Behçet's disease: Difference between revisions
WP:CHECKWIKI error fix for #61. Punctuation goes before References. Do general fixes if a problem exists using AWB (8805) |
Changed outdated ICD-9 code. No research exists to indicate Behcet's is caused by any known infection and currently remains medically unclassified. These codes were written decades ago in the US.. ~JB |
||
| Line 5: | Line 5: | ||
| DiseasesDB = 1285 |
| DiseasesDB = 1285 |
||
| ICD10 = {{ICD10|M|35|2|m|30}} |
| ICD10 = {{ICD10|M|35|2|m|30}} |
||
| ICD9 = {{ICD9| |
| ICD9 = {{ICD9|279.49}} |
||
| ICDO = |
| ICDO = |
||
| OMIM = 109650 |
| OMIM = 109650 |
||
Revision as of 03:00, 25 December 2012
| Behçet's disease | |
|---|---|
| Specialty | Immunology, rheumatology |
Behçet's disease (BEH-chets), sometimes called Behçet's syndrome, Morbus Behçet, or Silk Road disease, is a rare immune-mediated systemic vasculitis[1] that often presents with mucous membrane ulceration and ocular problems. Behçet's disease (BD) was named in 1937 after the Turkish dermatologist Hulusi Behçet, who first described the triple-symptom complex of recurrent oral aphthous ulcers, genital ulcers, and uveitis. As a systemic disease, it can also involve visceral organs such as the gastrointestinal tract, pulmonary, musculoskeletal, cardiovascular and neurological systems. This syndrome can be fatal due to ruptured vascular aneurysms or severe neurological complications.[2]
Signs and symptoms
Skin and mucosa
Nearly all patients present with some form of painful oral mucocutaneous ulcerations in the form of aphthous ulcers or non-scarring oral lesions.[2] The oral lesions are similar to those found in inflammatory bowel disease and can be relapsing.[2] Painful genital ulcerations usually develop around the anus, vulva, or scrotum and cause scarring in 75% of the patients.[2] Additionally, patients may present with erythema nodosum, cutaneous pustular vasculitis, and lesions similar to pyoderma gangrenosum.[2]
Ocular system

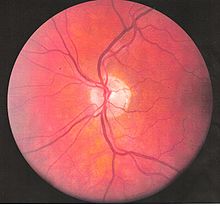
Inflammatory eye disease can develop early in the disease course and lead to permanent vision loss in 20% of cases. Ocular involvement can be in the form of posterior uveitis, anterior uveitis, or retinal vasculitis. Anterior uveitis presents with painful eyes, conjuctival redness, hypopyon, and decreased visual acuity, while posterior uveitis presents with painless decreased visual acuity and visual field floaters. A rare form of ocular (eye) involvement in this syndrome is retinal vasculitis which presents with painless decrease of vision with the possibility of floaters or visual field defects.Cite error: The <ref> tag has too many names (see the help page). Optic nerve atrophy has been identified as the most common cause of visual impairment. Behçet's disease may result in primary or secondary optic nerve involvement. Papilledema as a result of dural sinus thrombosis[3] and atrophy resulting from retinal disease, have been characterized as secondary causes of optic nerve atrophy in Behçet's disease.[4][5]
Signs and symptoms of acute optic neuropathy include painless loss of vision which may affect either one or both eyes, reduced visual acuity, reduced color vision, relative afferent pupillary defect, central scotoma, swollen optic disc, macular edema, or retrobulbar pain. When these symptoms occur with concurrent mucocutaneous ulcerations, they raise suspicion of acute optic neuropathy in Behçet's Disease. Progressive optic atrophy may result in decreased visual acuity or color vision. Intracranial hypertension with papilledema may be present.
Bowels
GI manifestations include abdominal pain, nausea, and diarrhea with or without blood, and they often involve the ileocecal valve.[2] Many patients with BD often complain about abdominal tenderness, bloating, and generic abdominal discomfort that closely mimics irritable bowel syndrome.
Lungs
Lung involvement is typically in the form of hemoptysis, pleuritis, cough, or fever, and in severe cases can be life threatening if the outlet pulmonary artery develops an aneurysm which ruptures causing severe vascular collapse and death from bleeding in the lungs.[2] Nodules, consolidations, cavities and ground glass lesions are common in patients with pulmonary involvement.[6] Pulmonary artery thrombosis may occur.
Musculoskeletal system
Arthralgia is seen in up to half of patients, and is usually a non-erosive poly or oligoarthritis primarily of the large joints of the lower extremities.[2]
Neurological system
Neurological involvements range from aseptic meningitis to vascular thrombosis such as dural sinus thrombosis and organic brain syndrome manifesting with confusion, seizures, and memory loss.[2] They often appear late in the progression of the disease but are associated with a poor prognosis.
Cardiac
Pericarditis is a frequent cardiac manifestation in France.[6]
Cause
The cause is not well-defined, but it is primarily characterized by auto-inflammation of the blood vessels. Although sometimes erroneously referred to as a "diagnosis of exclusion," the diagnosis can sometimes be reached by pathologic examination of the affected areas.[7]
The primary mechanism of the damage is an overactive immune system that seems to target the patient's own body. The involvement of a subset of T cells (Th17) seems to be important.[6] The primary cause is not well known. In fact, as of now, no one knows why the immune system starts to behave this way in Behçet's disease. There does however seem to be a genetic component involved, as first degree relatives of the affected patients are often affected in more than expected proportion for the general population. [citation needed]
An association with the GIMAP family of genes on the long arm of chromosome 7 (7q36.1) has been reported.[8] The genes implicated were GIMAP1, GIMAP2 and GIMAP4.
Pathophysiology

Behçet's disease is considered more prevalent in the areas surrounding the old silk trading routes in the Middle East and in Central Asia. Thus, it is sometimes known as Silk Road Disease. However, this disease is not restricted to people from these regions. A large number of serological studies show a linkage between the disease and HLA-B51.[10] HLA-B51 is more frequently found from the Middle East to South Eastern Siberia, but the incidence of B51 in some studies was 3 fold higher than the normal population. However, B51 tends not to be found in disease when a certain SUMO4 gene variant is involved,[11] and symptoms appear to be milder when HLA-B27 is present.[12] At the current time, a similar infectious origin has not yet been confirmed that leads to Behçet's disease, but certain strains of Streptococcus sanguinis has been found to have a homologous antigenicity.[13]
Vasculitis resulting in occlusion of the vessels supplying the optic nerve may be the cause of acute optic neuropathy and progressive optic atrophy in Behçet's disease. Histological evaluation in a reported case of acute optic neuropathy demonstrated substitution of the axonal portion of the optic nerve with fibrous astrocytes without retinal changes.[5] CNS involvement in Behçet's may lead to intracranial hypertension most commonly due to dural venous sinus thrombosis[3] [8-10] and subsequent secondary optic atrophy.
Diagnosis
There is no specific pathological testing or technique available for the diagnosis of the disease, although the International Study Group criteria for the disease are highly sensitive and specific, involving clinical criteria and a pathergy test.[2][14] Behçet's disease has a high degree of resemblance to diseases that cause mucocutaneous lesions such as Herpes simplex labialis, and therefore clinical suspicion should be maintained until all the common causes of oral lesions are ruled out from the differential diagnosis.
Visual acuity, or color vision loss with concurrent mucocutaneous lesions and/or systemic Behçet's symptoms should raise suspicion of optic nerve involvement in Behçet's disease and prompt a work-up for Behçet's disease if not previously diagnosed in addition to an ocular work-up. Diagnosis of Behçet's disease is based on clinical findings including oral and genital ulcers, skin lesions such as erythema nodosum, acne, or folliculitis, ocular inflammatory findings and a pathergy reaction. Inflammatory markers such ESR, and CRP may be elevated. A complete ophthalmic examination may include a slit lamp examination, optical coherence tomography to detect nerve loss, visual field examinations, fundoscopic examination to assess optic disc atrophy and retinal disease, fundoscopic angiography, and visual evoked potentials, which may demonstrate increased latency. Optic nerve enhancement may be identified on Magnetic Resonance Imaging (MRI) in some patients with acute optic neuropathy. However, a normal study does not rule out optic neuropathy. Cerebrospinal fluid (CSF) analysis may demonstrate elevated protein level with or without pleocytosis. Imaging including angiography may be indicated to identify dural venous sinus thrombosis as a cause of intracranial hypertension and optic atrophy.
Diagnostic guidelines

According to the International Study Group guidelines, for a patient to be diagnosed with Behçet's disease,[14] the patient must have oral (aphthous) ulcers (any shape, size, or number at least 3 times in any 12 months period) along with 2 out of the following 4 "hallmark" symptoms:
- genital ulcers (including anal ulcers and spots in the genital region and swollen testicles or epididymitis in men)
- skin lesions (papulo-pustules, folliculitis, erythema nodosum, acne in post-adolescents not on corticosteroids)
- eye inflammation (iritis, uveitis, retinal vasculitis, cells in the vitreous)
- pathergy reaction (papule >2 mm dia. 24-48 hrs or more after needle-prick). The pathergy test has a specificity of 95% to 100%, but the results are often negative in American and European patients[2]
Despite the inclusive criteria set forth by the International Study Group, there are cases where not all the criteria can be met and therefore a diagnosis cannot readily be made. There is however a set of clinical findings that a physician can rely upon in making a tentative diagnosis of the disease; essentially Behçet's disease does not always follow the International Study Group guidelines and so a high degree of suspicion for a patient who presents having any number of the following findings is necessary:
- mouth ulcers
- arthritis/arthralgia
- nervous system symptoms
- stomach and/or bowel inflammation
- deep vein thrombosis
- superficial thrombophlebitis
- epididymitis
- cardio-vascular problems of an inflammatory origin
- inflammatory problems in chest and lungs
- problems with hearing and/or balance
- extreme exhaustion
- changes of personality, psychoses
- any other members of the family with a diagnosis of Behçet disease.
Treatment
Current treatment is aimed at easing the symptoms, reducing inflammation, and controlling the immune system. High dose Corticosteroid therapy (1 mg/kg/d oral prednisone) is indicated for severe disease manifestations.[15] Anti-TNF therapy such as infliximab has shown promise in treating the uveitis associated with the disease.[16][17] Another Anti-TNF agent, Etanercept, may be useful in patients with mainly skin and mucosal symptoms.[18]
Interferon alfa-2a may also be an effective alternative treatment, particularly for the genital and oral ulcers[19] as well as ocular lesions.[20] Azathioprine, when used in combination with interferon alfa-2b also shows promise,[21] and Colchicine can be useful for treating some genital ulcers, erythema nodosum, and arthritis.[22]
Thalidomide has also been used due to its immune-modifying effect.[23] Dapsone and rebamipide have been shown, in small studies, to have beneficial results for mucocutaneous lesions.[24][25]
Given its rarity, the optimal treatment for acute optic neuropathy in Behçet's disease has not been established. Early identification and treatment is essential. Response to ciclosporin, periocular triamcinolone, and IV methylprednisone followed by oral prednisone has been reported although relapses leading to irreversible visual loss may occur even with treatment.[26] Immunosuppressants such as interferon alpha and tumour necrosis factor antagonists may improve though not completely reverse symptoms of ocular Behçet's, which may progress over time despite treatment. When symptoms are limited to the anterior chamber of the eye prognosis is improved. Posterior involvement, particularly optic nerve involvement is a poor prognostic indicator. Secondary optic nerve atrophy is frequently irreversible. Lumbar puncture or surgical treatment may be required to prevent optic atrophy in cases of intracranial hypertension refractory to treatment with immunomodulators and steroids.
IVIG could be a threatment for servere [27] or complicated cases [28] .[29]
Epidemiology
The syndrome is rare in the United States, but is common in the Middle East and Asia, suggesting a possible cause endemic to the tropical areas.[30] It is not associated with cancer, and links with tissue-types (which are under investigation) are not certain. It also does not follow the usual pattern for autoimmune diseases. However, one study has revealed a possible connection to food allergies, particularly to dairy products.[31] An estimated 15,000 to 20,000 Americans have been diagnosed with this disease. In the UK, it is estimated to have about 1 case for every 100,000 people.[32] Globally, males are affected more frequently than females.[33] In the United States, more females are affected than males.[citation needed]
In an epidemiologic study, 56% of patient’s with Behçet's disease developed ocular involvement at a mean age of 30.[34] Ocular involvement was the first manifestation of Behçet's disease in 8.6% of patients.[34] Ocular Behçet's with involvement of the optic nerve is rarely reported. Among patients with ocular Behçet's disease funduscopic findings of optic atrophy, and optic disc paleness have been identified with a frequency of 17.9% and 7.4%, respectively. Other fundoscopic findings include vascular sheathing(23.7%),[4] retinal hemorrhage(9%),[4] macular edema(11.3%),[4] branch retinal vein occlusion(5.8%),[4] and retinal edema(6.6%).[4] However, optic atrophy was the most significant cause of visual impairment identified in 54% of patients with ocular Behçet's disease and permanent visual impairment.[4]
History
Behçet disease is named after Hulusi Behçet (1889–1948), the Turkish dermatologist and scientist who first recognized the syndrome in one of his patients in 1924 and reported his research on the disease in Journal of Skin and Venereal Diseases in 1936.[35][36] The name (Morbus Behçet) was formally adopted at the International Congress of Dermatology in Geneva in September 1947. Symptoms of this disease may have been described by Hippocrates in the 5th century BC, in his 3rd Epidemion-book.[37] Its first modern formal description was published in 1922.[35]
Some sources use the term "Adamantiades’ syndrome" or "Adamandiades-Behçet syndrome", for the work done by Benediktos Adamantiades.[38] However, the current World Health Organization/ICD-10 standard is "Behçet's disease". In 1991, Saudi Arabian medical researchers described "neuro-Behçet's disease",[39] a neurological involvement in Behçet's disease, considered one of the most devastating manifestations of the disease as investigated by an Egyptian researcher Sahar Saleem.[40] The mechanism can be immune-mediated or thrombotic.[41] The term dates back to at least 1990.[42]
References
- ^ "Glossary,". Archived from the original on 19 April 2009. Retrieved 2009-03-28.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c d e f g h i j k American College of Physicians (ACP). Medical Knowledge Self-Assessment Program (MKSAP-15): Rheumatology. "Systemic vasculitis - Behcet disease." p. 71-73. ISBN 978-1-934465-30-1
- ^ a b Fujikado, T (1994). "Dural sinus thrombosis in Behçet's disease—a case report". Japanese Journal of Ophthalmology. 38 (4): 411–416. PMID 7723211.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c d e f g Ozdal, PC (2002). "Posterior segment involvement in ocular Behçet's disease". European Journal of Ophthalmology. 12 (5): 424–431. PMID 12474927.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ a b Kansu, T (1989). "Optic neuropathy in Behçet's disease". Journal of Clinical Neuro-ophthalmology. 9 (4): 277–280. PMID 2531168.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ^ a b c Hatemi G, Seyahi E, Fresko I, Hamuryudan V (2012) Behçet's syndrome: a critical digest of the recent literature. Clin Exp Rheumatol
- ^ "Behcet Disease: Overview - eMedicine Dermatology". Retrieved 2009-03-28.
- ^ Lee YJ, Horie Y, Wallace GR, Choi YS, Park JA, Song R, Kang YM, Kang SW, Baek HJ, Kitaichi N, Meguro A, Mizuki N, Namba K, Ishida S, Kim J, Niemczek E, Lee EY, Song YW, Ohno S, Lee EB (2012) Genome-wide association study identifies GIMAP as a novel susceptibility locus for Behcet's disease. Ann Rheum Dis
- ^ Ohno, S. (1982). "Close association of HLA-Bw51 with Behcet's disease". Archives of Ophthalmology. 100 (9): 1455–1458. PMID 6956266.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Durrani K, Papaliodis GN (2008). "The genetics of Adamantiades-Behcet's disease". Semin Ophthalmol. 23 (1): 73–9. doi:10.1080/08820530701745264. PMID 18214795.
- ^ Hou S; Yang P; Du L; et al. (2008). "SUMO4 gene polymorphisms in Chinese Han patients with Behcet's disease". Clin. Immunol. 129 (1): 170–5. doi:10.1016/j.clim.2008.06.006. PMID 18657476.
{{cite journal}}: Unknown parameter|author-separator=ignored (help); Unknown parameter|month=ignored (help) - ^ Ahn JK, Park YG (2007). "Human leukocyte antigen B27 and B51 double-positive Behçet uveitis". Arch. Ophthalmol. 125 (10): 1375–80. doi:10.1001/archopht.125.10.1375. PMID 17923546.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Yanagihori H, Oyama N, Nakamura K, Mizuki N, Oguma K, Kaneko F (2006). "Role of IL-12B promoter polymorphism in Adamantiades-Behcet's disease susceptibility: An involvement of Th1 immunoreactivity against Streptococcus Sanguinis antigen". J. Invest. Dermatol. 126 (7): 1534–40. doi:10.1038/sj.jid.5700203. PMID 16514412.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b International Study Group for Behçet's Disease (1990). "Criteria for diagnosis of Behçet's disease". Lancet. 335 (8697): 1078–80. doi:10.1016/0140-6736(90)92643-V. PMID 1970380.
{{cite journal}}: Unknown parameter|month=ignored (help) Cite error: The named reference "pmid1970380" was defined multiple times with different content (see the help page). - ^ CMDT (Current Medical Diagnosis & Treatment) 2007, Chapter 20, page 872
- ^ Sfikakis PP, Theodossiadis PG, Katsiari CG, Kaklamanis P, Markomichelakis NN (2001). "Effect of infliximab on sight-threatening panuveitis in Behcet's disease". Lancet. 358 (9278): 295–6. doi:10.1016/S0140-6736(01)05497-6. PMID 11498218.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sfikakis PP (2002). "Behçet's disease: a new target for anti-tumour necrosis factor treatment". Ann Rheum Dis. 61 Suppl 2 (Suppl 2): ii51–3. doi:10.1136/ard.61.suppl_2.ii51. PMC 1766720. PMID 12379622.
- ^ Melikoglu M, Fresko I, Mat C, Ozyazgan Y, Gogus F, Yurdakul S, Hamuryudan V, Yazici H (2005). "Short-term trial of etanercept in Behcet's disease: a double blind, placebo controlled study". J Rheumatol. 32 (1): 98–105. PMID 15630733.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Alpsoy E, Durusoy C, Yilmaz E, Ozgurel Y, Ermis O, Yazar S, Basaran E (2002). "Interferon alfa-2a in the treatment of Behcet disease: a randomized placebo-controlled and double-blind study". Arch Dermatol. 138 (4): 467–71. doi:10.1001/archderm.138.4.467. PMID 11939808.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kotter I, Zierhut M, Eckstein AK, Vonthein R, Ness T, Gunaydin I, Grimbacher B, Blaschke S, Meyer-Riemann W, Peter HH, Stubiger N (2003). "Human recombinant interferon alfa-2a for the treatment of Behçet's disease with sight threatening posterior or panuveitis". Br J Ophthalmol. 87 (4): 423–31. doi:10.1136/bjo.87.4.423. PMC 1771623. PMID 12642304.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hamuryudan V, Ozyazgan Y, Fresko Y, Mat C, Yurdakul S, Yazici H (2002). "Interferon alfa combined with azathioprine for the uveitis of Behcet's disease: an open study". Isr Med Assoc J. 4 (11 Suppl): 928–30. PMID 12455182.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Yurdakul S, Mat C, Tuzun Y, Ozyazgan Y, Hamuryudan V, Uysal O, Senocak M, Yazici H (2001). "A double-blind trial of colchicine in Behcet's syndrome". Arthritis Rheum. 44 (11): 2686–92. doi:10.1002/1529-0131(200111)44:11<2686::AID-ART448>3.0.CO;2-H. PMID 11710724.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hamuryudan V, Mat C, Saip S, Ozyazgan Y, Siva A, Yurdakul S, Zwingenberger K, Yazici H (1998). "Thalidomide in the treatment of the mucocutaneous lesions of the Behcet syndrome. A randomized, double-blind, placebo-controlled trial". Ann Intern Med. 128 (6): 443–50. PMID 9499327.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Matsuda T, Ohno S, Hirohata S, Miyanaga Y, Ujihara H, Inaba G, Nakamura S, Tanaka S, Kogure M, Mizushima Y (2003). "Efficacy of rebamipide as adjunctive therapy in the treatment of recurrent oral aphthous ulcers in patients with Behcet's disease: a randomised, double-blind, placebo-controlled study". Drugs R D. 4 (1): 19–28. doi:10.2165/00126839-200304010-00002. PMID 12568631.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Sharquie KE, Najim RA, Abu-Raghif AR (2002). "Dapsone in Behcet's disease: a double-blind, placebo-controlled, cross-over study". J Dermatol. 29 (5): 267–79. PMID 12081158.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Voros, G.M., S.S. Sandhu, and R. Pandit, Acute optic neuropathy in patients with Behcet's disease. Report of two cases. Ophthalmologica, 2006. 220(6): p. 400-5.
- ^ Seider; et al. "Intravenous immunoglobulin therapy for resistant ocular Behçet's disease". Br J Ophthalmol. 2001 Nov;85(11):1287-8. Retrieved 13 November 2012.
{{cite web}}: Explicit use of et al. in:|last=(help) - ^ Shutty; et al. "Optimal use of ivig in a patient with Behçet syndrome and common variable immunodeficiency". Ann Allergy Asthma Immunol 109 (2012) 71–84. Retrieved 13 November 2012.
{{cite web}}: Explicit use of et al. in:|last=(help) - ^ Beales, Ian L P. "Gastrointestinal Involvement in Behçet's Syndrome". Nature. Retrieved 13 November 2012.
- ^ Behcet's syndrome (Medline Plus).
- ^ Triolo; et al. (2002). "Humoral and cell mediated immune response to cow's milk proteins in Behçet's disease". Ann Rheum Dis. 61 (5): 459–62. doi:10.1136/ard.61.5.459. PMC 1754076. PMID 11959773.
- ^ Behcet's disease.
- ^ Escudier M, Bagan J, Scully C (2006). "Number VII Behçet's disease (Adamantiades syndrome)". Oral Dis. 12 (2): 78–84. doi:10.1111/j.1601-0825.2005.01144.x. PMID 16476027.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Krause, L.; Köhler, A. K.; Altenburg, A.; Papoutsis, N.; Zouboulis, C. C.; Pleyer, U.; Stroux, A.; Foerster, M. H. (2008). "Ocular involvement in Adamantiades-Behçet's disease in Berlin, Germany". Graefe's Archive for Clinical and Experimental Ophthalmology. 247 (5): 661. doi:10.1007/s00417-008-0983-4.
- ^ a b synd/1863 at Who Named It?
- ^ H. Behçet. Über rezidivierende, aphtöse, durch ein Virus verursachte Geschwüre am Mund, am Auge und an den Genitalien.
Dermatologische Wochenschrift, Hamburg, 1937, 105(36): 1152-1163. Reproduced in Viggor SF, Willis AM, Jawad ASM (2011). "Behçet's disease". Grand Rounds. 11: L1–L2. doi:10.1102/1470-5206.2011.L001.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Johns Hopkins Vasculitis Center (2004). Johns Hopkins Vasculitis Center Discusses Behcets Disease. Retrieved September 9, 2005.
- ^ B. Adamandiades. Sur un cas d'iritis à hypopyon récidivant. Annales d'oculistique, Paris, 1931, 168: 271-278.
- ^ Malhotra Ravi (2004). "Saudi Arabia". Practical Neurology. 4 (3): 184–185. doi:10.1111/j.1474-7766.2004.03-225.x.
- ^ S. Saleem (2005), Neuro-Behçet's Disease: NBD, Neurographics, Vol. 4, Issue 2, Article 1.
- ^ Al-Araji A, Kidd DP (2009). "Neuro-Behçet's disease: epidemiology, clinical characteristics, and management". Lancet Neurol. 8 (2): 192–204. doi:10.1016/S1474-4422(09)70015-8. PMID 19161910.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Su SL, Way LJ, Lin RT, Peng MJ, Wu SC (1990). "Neuro-Behçet's disease: report of three cases with a review of the literature". Gaoxiong Yi Xue Ke Xue Za Zhi. 6 (3): 155–62. PMID 2188002.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
Further reading
- Yamauchi, Y., et al., Suspected simultaneous bilateral anterior ischemic optic neuropathy in a patient with Behcet's disease. Ocul Immunol Inflamm, 2005. 13(4): p. 317-25.
- Brissaud, P., et al., Digital angiography for the diagnosis of dural sinus thrombosis in Behcet's disease. Arthritis Rheum, 1985. 28(3): p. 359-60.
- el-Ramahi, K.M. and M.Z. al-Kawi, Papilloedema in Behcet's disease: value of MRI in diagnosis of dural sinus thrombosis. J Neurol Neurosurg Psychiatry, 1991. 54(9): p. 826-9.
- Fujikado, T. and K. Imagawa, Dural sinus thrombosis in Behcet's disease—a case report. Jpn J Ophthalmol, 1994. 38(4): p. 411-6.
