Epilepsy: Difference between revisions
rm Epilepsy Foundation external link. It wasn't in the right place (Lists of organisations) and their Answerplace is already linked. |
|||
| (One intermediate revision by the same user not shown) | |||
| Line 306: | Line 306: | ||
*[http://www.epilepsyfoundation.org/answerplace/ Answerplace] from the [http://www.epilepsyfoundation.org/ Epilepsy Foundation]. |
*[http://www.epilepsyfoundation.org/answerplace/ Answerplace] from the [http://www.epilepsyfoundation.org/ Epilepsy Foundation]. |
||
<!-- Please keep this list very short. The above set contains those that are particularly comprehensive. --> |
<!-- Please keep this list very short. The above set contains those that are particularly comprehensive. --> |
||
*[http://www.seizures.net Pregnancy and Epilepsy and Epilepsy Info] from the [[North Pacific Epilepsy Research]] |
|||
===Professional resources=== |
===Professional resources=== |
||
Revision as of 18:39, 16 November 2006
| Epilepsy | |
|---|---|
| Specialty | Neurology, epileptology |
| Frequency | 0.9% |
Epilepsy (sometimes referred to as a seizure disorder) is a common chronic neurological condition that is characterized by recurrent unprovoked epileptic seizures.[1][2] These seizures are transient signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain.[3] It affects approximately 50 million people worldwide.[4] Epilepsy is usually controlled, but not cured, with medication – although surgery may be considered in difficult cases. Not all epilepsy syndromes are lifelong, for example some are confined to particular stages of childhood.
Classification
Epilepsies are classified five ways:
- By their first cause (or etiology).
- By the observable manifestations of the seizures, known as "semiology."
- By the location in the brain where the seizures originate.
- As a part of discrete, identifiable medical syndromes.
- By the event that triggers the seizures, as in primary reading epilepsy.
In 1981, the International League Against Epilepsy (ILAE) proposed a classification scheme for individual seizures that remains in common use.[5] This classification is based on observation (clinical and EEG) rather than the underlying pathophysiology or anatomy and is outlined later on in this article. In 1989, the ILAE proposed a classification scheme for epilepsies and epileptic syndromes.[6] This can be broadly described as a two-axis scheme having the cause on one axis and the extent of localisation within the brain on the other. Since 1997, the ILAE have been working on a new scheme that has five axes: ictal phenomenon, seizure type, syndrome, etiology and impairment.[7]
Diagnosis
The diagnosis of epilepsy requires the presence of recurrent, unprovoked seizures; accordingly, it is usually made based on the medical history. EEG, brain MRI, SPECT, PET, and magnetoencephalography may be useful to discover an etiology for the epilepsy, discover the affected brain region, or classify the epileptic syndrome, but these studies are not useful in making the initial diagnosis.
Long-term video-EEG monitoring for epilepsy is the gold standard for diagnosis, but it is not routinely employed owing to its high cost, low availability and inconvenience.
Convulsive or other seizure-like activity, non-epileptic in origin, can be observed in many other medical conditions. These non-epileptic seizures can be hard to differentiate and may lead to misdiagnosis.
Epilepsy covers conditions with different aetiologies, natural histories and prognoses, each requiring different management strategies. A full medical diagnosis requires a definite categorisation of seizure and syndrome types.[8]
Causes
The cause of an individual's epilepsy can be divided into two categories: symptomatic and idiopathic.[6] Symptomatic epilepsies originate due to some structural or metabolic abnormality in the brain. This may be the result of:
- genetic conditions such as tuberous sclerosis and ring chromosome 20 syndrome
- complications during pregnancy or birth
- stroke
- head injury
- neurosurgical operations
- bacterial or viral encephalitis
- parasitical infection
- alcohol
The term cryptogenic is used to describe epilepsy where the cause is suspected to be symptomatic but the underlying illness or damage has not been identified.
The term idiopathic means "a disorder unto itself", and not "cause unknown".[7] No other condition has been implicated as the cause of the epilepsy. Idiopathic epilepsies are often but not exclusively genetic and generalised - for example Juvenile Absence Epilepsy.
Triggers
The diagnosis of epilepsy requires that the seizures be "unprovoked", with the implication that the provocant is assumed to be something obviously harmful. However, in some epilepsy syndromes the provocant can reasonably be considered to be part of normal daily life. Examples of these normal provocants include reading, hot water on the head, hyperventilation, and flashing or flickering lights. This last provocant is a special type of reflex epilepsy called photosensitive epilepsy. Although assumed to be a common trigger for epilepsy, amongst both patients and the public, only around 5% of people with epilepsy are affected by flickering lights.
Certain circumstances can lead to an increased likelihood of seizures in someone with epilepsy or in certain syndromes. For example:
- during sleep
- the transition between sleep and awake
- tiredness
- illness
- constipation
- menstruation
- stress
- alcohol consumption
Epidemiology
The most common ages of incidence are under the age of 18 and over the age of 65. It has been estimated that about 1% of the population meets the diagnostic criteria for epilepsy at any given time, but some theorize that the prevalence may be much higher in fact.
Seizure types
Seizure types are organised firstly according to whether the source of the seizure within the brain is localised (partial or focal onset seizures) or distributed (generalised seizures). Partial seizures are further divided on the extent to which consciousness is affected. If it is unaffected, then it is a simple partial seizure; otherwise it is a complex partial seizure. A partial seizure may spread within the brain - a process known as secondary generalisation. Generalised seizures are divided according to the effect on the body but all involve loss of consciousness. These include absence (petit mal), myoclonic, clonic, tonic, tonic-clonic (grand mal) and atonic seizures.
Seizure syndromes
There are many different epilepsy syndromes, each presenting with its own unique combination of seizure type, typical age of onset, EEG findings, treatment, and prognosis. Below are some common seizure syndromes:
- Infantile spasms (West syndrome) is associated with brain development abnormalities, tuberous sclerosis, and perinatal insults to the brain. It affects infants (as implied by its name), which by definition is between 30 days to 1 year of life. It carries a poor prognosis such that only 5-10% of children with infantile spasms will develop normal to near-normal function, while more than two-thirds will have severe deficits. The typical seizures are characterized by sudden flexor and extensor spasms of head, trunk, and extremities. The key EEG finding in these patients is a hypsarrhythmia, or a high-voltage slow wave with multifocal spikes. The first line treatment for these patients is adrenocorticotropic hormone (ACTH or corticotropin) since traditional antiepileptic drugs generally cannot adequately control seizure activity. Vigabatrin is also used in many countries, and is particularly effective when tuberous sclerosis is the cause of seizures.
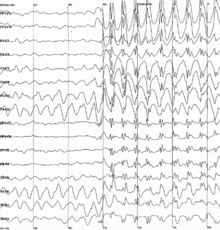
- Childhood absence epilepsy affects children between the ages of 4 and 12 years of age. These patients have recurrent absence seizures that can occur hundreds of times a day. On EEG, one finds the stereotyped generalized 3 Hz spike and wave discharges. A subset of these patients will also develop generalized tonic-clonic seizures. This condition carries a fairly good prognosis in that these children do not usually show cognitive decline or neurological deficits. First line treatment for pure absence seizures is ethosuximide. If patients do not respond or have mixed seizures along with their absence seizures, then valproic acid can be used.
- Benign focal epilepsy of childhood (Benign Rolandic epilepsy) begins in children between the ages of 4 and 13 years. Apart from their seizure disorder, these patients are otherwise normal. Seizures occur at night and sleep promotes secondary generalization. As such, parents only report generalized seizures because focal manifestations are often subtle and go unnoticed. Between seizures, patients have a stereotyped EEG pattern that includes di- or triphasic sharp waves over the central-midtemporal (Rolandic) regions. Prognosis is uniformly good with seizures disappearing by adolescence. Carbamazepine is the first line treatment, though phenytoin and phenobarbital have also been used with some efficacy.
- Juvenile myoclonic epilepsy (JME) begins in patients aged 8 to 20 years. These patients have normal IQ and are otherwise neurologically intact. JME is thought to be genetic, though that is not to say that JME will show in immediate family members. The seizures are morning myoclonic jerks often with generalized tonic-clonic seizures that occur just after waking. 'Petit mal' or absence seizures are less common in cases of JME, but are known to occur more often in young girls. EEG readings reveal generalized spikes with 4-6 Hz spike wave discharges and multiple spike discharges. Interestingly, these patients are often first diagnosed when they have their first generalized tonic-clonic seizure later in life when they experience sleep deprivation (e.g., freshman year in college after staying up late to study for exams). Alcohol is a major contributing factor and those with severe JME should monitor their intake of units. Valproic acid is the first line treatment, whereas carbamazepine can actually worsen symptoms. This condition is lifelong, thus patients must be taught appropriate sleep hygiene to prevent generalized tonic-clonic seizures. The severity of JME varies from person to person - some will experience full blown tonic-clonic seizures regularly, others will suffer only under sufficient stress from lack of sleep and intoxication.
- Temporal lobe epilepsy is the most common epilepsy of adults. In most cases, the epileptogenic region is found in the mesial temporal structures (e.g., the hippocampus, amygdala, and parahippocampal gyrus). Seizures begin in late childhood and adolescence. There is an association with febrile seizures in childhood, and some studies have shown herpes simplex virus (HSV) DNA in these regions, suggesting that perhaps this epilepsy has an infectious etiology. Most of these patients have complex partial seizures sometimes preceded by an aura. If the patient does not respond sufficiently to medical treatment, surgery may be considered.
- Frontal lobe epilepsy
- Lennox-Gastaut syndrome
- Occipital lobe epilepsy
Treatment
Epilepsy is usually treated with medication prescribed by a physician; primary caregivers, neurologists, and neurosurgeons all frequently care for people with epilepsy. In some cases the implantation of a stimulator of the vagus nerve, or a special diet can be helpful. Neurosurgical operations for epilepsy can be palliative, reducing the frequency or severity of seizures; or, in some patients, an operation can be curative.
Responding to a seizure
In most cases, the proper emergency response to a generalized tonic-clonic epileptic seizure is simply to prevent the patient from self-injury by moving him or her away from sharp edges, placing something soft beneath the head, and carefully rolling the person into the recovery position to avoid asphyxiation. In some cases the person may seem to start snoring loudly following a seizure, before coming to. This merely indicates that the person is beginning to breathe properly and does not mean he or she is suffocating. Should the person regurgitate, the material should be allowed to drip out the side of the person's mouth by itself. If a seizure lasts longer than 5 minutes, or if the seizures begin coming in 'waves' one after the other - then Emergency Medical Services should be contacted immediately. Prolonged seizures may develop into status epilepticus, a dangerous condition requiring hospitalization and emergency treatment.
Objects should never be placed in a person's mouth by anybody - including paramedics - during a seizure as this could result in serious injury to either party. Despite common folklore, it is not possible for a person to swallow their own tongue during a seizure. Unfortunately, it is more likely the person will bite their own tongue.
After a seizure, it is typical for a person to be exhausted and confused. Often the person is not immediately aware that they have just had a seizure. During this time one should stay with the person - reassuring and comforting them - until they appear to act as they normally would. In some instances the person may also vomit after coming to. People should not eat or drink until they have returned to their normal level of awareness, and they should not be allowed to wander about unsupervised. Many patients will sleep deeply for a few hours after a seizure - this is common for those having just experienced a more violent type of seizure such as a tonic-clonic. In about 50% of people with epilepsy, headaches may occur after a seizure. These headaches share many features with migraines, and respond to the same medications.
It is helpful if those present at the time of a seizure make note of how long and how severe the seizure was. It is also helpful to note any mannerisms displayed during the seizure. For example, the individual may twist the body to the right or left, may blink, might mumble nonsense words, might pull at clothing. Any observed behaviors, when relayed to a neurologist, may be of help in diagnosing the type of seizure which occured.
Pharmacologic treatment
Some medications can be taken daily in order to prevent seizures altogether or reduce the frequency of their occurrence. These are termed "anticonvulsant" or "antiepileptic" drugs (sometimes AEDs). All such drugs have side effects that are idiosyncratic and others that are dosage-dependent. It is not possible to predict who will suffer from side effects or at what dose the side effects will appear.
Some people with epilepsy will experience a complete remission when treated with an anticonvulsant medication. If this does not occur, the dose of medication may be increased, or another medication may be added to the first. The general strategy is to increase the medication dose until either the seizures are controlled, or until dose-limiting side effects appear; at which point the medication dose is reduced to the highest amount that did not produce undesirable side effects.
Serum levels of AEDs can be checked to determine medication compliance and to assess the effects of drug-drug interactions; some physicians do not use serum levels to fine tune medication, but other physicians believe that serum levels provide excellent data for tailoring medications to suit an individual's specific and relatively variable body chemistry. For example, therapeutic doses (the dose at which seizures are controlled and side effects are minimal and tolerable) may vary widely from among patients. The therapeutic ranges provided by pharmaceutical companies are only ranges and by using blood serum levels and seizures diaries, better seizure control can sometimes be reached. In some cases (such as a seizure flurry) serum levels can be useful to know if the level is very high or very low.
If a person's epilepsy cannot be brought under control after adequate trials of two or three (experts vary here)different drugs, that person's epilepsy is generally said to be 'medically refractory.'
Various drugs may prevent seizures or reduce seizure frequency: these include carbamazepine (common brand name Tegretol), clobazam (Frisium), clonazepam (Klonopin), ethosuximide (Zarontin), felbamate (Felbatol), fosphenytoin (Cerebyx), flurazepam (Dalmane), gabapentin (Neurontin), lamotrigine (Lamictal), levetiracetam (Keppra), oxcarbazepine (Trileptal), mephenytoin (Mesantoin), phenobarbital (Luminal), phenytoin (Dilantin), pregabalin (Lyrica), primidone (Mysoline), sodium valproate (Epilim), tiagabine (Gabitril), topiramate (Topamax), valproate semisodium (Depakote), valproic acid (Depakene, Convulex), and vigabatrin (Sabril).
Other drugs are commonly used to abort an active seizure or interrupt a seizure flurry; these include diazepam (Valium) and lorazepam (Ativan). Drugs used only in the treatment of refractory status epilepticus include paraldehyde (Paral) and pentobarbital (Nembutal).
Bromides were the first of the effective anticonvulsant pure compounds, but are no longer used in humans[9] due to their toxicities and low efficacy.
Surgical treatment
Surgical treatment can be an option for epilepsy when an underlying brain abnormality, such as a benign tumor or an area of scar tissue (e.g. hippocampal sclerosis) can be identified. The abnormality must be removable by a neurosurgeon.
Surgery is usually only offered to patients when their epilepsy has not been controlled by adequate attempts with multiple medications. Before surgery is offered, the medical team conducts many tests to assess whether removal of brain tissue will result in unacceptable problems with memory, vision, language or movement, which are controlled by different parts of the brain. These tests usually include a neuropsychological evaluation, which sometimes includes an intracarotid sodium amobarbital test (Wada test) - although this invasive procedure is being replaced by non-invasive functional MRI in many centres. Resective surgery, as opposed to palliative, successfully eliminates or significantly reduces seizures in about 50-90% of the patients who undergo it (the exact percentage depends on the particulars of the case and surgeon in question.) Many patients decide not to undergo surgery owing to fear or the uncertainty of having a brain operation.
The most common form of resective surgical treatment for epilepsy is to remove the front part of either the right or left temporal lobe. A study of 48 patients who underwent this operation, anterior temporal lobectomy, between 1965 and 1974 determined the long-term success of the procedure. Of the 48 patients, 21 had had no seizures that caused loss of consciousness since the operation. Three others had been free of seizures for at least 19 years. The rest had either never been completely free of seizures or had died between the time of the surgery and commencement of the study.[10]
Palliative surgery for epilepsy is intended to reduce the frequency or severity of seizures. Examples are callosotomy or commissurotomy to prevent seizures from generalizing (spreading to involve the entire brain), which results in a loss of consciousness. This procedure can therefore prevent injury due to the person falling to the ground after losing consciousness. It is performed only when the seizures cannot be controlled by other means. Resective surgery can be considered palliative if it is undertaken with the expectation that it will reduce but not eliminate seizures.
Hemispherectomy is a drastic operation in which most or all of one half of the cerebral cortex is removed. It is reserved for people suffering from the most catastrophic epilepsies, such as those due to Rasmussen syndrome. If the surgery is performed on very young patients (2-5 years old), the remaining hemisphere may acquire some rudimentary motor control of the ipsilateral body; in older patients, paralysis results on the side of the body opposite to the part of the brain that was removed. Because of these and other side effects it is usually reserved for patients who have exhausted other treatment options.
Other treatment
Ketogenic diets may occasionally be effective in controlling some types of epilepsy; although the mechanism behind the effect is not fully understood, shifting of pH towards a metabolic acidosis and alteration of brain metabolism may be involved. Ketogenic diets are high in fat and extremely low in carbohydrates, with intake of fluids often limited. This treatment, originated as early as the 1920s at Johns HopkinsMedical Center, was largely abandoned with the discovery of modern anti-epileptic drugs, but recently has returned to the anti-epileptic treatment arsenal. Ketogenic diets are sometimes prescribed in severe cases where drugs have proven ineffective.
There are several downsides to what initially seems a benign therapy, however. The ketogenic diet is not good for the heart or kidneys and medical problems resulting from the diet have been reported. In addition, the diet is extremely unpalatable and few patients are able to tolerate it for any length of time. Since a single potato chip is adequate to break the ketosis, staying on the diet requires either great willpower or perfect control of a person's dietary intake. People fed via gastrostomy or young children who receive all their food in the presence of a caregiver are better candidates.
Vagus nerve stimulation is a recently developed form of seizure control which uses an implanted electrical device, similar in size, shape and implant location to a heart pacemaker, which connects to the vagus nerve in the neck. Once in place the device can be set to emit electronic pulses, stimulating the vagus nerve at pre-set intervals and milliamp levels. Treatment studies have shown that approximately 50% of those treated in this fashion will show significant seizure reduction.
The Responsive Neurostimulator System (RNS) is currently undergoing clinical study prior to FDA approval. This system relies upon a device implanted just under the scalp. The leads attached to the device are implanted either on the brain surface or in the brain area itself and are located close to the area where the seizures are believed to start. When a seizure begins, an electrical shock is delivered to suppress it. This system is different from the VNS system in that the RNS relies on direct brain stimulation and the RNS is a responsive system. The VNS pulses at predetermined intervals previously set by medical personnel. The RNS system responds to detected signs that a seizures is about to begin and can record events and allow customized response patterns which may provide a greater degree of seizure control.
A seizure response dog is a form of service dog that is trained to summon help or ensure personal safety when a seizure occurs. These are not suitable for everybody and not all dogs can be so trained. Rarely, a dog may develop the ability to sense a seizure before it occurs.
A number of systematic reviews by the Cochrane Collaboration into treatments for epilepsy looked at acupuncture[11], psychological interventions[12], vitamins[13] and yoga[14] and found there is no reliable evidence to support the use of these as treatments for epilepsy.
Pathophysiology
Mutations in several genes have been linked to some types of epilepsy. Several genes that code for protein subunits of voltage-gated and ligand-gated ion channels have been associated with forms of generalized epilepsy and infantile seizure syndromes.[15] Several ligand-gated ion channels have been linked to some types of frontal and generalized epilepsies. Epilepsy-related mutations in some non-ion channel genes have also been identified.
One interesting finding in animals is that repeated low-level electrical stimulation to some brain sites can lead to permanent increases in seizure susceptibility: in other words, a permanent decrease in seizure "threshold." This phenomenon, known as kindling (by analogy with the use of burning twigs to start a larger fire) was discovered by Dr. Graham Goddard in 1967. Chemical stimulation can also induce seizures; repeated exposures to some pesticides have been shown to induce seizures in both humans and animals. One mechanism proposed for this is called excitotoxicity. The roles of kindling and excitotoxicity, if any, in human epilepsy are currently hotly debated.
History and stigma
The word epilepsy is derived from the Greek epilepsia, which in turn can be broken in to epi- (upon) and lepsis (to take hold of, or seizure)[16] In the past, epilepsy was associated with religious experiences and even demonic possession. In ancient times, epilepsy was known as the "Sacred Disease" because people thought that epileptic seizures were a form of attack by demons, or that the visions experienced by persons with epilepsy were sent by the gods. However, in many cultures, persons with epilepsy have been stigmatized, shunned, or even imprisoned; in the Salpêtrière, the birthplace of modern neurology, Jean-Martin Charcot found people with epilepsy side-by-side with the mentally retarded, those with chronic syphilis, and the criminally insane. In Tanzania to this day, as with other parts of Africa epilepsy is associated with possession by evil spirits, witchcraft, or poisoning, and is believed by many to be contagious.[17] In ancient Rome, epilepsy was known as the Morbus Comitialis ('disease of the assembly hall') and was seen as a curse from the gods.
Stigma continues to this day, in both the public and private spheres, but polls suggest it is generally decreasing with time, at least in the developed world; Hippocrates remarked that epilepsy would be considered divine only until it was understood.[18]
Legal implications
Most people diagnosed with epilepsy are forbidden by their local laws from operating vehicles. However, there are usually exceptions for those who can prove that they have stabilized their condition. Those few whose seizures do not cause impairment of consciousness, or whose seizures only arise from sleep, may be exempt from such restrictions, depending on local laws. There is an ongoing debate in bioethics over who should bear the burden of ensuring that an epilepsy patient does not drive a car or fly an airplane.
In the U.S., people with epilepsy can drive if their seizures are controlled with treatment and they meet the licensing requirements in their state. How long they have to be free of seizures varies in different states, but it is most likely to be between three months and a year.[19] [20] The majority of the 50 states place the burden on patients to report their condition to appropriate licensing authorities so that their privileges can be revoked where appropriate. A minority of states (including California) place the burden of reporting on the patient's physician. After reporting is carried out, it is usually the driver's licensing agency that decides to revoke or restrict a driver's license.
In the UK, it is the responsibility of the patient to inform the Driver and Vehicle Licensing Agency (DVLA) if they have epilepsy.[21] The DVLA rules are quite complex[22] , but in summary[23] , those continuing to have seizures or who are within 6 months of medication change may have their license revoked. A doctor who becomes aware that a patient with uncontrolled epilepsy is continuing to drive has, after reminding the patient of their responsibility, a duty to break confidentiality and inform the DVLA. The doctor should advise the patient of the disclosure and the reasons why their failure to notify the agency obliged the doctor to act.
Important investigators of epilepsy
- Galen
- Jean-Martin Charcot
- John Hughlings Jackson
- Hans Berger
- Herbert Jasper
- Wilder Penfield
- H. Houston Merritt
- William G. Lennox
See also
- Seizure
- Non-epileptic seizures
- List of people with epilepsy
- Epilepsy in animals
- Seizure response dog
- Jacksonian seizure
- Photosensitive epilepsy
- Temporal lobe epilepsy
- Abdominal epilepsy
- ISAS (Ictal-Interictal SPECT Analysis by SPM)
Notes and references
- ^ Commission on Epidemiology and Prognosis, International League Against Epilepsy (1993). "Guidelines for epidemiologic studies on epilepsy. Commission on Epidemiology and Prognosis, International League Against Epilepsy". Epilepsia. 34 (4): 592–6. PMID 8330566.
- ^ Blume W, Lüders H, Mizrahi E, Tassinari C, van Emde Boas W, Engel J (2001). "Glossary of descriptive terminology for ictal semiology: report of the ILAE task force on classification and terminology". Epilepsia. 42 (9): 1212–8. PMID 11580774.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fisher R, van Emde Boas W, Blume W, Elger C, Genton P, Lee P, Engel J (2005). "Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE)". Epilepsia. 46 (4): 470–2. doi:10.1111/j.0013-9580.2005.66104.x. PMID 15816939.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Atlas: Epilepsy care in the world 2005 (PDF). World Health Organization. 2005-09-21. p. 3. 9241563036.
- ^ "Proposal for revised clinical and electroencephalographic classification of epileptic seizures. From the Commission on Classification and Terminology of the International League Against Epilepsy". Epilepsia. 22 (4): 489–501. 1981. PMID 6790275.
- ^ a b "Proposal for revised classification of epilepsies and epileptic syndromes. Commission on Classification and Terminology of the International League Against Epilepsy". Epilepsia. 30 (4): 389–99. 1989. PMID 2502382.
- ^ a b Jerome Engel. "A Proposed Diagnostic Scheme For People With Epileptic Seizures And With Epilepsy: Report Of The Ilae Task Force On Classification And Terminology". ILAE. Retrieved 2006-07-18.
- ^ C P Panayiotopoulos and M Koutroumanidis (2005). "The significance of the syndromic diagnosis of the epilepsies". National Society for Epilepsy.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Clemmons DVM, PhD, R.M. (1997). "Seizure Disorders in Dogs and Cats". The Neurology Service at the VMTH. University of Florida’s Veterinary Medical Teaching Hospital. Retrieved 2006-03-29.
- ^ Kelley K, Theodore WH (2005). "Prognosis 30 years after temporal lobectomy". Neurology. 64 (11): 1974–6. PMID 15955959.
- ^ Cheuk D, Wong V (2006). "Acupuncture for epilepsy". Cochrane Database Syst Rev (2): CD005062. PMID 16625622.
- ^ Ramaratnam S, Baker GA, Goldstein LH (2005). "Psychological treatments for epilepsy". Cochrane Database Syst Rev (4): CD002029. PMID 16235293.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ranganathan LN, Ramaratnam S (2005). "Vitamins for epilepsy". Cochrane Database Syst Rev (2): CD004304. PMID 15846704.
- ^ Ramaratnam S, Sridharan K (2000). "Yoga for epilepsy". Cochrane Database Syst Rev (3): CD001524. PMID 10908505.
- ^ Miriam H. Meisler and Jennifer A. Kearney (2005). "Sodium channel mutations in epilepsy and other neurological disorders". Journal of Clinical Investigation. 115 (8): 2010–2017. PMID 16075041 doi:10.1172/JCI25466.
- ^ Harper, Douglas (2001). "epilepsy". Online Etymological Dictionary. Retrieved 2005-06-05.
- ^ Morbus sacer in Africa: some religious aspects of epilepsy in traditional cultures. Jilek-Aall L. PMID: 10080524 Retrieved 8 October 2006.
- ^ Hippocrates quotes
- ^ Epilepsy Foundation Driving and You - Can you drive an automobile if you have epilepsy?.
- ^ Epilepsy Foundation Driver Information by State
- ^ UK Epilepsy Action: Driving and Epilepsy, I've had a seizure. What should I do?
- ^ UK Driver and Vehicle Licensing Agency Guide to the Current Medical Standards Of Fitness to Drive. Full details for doctors regarding epilepsy are given in the Appendix. Information for drivers can be found in Medical Rules - Group 1 Licence Holders
- ^ UK Epilepsy Action: booklet with further details about driving PDF
External links
Patient resources
- Epilepsy information and advice from Epilepsy Action.
- Epilepsy Information Page from the National Institute of Neurological Disorders and Stroke.
- Health Topics: Epilepsy from MedlinePlus.
- Epilepsy.com from the Epilepsy Therapy Development Project.
- Information on epilepsy from the National Society for Epilepsy.
- Answerplace from the Epilepsy Foundation.
- Pregnancy and Epilepsy and Epilepsy Info from the North Pacific Epilepsy Research
Professional resources
- International League Against Epilepsy.
- Epilepsy.com/Professionals from the Epilepsy Therapy Development Project.
- e-epilepsy from the National Society for Epilepsy.
- Seizures and Epilepsy from eMedicine.
Lists of organizations
Many organisations provide regional support for those with epilepsy, their families and professionals in the field. Lists of such groups can be found at:
- International Bureau for Epilepsy (IBE) An umbrella group for various national and regional epilepsy support organisations. For local groups, see their list of chapters and friends.
- The International League Against Epilepsy (ILAE). A list of professional organisations at ILAE: Links.
- The Joint Epilepsy Council of the UK and Ireland - The JEC is an umbrella organisation which exists to represent the united voice of a number of UK and Irish based epilepsy charities.
