
- University of Mississippi Medical Center
- Patient's Guide to Heart Transplant Surgery
- Heart Transplant at Children's Medical Center
- Official Heart Transplant Museum - Heart Of Cape Town
- Photograph of first U.S. heart transplant
- British Heart Foundation - Information on Heart Transplants
- Pediatric Heart Transplant Program - St. Joseph's Hospital and Medical Center
- Western Cape government, South Africa (21 February 2005). "Chris Barnard Performs World's First Heart Transplant". Cape Gateway. Retrieved 2007-01-10.
- Department of Cardiothoracic Surgery. "Patient's Guide to Heart Transplant Surgery". University of Southern California. Retrieved 2007-01-10.
- Nancy Reid (22 September 2005). "Heart transplant: How is it performed?". Healthwise. Retrieved 2007-01-10.
- Jeffrey Everett (2003-10-29). "Heart Transplant: Indications". AllRefer.com. Retrieved 2007-01-10.
- "Hartford Hospital Heart Transplant Program". Hartford Hospital, Connecticut, United States. Retrieved 2007-01-10.
