Apixaban: Difference between revisions
Carlo Banez (talk | contribs) - link to FDA information |
|||
| Line 18: | Line 18: | ||
| routes_of_administration = Oral |
| routes_of_administration = Oral |
||
| licence_EU = Eliquis |
| licence_EU = Eliquis |
||
| licence_US = Apixaban |
|||
<!--Pharmacokinetic data--> |
<!--Pharmacokinetic data--> |
||
Revision as of 14:09, 7 February 2013
 | |
| Clinical data | |
|---|---|
| Trade names | Eliquis |
| Other names | BMS-562247-01 |
| AHFS/Drugs.com | eliquis |
| License data | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | ca. 50% |
| Elimination half-life | 9–14 h |
| Excretion | 75% biliary, 25% renally |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.167.332 |
| Chemical and physical data | |
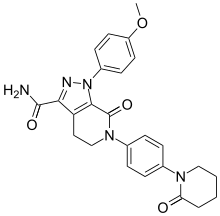
| Formula | C25H25N5O4 |
| Molar mass | 459.497 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Apixaban (INN, trade name Eliquis) is an anticoagulant for the prevention of venous thromboembolism and venous thromboembolic events. It is a direct factor Xa inhibitor. Apixaban has been available in Europe since May 2011 and was approved for preventing venous thromboembolism after elective hip or knee replacement.[2] The FDA approved apixaban in December 2012 with an indication of reducing the risk of stroke and dangerous blood clots (systemic embolism) in patients with atrial fibrillation that is not caused by a heart valve problem.[3] The drug was developed in a joint venture by Pfizer and Bristol-Myers Squibb.[4][5]
Medical uses
Apixaban is used to prevent the formation of blood clots in the veins in adults who have had an operation to replace a hip or knee.
Clinical trials
This section needs more reliable medical references for verification or relies too heavily on primary sources. (September 2012) |  |
In the ADVANCE-2 trial , apixaban 2.5 mg orally twice daily for 10–14 days displayed superiority compared to enoxaparin 40 mg daily for deep venous thromboembolism prophylaxis following knee replacement surgery.[6] However, results of the ADVANCE-1 trial, apixaban 2.5 mg daily compared to enoxaparin 30 mg twice daily, did not meet prespecified noninferiority criteria.[7] Both trials did seem to demonstrate a favorable bleeding profile, when compared to enoxaparin. The ADVANCE-3 trial showed apixaban 2.5 mg twice daily for 35 days was superior to enoxaparin 40 mg in preventing thrombosis in patients undergoing elective hip replacement surgery, with similar bleeding rates.[8][9]
In a systematic review comparing dabigatran, rivaroxaban and apixaban with enoxaparin, for thromboprophylaxis after total hip or knee replacement, the risk of symptomatic venous thromboembolism was lower with rivaroxaban and similar with dabigatran and apixaban; compared with enoxaparin, the relative risk of clinically relevant bleeding was higher with rivaroxaban, similar with dabigatran and lower with apixaban. A higher efficacy of new anticoagulants was generally associated with a higher bleeding tendency. The new anticoagulants did not differ significantly for efficacy and safety.[10]
The ADOPT study: in patients hospitalised for medical reasons and with risk of venous thromboemboli, a long treatment of 25 days with apixaban 2.5 mg twice per day had no significant added value above enoxaparin 40 mg daily for about seven days for the prevention of venous thromboembolic events, but more major hemorrhages occurred.[11]
A 2011 trial, AVERROES, showed, in patients with atrial fibrillation who have failed or are not candidates for vitamin K antagonist therapy, apixaban, 5 mg twice daily, as compared with aspirin at a dose of 81 to 324 mg daily, reduced the risk of stroke or systemic embolism by more than 50% (from 3.7% per year with aspirin to 1.6% per year with apixaban). Major bleeding events were similar for both groups. Difference in death rates did not reach statistical significance. The trial was stopped early because the efficacy of apixaban had been shown. The mean follow-up period up to this date was 1.1 years.[12]
In the ARISTOTLE study, a head-to-head study of apixaban 5 mg twice daily versus warfarin, in patients with atrial fibrillation[13][14] apixaban was not inferior to warfarin (primary endpoint) and was superior in avoiding major bleeding (a key secondary endpoint). In this study 30.5% of patients took aspirin with warfarin. Time within the therapeutic range was mean 62%. Risk for stroke was low: mean CHADS2 score 2.1.[15] A systematic review of new anticoagulants (dabigatran, rivaroxaban and apixaban) stated treatment benefits of apixaban and other new anticoagulants compared with warfarin are small and vary depending on the control achieved by warfarin treatment. In atrial fibrillation, they decreased all-cause mortality. Numbers needed to treat were 125 for two years of treatment with new anticoagulants against warfarin. Adverse effects of new anticoagulants compared with warfarin were lower for fatal bleeding and hemorrhagic stroke, numerically lower for major bleeding, numerically higher for gastrointestinal bleeding, and higher for discontinuation due to adverse events. Bleeding risks may be increased for persons older than 75 years or those receiving warfarin who have good control.[16]
A systematic review on data of clinical trials with dabigatran, rivaroxaban and apixaban in atrial fibrillation suggests all three agents are at least as efficacious as dose-adjusted warfarin, with similar major bleeding profiles. For patients who are unwilling to adhere to regular coagulation monitoring or whose therapeutic effect using warfarin is not optimal despite adequate monitoring and management, they may provide alternatives in anticoagulation.[17] An indirect comparison study of these agents suggests apixaban is associated with less major bleeding than dabigatran 150 mg or rivaroxaban, and rivaroxaban is less effective than dabigatran 150 mg in preventing stroke or systemic embolism. Such an indirect comparison should be used only to generate hypotheses which need to be tested in a dedicated, randomised trial comparing the three drugs directly.[18] Another indirect comparison of these agents indicates that, in patients with a CHADS2 score ≥3, dabigatran 150 mg, apixaban 5 mg, and rivaroxaban 20 mg resulted in statistically similar rates of stroke and systemic embolism, but apixaban had a lower risk of major hemorrhage compared with dabigatran and rivaroxaban.[19]
No head-to-head trials of new anticoagulants or large-scale observational studies have been conducted to reflect routine and long-term use of these agents.[16]
A 2011 trial, APPRAISE-2, showed patients receiving apixaban 5 mg twice daily against placebo after acute coronary syndrome experienced an 150% increased rate of major bleeding episodes without a significant reduction in recurrent ischemic events, so the trial was terminated early. A greater number of intracranial and fatal bleeding events occurred with apixaban than with placebo. With a median follow up of 241 days, absolute risk increase for Timi major bleeding was 0.8%, for Timi major and minor bleeding 1.4%, for fatal bleeding 0.1%, for intracranial bleeding 0.2% and for any bleeding 10.1% against placebo. The majority of the patients (81%) were receiving aspirin plus a P2Y12-receptor antagonist, predominantly clopidogrel. The increase in bleeding events with apixaban, as compared with placebo, was seen both in patients taking combination antiplatelet therapy and in patients taking aspirin alone. More patients discontinued apixaban than the placebo drug. The most common reasons for discontinuation of the study drug were adverse events (8.5% in the apixaban group vs. 6.5% in the placebo group) and withdrawal of consent (5.3% vs. 4.2%).[20] The trial points to the possible real-world dangers of adding new anticoagulants to combination antiplatelet therapy. A meta-analysis has concluded the new anticoagulants (anti-Xa or direct thrombin inhibitors) give a small benefit when added to dual antiplatelet therapy in acute coronary syndrome, but an unacceptably high rate of bleeding.[21]
See also
References
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 Oct 2023.
- ^ "ELIQUIS® (apixaban) Approved In Europe For Preventing Venous Thromboembolism After Elective Hip Or Knee Replacement" (Press release). Pfizer. April 20, 2012. Retrieved 2012-05-29.
- ^ "FDA approves Eliquis to reduce the risk of stroke, blood clots in patients with non-valvular atrial fibrillation". FDA. Retrieved 2012-12-30.
- ^ "Bristol-Myers Squibb News Release 26 April 2007". Archived from the original on 11 September 2007. Retrieved 2007-09-15.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Nainggolan, Lisa. "Apixaban better than European enoxaparin regimen for preventing VTE". Retrieved 2011-04-01.
- ^ Lassen, Michael Rud; Raskob, Gary E; Gallus, Alexander; Pineo, Graham; Chen, Dalei; Hornick, Philip; Advance-2, Investigators (2010). "Apixaban versus enoxaparin for thromboprophylaxis after knee replacement (ADVANCE-2): A randomised double-blind trial". The Lancet. 375 (9717): 807–15. doi:10.1016/S0140-6736(09)62125-5. PMID 20206776.
{{cite journal}}: CS1 maint: numeric names: authors list (link) - ^ Lassen, Michael Rud; Raskob, Gary E.; Gallus, Alexander; Pineo, Graham; Chen, Dalei; Portman, Ronald J. (2009). "Apixaban or Enoxaparin for Thromboprophylaxis after Knee Replacement". New England Journal of Medicine. 361 (6): 594–604. doi:10.1056/NEJMoa0810773. PMID 19657123.
- ^ Lassen, Michael Rud; Gallus, Alexander; Raskob, Gary E.; Pineo, Graham; Chen, Dalei; Ramirez, Luz Margarita; Advance-3, Investigators (2010). "Apixaban versus Enoxaparin for Thromboprophylaxis after Hip Replacement". New England Journal of Medicine. 363 (26): 2487–98. doi:10.1056/NEJMoa1006885. PMID 21175312.
{{cite journal}}: CS1 maint: numeric names: authors list (link) - ^ Nainggolan, Lisa. "Apixaban better than European enoxaparin regimen for preventing VTE". theheart.org by WebMD. Retrieved 2011-04-01.
- ^ Gomez-Outes, A.; Terleira-Fernandez, A. I.; Suarez-Gea, M. L.; Vargas-Castrillon, E. (2012). "Dabigatran, rivaroxaban, or apixaban versus enoxaparin for thromboprophylaxis after total hip or knee replacement: Systematic review, meta-analysis, and indirect treatment comparisons". BMJ. 344: e3675. doi:10.1136/bmj.e3675. PMC 3375207. PMID 22700784.
- ^ Goldhaber, Samuel Z.; Leizorovicz, Alain; Kakkar, Ajay K.; Haas, Sylvia K.; Merli, Geno; Knabb, Robert M.; Weitz, Jeffrey I.; Adopt Trial, Investigators (2011). "Apixaban versus Enoxaparin for Thromboprophylaxis in Medically Ill Patients". New England Journal of Medicine. 365 (23): 2167–77. doi:10.1056/NEJMoa1110899. PMID 22077144.
- ^ Connolly, Stuart J.; Eikelboom, John; Joyner, Campbell; Diener, Hans-Christoph; Hart, Robert; Golitsyn, Sergey; Flaker, Greg; Avezum, Alvaro; Hohnloser, Stefan H. (2011). "Apixaban in Patients with Atrial Fibrillation". New England Journal of Medicine. 364 (9): 806–17. doi:10.1056/NEJMoa1007432. PMID 21309657.
- ^ Clinical trial number NCT00412984 for "Apixaban for the Prevention of Stroke in Subjects With Atrial Fibrillation (ARISTOTLE)" at ClinicalTrials.gov
- ^ Granger, Christopher B.; Alexander, John H.; McMurray, John J.V.; Lopes, Renato D.; Hylek, Elaine M.; Hanna, Michael; Al-Khalidi, Hussein R.; Ansell, Jack; Atar, Dan (2011). "Apixaban versus Warfarin in Patients with Atrial Fibrillation". New England Journal of Medicine. 365 (11): 981–92. doi:10.1056/NEJMoa1107039. PMID 21870978.
- ^ Husten L (2011-06-22). "ELIQUIS® (apixaban) Meets Primary and Key Secondary Endpoints in Phase 3 ARISTOTLE Study". CardioBrief. WordPress.com. Retrieved 2011-06-23.
- ^ a b Adam, Soheir S.; McDuffie, Jennifer R.; Ortel, Thomas L.; Williams, John W. (2012). "Comparative Effectiveness of Warfarin and New Oral Anticoagulants for the Management of Atrial Fibrillation and Venous Thromboembolism: A Systematic Review". Annals of Internal Medicine. PMID 22928173.
- ^ O'Dell, Kate M.; Igawa, Daniel; Hsin, Jerline (2012). "New Oral Anticoagulants for Atrial Fibrillation: A Review of Clinical Trials". Clinical Therapeutics. 34 (4): 894–901. doi:10.1016/j.clinthera.2012.01.019. PMID 22417716.
- ^ Mantha, S.; Ansell, J. (2012). "An indirect comparison of dabigatran, rivaroxaban and apixaban for atrial fibrillation". Thrombosis and Haemostasis. 108 (3): 476–84. doi:10.1160/TH12-02-0093. PMID 22740145.
- ^ Schneeweiss, S.; Gagne, J. J.; Patrick, A. R.; Choudhry, N. K.; Avorn, J. (2012). "Comparative Efficacy and Safety of New Oral Anticoagulants in Patients with Atrial Fibrillation". Circulation: Cardiovascular Quality and Outcomes. 5 (4): 480–6. doi:10.1161/CIRCOUTCOMES.112.965988. PMID 22787066.
- ^ Alexander, John H.; Lopes, Renato D.; James, Stefan; Kilaru, Rakhi; He, Yaohua; Mohan, Puneet; Bhatt, Deepak L.; Goodman, Shaun; Verheugt, Freek W. (2011). "Apixaban with Antiplatelet Therapy after Acute Coronary Syndrome". New England Journal of Medicine. 365 (8): 699–708. doi:10.1056/NEJMoa1105819. PMID 21780946.
- ^ Komócsi A, Vorobcsuk A, Kehl D, et al. Use of new-generation oral anticoagulant agents in patients receiving antiplatelet therapy after an acute coronary syndrome. Arch Intern Med 2012; DOI:10.1001/archinternmed.2012.4026. http://archinte.jamanetwork.com/article.aspx?articleid=1362940
