Thyroid: Difference between revisions
General Tojo (talk | contribs) revert to more informative prior version |
General Tojo (talk | contribs) →General: correction of errors |
||
| Line 7: | Line 7: | ||
==General== |
==General== |
||
The thyroid |
The thyroid gland is a double-lobed structure located in the neck, just below the larynx. The hormone produced by the thyroid gland is thyroxine. Thyroxine controls the individual's rate of metabolism. The hormone must be present in a definite amount. Oversecretion of the hormone results in very rapid metabolism, and undersecretion results in a lowered rate of metabolism. Ioidine is a very important part of thyroxine. So a supply of iodine in the diet is essential. An iodine deficiency results in the thyroid gland enlarging in an attempt to produce the required amount of the hormone.{{ref_label|general|3|}} |
||
==Anatomy== |
==Anatomy== |
||
Revision as of 14:45, 21 June 2006

The thyroid is one of the larger endocrine glands in the body. It is located in the neck and produces hormones, principally thyroxine (T4) and triiodothyronine (T3), that regulate the rate of metabolism and affect the growth and rate of function of many other systems in the body.
General
The thyroid gland is a double-lobed structure located in the neck, just below the larynx. The hormone produced by the thyroid gland is thyroxine. Thyroxine controls the individual's rate of metabolism. The hormone must be present in a definite amount. Oversecretion of the hormone results in very rapid metabolism, and undersecretion results in a lowered rate of metabolism. Ioidine is a very important part of thyroxine. So a supply of iodine in the diet is essential. An iodine deficiency results in the thyroid gland enlarging in an attempt to produce the required amount of the hormone.[3]
Anatomy
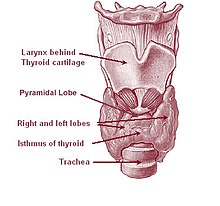
The thyroid is situated on the front side of the neck, at the level of C5 to T1 vertebral bodies, just below the laryngeal prominence (Adam's apple), near the thyroid cartilage over the trachea but covered by layers of skin and muscle. The thyroid is one of the larger endocrine glands - 10-20 grams in adults- and butterfly-shaped: the wings correspond to the lobes and the body to the isthmus of the thyroid. It may enlarge substantially during pregnancy and when affected by a variety of diseases.
Blood supply
The thyroid gland is supplied by two pairs of arteries: the superior and inferior thyroid arteries of each side. The superior thyroid artery is the first branch of the external carotid, and supplies mostly the upper half of the thyroid gland, while the inferior thyroid artery is the major branch of the thyrocervical trunk, which comes off of the subclavian artery. In 10% of people, there is an additional thyroid artery, the thyreoidea ima, that arises from the brachiocephalic trunk or the arch of the aorta. Lymph drainage follows the arterial supply.
There are three main veins that drain the thyroid to the superior vena cava: the superior, middle and inferior thyroid veins.
Embryologic development
In the fetus, at 3-4 weeks of gestation, the thyroid gland appears as an epithelial proliferation in the floor of the pharynx at the base of the tongue between the tuberculum impar and the copula at a point latter indicated by the foramen cecum. Subsequently the thyroid descends in front of the pharyngeal gut as a bilobed diverticulum through the thyroglossal duct. Over the next few weeks, it migrates to the base of the neck. During migration, the thyroid remains connected to the tongue by a narrow canal, the thyroglossal duct.
Follicles of the thyroid begin to make colloid in the 11th week and thyroxine by the 18th week.
Histology of the thyroid
The thyroid is composed of spherical follicles that selectively absorb iodine (as iodide ions, I-) from the blood and for production of thyroid hormones. Twenty-five percent of all the body I- is in the thyroid gland. The follicles are made of a single layer of thyroid epithelial cells, which secrete T3 and T4. Inside the follicles is a colloid which is rich in a protein called thyroglobulin. The colloidal material serves as a reservoir of materials for thyroid hormone production and, to a lesser extent, a reservoir of the hormones themselves. Scattered among follicular cells and in spaces between the spherical follicles are another type of thyroid cell, parafollicular cells or C cells, which secrete calcitonin.
Physiology
The primary function of the thyroid is production of the hormones thyroxine (T4), triiodothyronine (T3), and calcitonin. Up to 40% of the T4 is converted to T3 by peripheral organs such as the liver, kidney and spleen. T3 is about ten times more active than T4[1].
T3 and T4 production and action
Thyroxine is synthesised by the follicular cells from the tyrosine residues of the protein called thyroglobulin (TG). Iodine, captured with the "iodine trap" is activated by the enzyme thyroid peroxidase (TPO) and linked to the 3' and 5' sites of the benzene ring of the tyrosine residues on TG. Upon stimulation by TSH (see below), the follicular cells reabsorb TG and proteolytically cleave the iodinated tyrosines from TG, forming T4 and T3 (in T3, one iodine is absent compared to T4), and releasing them into the blood. Thyroid hormone that is secreted from the gland is about 90% T4 and about 10% T3[1].
Cells of the brain are a major target for thyroid hormone. A transport protein (OATP1C1) has been identified that seems to be important for T4 transport across the blood brain barrier[2]. A second transport protein (MCT8) is important for T3 transport across brain cell membranes[2].
In the blood, T4 and T3 are partially bound to thyroxine-binding globulin, transthyretin and albumin. Only a very small fraction of the circulating hormone is free (unbound) - T4 0.03% and T3 0.3%. Only the free fraction has hormonal activity. As with the steroid hormones and retinoic acid, thyroid hormones cross the cell membrane and bind to intracellular receptors (α1, α2, β1 and β2), which act alone, in pairs or together with the retinoid X-receptor as transcription factors to modulate DNA transcription[1].
T3 and T4 regulation
The production of thyroxine is regulated by thyroid-stimulating hormone (TSH), released by the pituitary. The thyroid and thyrotropes form a negative feedback loop: TSH production is suppressed when the T4 levels are high, and vice versa. The TSH production itself is modulated by thyrotropin-releasing hormone, which is produced by the hypothalamus and secreted at an increased rate in situations such as cold (in which an accelerated metabolism would generate more heat). TSH production is blunted by somatostatin (SRIH).
Calcitonin
An additional hormone produced by the thyroid contributes to the regulation of blood calcium levels. Parafollicular cells produce calcitonin in response to hypercalcemia. Calcitonin stimulates movement of calcium into bone, in opposition to the effects of parathyroid hormone. However calcitonin seems far less essential than PTH, as calcium metabolism remains clinically normal after removal of the thyroid, but not the parathyroids.
Calcitonin can be used therapeutically for the treatment of hypercalcemia or osteoporosis.
The significance of iodine
In areas of the world where iodine - essential for the production of thyroxine, which contains four iodine atoms - is lacking in the diet, the thyroid gland can be considerably enlarged, resulting in the swollen necks of endemic goitre.
Thyroxine is critical to the regulation of metabolism and growth, throughout the animal kingdom. Among amphibians, for example, administering a thyroid-blocking agent such as propylthiouracil (PTU) can prevent tadpoles from metamorphosing into frogs; conversely, administering thyroxine will trigger metamorphosis.
In humans, children born with thyroid hormone deficiency will not grow well, and brain development can be severely impaired, in the condition referred to as cretinism. Newborn children in many developed countries are now routinely tested for thyroid hormone deficiency as part of newborn screening by analysis of a drop of blood. Children with thyroid hormone deficiency are treated by supplementation with synthetic thyroxine, which enables them to grow and develop normally.
Because of the thyroid's selective uptake and concentration of what is a fairly rare element, it is sensitive to the effects of various radioactive isotopes of iodine produced by nuclear fission. In the event of large accidental releases of such material into the environment, the uptake of radioactive iodine isotopes by the thyroid can, in theory, be blocked by saturating the uptake mechanism with a large surplus of non-radioactive iodine, taken in the form of potassium iodide tablets. While biological researchers making compounds labelled with iodine isotopes do this, in the wider world such preventive measures are usually not stockpiled before an accident, nor are they distributed adequately afterward - one consequence of the Chernobyl disaster was an increase in thyroid cancers in children in the years following the accident. [2]
Iodised salt is a cheap and easy way of adding iodine to the diet. This has eliminated endemic cretinism in most developed countries, and some governments have made the iodination of flour mandatory.
Diseases of the thyroid gland
Hyper- and hypofunction (affects about 2% of the population):
- Hypothyroidism (underactivity)
- Hashimoto's thyroiditis / thyroiditis
- Ord's thyroiditis
- Postoperative hypothyroidism
- Postpartum thyroiditis
- Silent thyroiditis
- Acute thyroiditis
- Iatrogenic hypothyroidism
- Hyperthyroidism (overactivity)
- Thyroid storm
- Graves-Basedow disease
- Toxic thyroid nodule
- Toxic nodular struma (Plummer's disease)
- Hashitoxicosis
- Iatrogenic hyperthyroidism
- De Quervain thyroiditis (inflammation starting as hyperthyroidism, can end as hypothyroidism)
Anatomical problems:
- Goitre
- Lingual thyroid
- Thryoglossal duct cyst
Tumors:
- Thyroid adenoma
- Thyroid cancer
- Papillary
- Follicular
- Medullary
- Anaplastic
- Lymphomas and metastasis from elsewhere (rare)
Deficiencies:
Medication linked to thyroid disease includes amiodarone, lithium salts, some types of interferon and IL-2.
Diagnosis
The measurement of thyroid-stimulating hormone (TSH) levels is often used by doctors as a screening test. Elevated TSH levels can signify an inadequate hormone production, while suppressed levels can point at excessive unregulated production of hormone. If TSH is abnormal, decreased levels of thyroid hormones T4 and T3 may be present; these may be determined to confirm this. Autoantibodies may be detected in various disease states (anti-TG, anti-TPO, TSH receptor stimulating antibodies). Infrequently, TBG and transthyretin levels may be abnormal; these are not routinely tested.
Nodules of the thyroid may require ultrasound to establish their nature, and fine needle aspiration may be performed. Scintigraphy with iodine-131 may reveal whether parts of the thyroid are abnormally active or inactive.
Treatment
Medical treatment
Levothyroxine is a stereoisomer of thyroxine which is degraded much slower and can be administered once daily in patients with hypothyroidism.
Graves' disease may be treated with the thioamide drugs propylthiouracil, carbimazole or methimazole, or rarely with Lugol's solution. Hyperthyroidism as well as thyroid tumors may be treated with radioactive iodine.
Thyroid surgery
Thyroid surgery is performed for a variety of reasons. A nodule or lobe of the thyroid is sometimes removed for biopsy or for the presence of an autonomously functioning adenoma causing hyperthyroidism. A large majority of the thyroid may be removed, a subtotal thyroidectomy, to treat the hyperthyroidism of Graves' disease, or to remove a goitre that is unsightly or impinges on vital structures. A complete thyroidectomy of the entire thyroid, including associated lymph nodes, is the preferred treatment for thyroid cancer. Removal of the bulk of the thyroid gland usually produces hypothyroidism, unless the person takes thyroid hormone replacement.
If the thyroid gland must be removed surgically, care must be taken to avoid damage to adjacent structures, the parathyroid glands and the recurrent laryngeal nerve. Both are susceptible to accidental removal and/or injury during thyroid surgery. The parathyroid glands produce parathyroid hormone (PTH), a hormone needed to maintain adequate amounts of calcium in the blood. Removal results in hypoparathyroidism and a need for supplemental calcium and vitamin D each day. The recurrent laryngeal nerves provide motor control for all external muscles of the larynx except for the cricothyroid muscle, also runs along the posterior thyroid. Accidental laceration of either of the two or both recurrent laryngeal nerves may cause paralysis of the vocal cords and their associated muscles, changing the voice quality.
History
The thyroid was first identified by the anatomist Thomas Wharton (whose name is also eponymised in Wharton's duct of the submandibular gland) in 1656. Thyroid hormone (or thyroxin) was only identified in the 19th century.
References
- ^ a b The thyroid gland in Endocrinology: An Integrated Approach by Stephen Nussey and Saffron Whitehead (2001) Published by BIOS Scientific Publishers Ltd. ISBN 1859962521.
- ^ a b "Thyroid hormone transporters in health and disease" by Jurgen Jansen, Edith C. H. Friesema, Carmelina Milici and Theo J. Visser in Thyroid (2005) Volume 15, pages 757-768. PMID 16131319.
- ^ Kld Referencer's Rpg
External links
- Thyroid, a medical journal devoted to thyroid research.
- Thyroid Disease Manager (free online textbook)
- Thyroid Disease (Nuclear Medicine Information)
