Iron-deficiency anemia: Difference between revisions
m →Cause |
→Cause: moved children into its own category |
||
| Line 58: | Line 58: | ||
A diagnosis of iron-deficiency anemia requires further investigation into its cause.<ref name=":3"/> It can be caused by increased iron demand, increased iron loss, or decreased iron intake.<ref name=npsnews>{{cite web |url=http://www.nps.org.au/health_professionals/publications/nps_news/current/iron_anaemia |title=NPS News 70: Iron deficiency anaemia |publisher=NPS Medicines Wise |date=October 1, 2010 |accessdate=November 5, 2010 |deadurl=no |archiveurl=https://web.archive.org/web/20110222125316/http://www.nps.org.au/health_professionals/publications/nps_news/current/iron_anaemia |archivedate=February 22, 2011 |df= }}</ref> Increased iron demand often occurs during periods of growth, such as in children and pregnant women.<ref name=":13">{{Cite book|title=Henry's Clinical Diagnosis and Management by Laboratory Methods|last=M. Tarek Elghetany, Katherine I. Schexneider and Katalin Banki|first=|publisher=Elsevier|year=2017|isbn=|location=|pages=559-605}}</ref> For example, during stages of rapid growth, babies and adolescents may outpace dietary intake of iron which can result in deficiency in the absence of disease or a grossly abnormal diet.<ref name="npsnews" /> Iron loss is typically from blood loss. <ref name=":13" /> One example of blood loss is by chronic [[Gastrointestinal bleeding|gastrointestinal blood loss]], which could be linked to a possible [[Cancer|malignancy]].<ref name=":3"/> In women of childbearing age, [[Menorrhagia|heavy menstrual periods]] can be a source of blood loss and can also cause iron-deficiency anemia.<ref name=":3"/> People who do not consume much iron in their diet, such as vegan or vegetarian diets, are at increased risk of developing iron deficiency anemia due to low iron intake.<ref name=":10"/> |
A diagnosis of iron-deficiency anemia requires further investigation into its cause.<ref name=":3"/> It can be caused by increased iron demand, increased iron loss, or decreased iron intake.<ref name=npsnews>{{cite web |url=http://www.nps.org.au/health_professionals/publications/nps_news/current/iron_anaemia |title=NPS News 70: Iron deficiency anaemia |publisher=NPS Medicines Wise |date=October 1, 2010 |accessdate=November 5, 2010 |deadurl=no |archiveurl=https://web.archive.org/web/20110222125316/http://www.nps.org.au/health_professionals/publications/nps_news/current/iron_anaemia |archivedate=February 22, 2011 |df= }}</ref> Increased iron demand often occurs during periods of growth, such as in children and pregnant women.<ref name=":13">{{Cite book|title=Henry's Clinical Diagnosis and Management by Laboratory Methods|last=M. Tarek Elghetany, Katherine I. Schexneider and Katalin Banki|first=|publisher=Elsevier|year=2017|isbn=|location=|pages=559-605}}</ref> For example, during stages of rapid growth, babies and adolescents may outpace dietary intake of iron which can result in deficiency in the absence of disease or a grossly abnormal diet.<ref name="npsnews" /> Iron loss is typically from blood loss. <ref name=":13" /> One example of blood loss is by chronic [[Gastrointestinal bleeding|gastrointestinal blood loss]], which could be linked to a possible [[Cancer|malignancy]].<ref name=":3"/> In women of childbearing age, [[Menorrhagia|heavy menstrual periods]] can be a source of blood loss and can also cause iron-deficiency anemia.<ref name=":3"/> People who do not consume much iron in their diet, such as vegan or vegetarian diets, are at increased risk of developing iron deficiency anemia due to low iron intake.<ref name=":10"/> |
||
| ⚫ | Children who are at risk for iron-deficiency anemia include:<ref>{{Cite book|url=https://www.worldcat.org/oclc/952123506|title=American Academy of Pediatrics textbook of pediatric care|others=McInerny, Thomas K.,, American Academy of Pediatrics.|isbn=9781610020473|edition= |
||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
=== Parasitic disease === |
=== Parasitic disease === |
||
| Line 103: | Line 91: | ||
=== Babies === |
=== Babies === |
||
Babies are at increased risk of developing iron deficiency anemia due to their rapid growth.<ref name=":13" /> Their need for iron is greater than they are getting in their diet.<ref name=":13" /> Babies are born with iron stores; however, these iron stores typically run out by 4-6 months of ago. In addition, infants who are given cow's milk too early can develop anemia due to gastrointestinal blood loss.<ref name=":13" /> |
Babies are at increased risk of developing iron deficiency anemia due to their rapid growth.<ref name=":13" /> Their need for iron is greater than they are getting in their diet.<ref name=":13" /> Babies are born with iron stores; however, these iron stores typically run out by 4-6 months of ago. In addition, infants who are given cow's milk too early can develop anemia due to gastrointestinal blood loss.<ref name=":13" /> |
||
=== Children === |
|||
| ⚫ | Children who are at risk for iron-deficiency anemia include:<ref>{{Cite book|url=https://www.worldcat.org/oclc/952123506|title=American Academy of Pediatrics textbook of pediatric care|others=McInerny, Thomas K.,, American Academy of Pediatrics.|isbn=9781610020473|edition=2nd|location=[Elk Grove Village, IL]|oclc=952123506}}</ref> |
||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
=== Blood donors === |
=== Blood donors === |
||
Revision as of 21:24, 11 December 2018
| Iron-deficiency anemia | |
|---|---|
| Other names | Iron-deficiency anaemia |
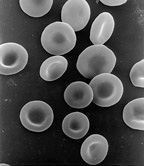 | |
| Red blood cells | |
| Specialty | Hematology |
| Symptoms | Feeling tired, weakness, shortness of breath, confusion, pallor[1] |
| Complications | Heart failure, arrhythmias, frequent infections[2] |
| Causes | Iron deficiency[3] |
| Diagnostic method | Blood tests[4] |
| Treatment | Dietary changes, medications, surgery[3] |
| Medication | Iron supplements, vitamin C, blood transfusions[5] |
| Frequency | 1.48 billion (2015)[6] |
| Deaths | 54,200 (2015)[7] |
Iron-deficiency anemia is defined as a decrease in the number of red blood cells due to a lack of iron in the body.[3][8] Typically, iron deficiency anemia develops over time and can present with symptoms such as feeling tired, weak, short of breath, or having decreased ability to exercise.[1] Anemia that comes on quickly often has greater symptoms, including: confusion, feeling like one is going to pass out, and increased thirst.[1] Anemia is typically significant before a person becomes noticeably pale.[1] Children with iron deficiency anemia may have problems with growth and development .[3] There may be additional symptoms depending on the underlying cause.[1]
Iron-deficiency anemia can be caused by blood loss, insufficient dietary intake, or poor absorption of iron from food.[3] Sources of blood loss can include heavy periods, childbirth, uterine fibroids, stomach ulcers, colon cancer, and urinary tract bleeding.[9] Poor absorption of iron from food may occur as a result of Crohn's disease or a gastric bypass.[9] In the developing world, parasitic worms, malaria, and HIV/AIDS increase the risk of iron deficiency anemia.[10] Diagnosis is generally confirmed by blood tests.[4]
Iron deficiency anemia can be prevented by eating a diet high in iron or by iron supplementation in those at risk.[11] Foods high in iron include meat, eggs, leafy green vegetables and iron-fortified foods such as cereals.[12] Treatment depends on the underlying cause and may include dietary changes, medications, or surgery.[3] Iron supplements and vitamin C may be recommended.[5] Severe cases may be treated with blood transfusions or iron injections.[3]
Iron-deficiency anemia affected about 1.48 billion people in 2015.[6] A lack of dietary iron is estimated to cause approximately half of all anemia cases globally.[13] Women and young children are most commonly affected.[3] In 2015 anemia due to iron deficiency resulted in about 54,000 deaths – down from 213,000 deaths in 1990.[7][14]
Signs and symptoms
Iron deficiency anemia may be present without a person experiencing symptoms.[15] If symptomatic, patients may present with the sign of pallor (reduced oxyhemoglobin in skin or mucous membranes), and the symptoms of fatigue, lightheadedness, and weakness. None of these symptoms (or any of the others below) are sensitive or specific. The symptom most suggestive of iron deficiency anemia in children is pallor of mucous membranes (primarily the conjunctiva). Even so, a large study showed that pallor of the mucous membranes is only 28% sensitive and 87% specific (with high predictive value) in distinguishing children with anemia [hemoglobin (Hb) < 11.0 g/dl] and 49% sensitive and 79% specific in distinguishing severe anemia (Hb < 7.0 g/dl).[16] Thus, this sign is reasonably predictive when present, but not helpful when absent, as only one-third to one-half of children who are anemic (depending on severity) will show pallor.
Iron deficiency anemia tends to develop slowly; therefore the body has time to adapt, and the disease often goes unrecognized for some time.[17] In severe cases, shortness of breath also known as dyspnea can occur.[18] Pica may also develop; of which pagophagia has been suggested to be the most specific for iron deficiency.[17]
Other possible symptoms and signs of iron-deficiency anemia include:[3][17][18][19]

- Irritability
- Angina (chest pain)
- Palpitations (feeling that the heart is skipping beats or fluttering)
- Breathlessness
- Tingling, numbness, or burning sensations
- Glossitis (inflammation or infection of the tongue)
- Angular cheilitis (inflammatory lesions at the mouth's corners)
- Koilonychia (spoon-shaped nails) or nails that are brittle
- Poor appetite
- Dysphagia (difficulty swallowing) due to formation of esophageal webs (Plummer-Vinson syndrome)
- Restless legs syndrome[21]
Child development
Iron-deficiency anemia is associated with poor neurological development, including decreased learning ability and altered motor functions.[22][23] This is because iron deficiency impacts the development of the cells of the brain called neurons. When the body is low on iron, the red blood cells get priority on iron and it is shifted away from the neurons of the brain. Exact causation has not been established, but there is a possible long-term impact from these neurological issues.[23]
Cause
A diagnosis of iron-deficiency anemia requires further investigation into its cause.[24] It can be caused by increased iron demand, increased iron loss, or decreased iron intake.[25] Increased iron demand often occurs during periods of growth, such as in children and pregnant women.[26] For example, during stages of rapid growth, babies and adolescents may outpace dietary intake of iron which can result in deficiency in the absence of disease or a grossly abnormal diet.[25] Iron loss is typically from blood loss. [26] One example of blood loss is by chronic gastrointestinal blood loss, which could be linked to a possible malignancy.[24] In women of childbearing age, heavy menstrual periods can be a source of blood loss and can also cause iron-deficiency anemia.[24] People who do not consume much iron in their diet, such as vegan or vegetarian diets, are at increased risk of developing iron deficiency anemia due to low iron intake.[15]
Parasitic disease
The leading cause of iron-deficiency anemia worldwide is a parasitic disease known as a helminthiasis caused by infestation with parasitic worms (helminths); specifically, hookworms, which include Ancylostoma duodenale, Ancylostoma ceylanicum, and Necator americanus, are most commonly responsible for causing iron-deficiency anemia.[24][27] The World Health Organization estimates that approximately two billion people are infected with soil-transmitted helminths worldwide.[28] Parasitic worms cause both inflammation and chronic blood loss by binding to a human's small-intestinal mucosa, and through their means of feeding and degradation, they can ultimately cause iron-deficiency anemia.[27][17]
Blood loss
Blood contains iron within red blood cells, so blood loss leads to a loss of iron. There are several causes of blood loss including menstrual bleeding, gastrointestinal bleeding, stomach ulcers, and bleeding disorders.[29] The bleeding may occur quickly or slowly. Slow, chronic blood loss within the body — such as from a peptic ulcer, angiodysplasia, inflammatory bowel disease, a colon polyp or gastrointestinal cancer (e.g., colon cancer)— can cause iron-deficiency anemia.
Menstrual bleeding
Menstrual bleeding is a common cause of iron deficiency anemia in women of child bearing age.[29] Women with menorrhagia (heavy menstrual periods) are at risk of iron-deficiency anemia because they are at higher-than-normal risk of losing a larger amount blood during menstruation than is replaced in their diet. Most women lose about 40 mL of blood per cycle. Iron is lost with the blood. Some birth control methods, such as pills and IUDs, may decrease the amount of blood, therefore iron lost during a menstrual cycle.[29]
Gastrointestinal bleeding
The most common cause of iron deficiency anemia in men and post-menopausal women is gastrointestinal bleeding.[29] There are many sources of gastrointestinal tract bleeding including the stomach, esophagus, small intestine, and the large intestine(colon). Gastrointestinal bleeding can result from regular use of some groups of medication, such as NSAIDs (e.g. aspirin), as well as antiplatelets such as clopidogrel and anticoagulants such as warfarin; however, these are required in some patients, especially those with states causing a tendency to form blood clots. In addition, some bleeding disorders can cause gastrointestinal bleeding therefore iron deficiency anemia.[29] Two examples of bleeding disorders are von Willebrand disease and polycythemia vera.[29]
Diet

The body normally gets the iron it requires from foods. If a person consumes too little iron, or iron that is poorly absorbed (non-heme iron), they can become iron deficient over time. Examples of iron-rich foods include meat, eggs, leafy green vegetables and iron-fortified foods. For proper growth and development, infants and children need iron from their diet.[12] For children, a high intake of cow’s milk is associated with an increased risk of iron-deficiency anemia.[30] Other risk factors for iron-deficiency anemia include low meat intake and low intake of iron-fortified products.[30]
The National Academy of Medicine updated Estimated Average Requirements (EARs) and Recommended Dietary Allowances (RDAs) in 2001. The current EAR for iron for women ages 14–18 is 7.9 mg/day, 8.1 for ages 19–50 and 5.0 thereafter (post menopause). For men the EAR is 6.0 mg/day for ages 19 and up. The RDA is 15.0 mg/day for women ages 15–18, 18.0 for 19–50 and 8.0 thereafter. For men, 8.0 mg/day for ages 19 and up. (RDAs are higher than EARs so as to identify amounts that will cover people with higher than average requirements.) The RDA for pregnancy is 27 mg/day, and for lactation, 9 mg/day. For children ages 1–3 years the RDA is 7 mg/day, 10 for ages 4–8 and 8 for ages 9–13.[31] The European Food Safety Authority (EFSA) refers to the collective set of information as Dietary Reference Values, with Population Reference Intakes (PRI) instead of RDAs, and Average Requirements instead of EARs. For women the PRI is 13 mg/day ages 15–17 years, 16 mg/day for women ages 18 and up who are premenopausal and 11 mg/day postmenopausal. For pregnancy and lactation, 16 mg/day. For men the PRI is 11 mg/day ages 15 and older. For children ages 1 to 14 the PRI increases from 7 to 11 mg/day. The PRIs are higher than the US RDAs, with the exception of pregnancy.[32]
Iron malabsorption
Iron from food is absorbed into the bloodstream in the small intestine, primarily in the duodenum.[33] Iron malabsorption is a less common cause of iron-deficiency anemia, but many gastrointestinal disorders can reduce the body's ability to absorb iron.[34] There are different mechanisms that may be present.
In celiac disease, abnormal changes in the structure of the duodenum can decrease iron absorption.[35] Abnormalities or surgical removal of the stomach can also lead to malabsorption by altering the acidic environment needed for iron to be converted into its absorbable form.[34] If there is insufficient production of hydrochloric acid in the stomach, hypochlorhydria/achlorhydria can occur (often due to chronic H. pylori infections or long-term proton pump inhibitor therapy), inhibiting the conversion of ferric iron to the absorbable ferrous iron.[35]
Pregnancy
Without iron supplementation, iron-deficiency anemia occurs in many pregnant women because their iron stores need to serve their own increased blood volume, as well as be a source of hemoglobin for the growing fetus and for placental development.[12]
Other less common causes are intravascular hemolysis and hemoglobinuria.
Iron deficiency in pregnancy appears to cause long-term and irreversible cognitive deficits in the baby.[36]
Babies
Babies are at increased risk of developing iron deficiency anemia due to their rapid growth.[26] Their need for iron is greater than they are getting in their diet.[26] Babies are born with iron stores; however, these iron stores typically run out by 4-6 months of ago. In addition, infants who are given cow's milk too early can develop anemia due to gastrointestinal blood loss.[26]
Children
Children who are at risk for iron-deficiency anemia include:[37]
- Preterm infants
- Low birth weight infants
- Infants fed with cow milk under 12 months of age
- Breastfed infants who have not received iron supplementation after age 6 months, or those receiving non-iron-fortified formulas
- Children between the ages of 1 to 5 years old who receive more than 24 ounces (700 mL) of cow milk per day
- Children with low socioeconomic status
- Children with special health care needs
- Children of Hispanic ethnicity [38]
- Children who are overweight [38]
Blood donors
Frequent blood donors are also at risk for developing iron deficiency anemia.[39] When whole blood is donated, approximately 200mg of iron is also lost from the body.[40] The blood bank screens people for anemia before drawing blood for donation. If the patient has anemia, blood is not drawn.[40] Less iron is lost if the person is donating platelets or white blood cells.[40]
Mechanism
Anemia can result from significant iron deficiency.[34] When the body has sufficient iron to meet its needs (functional iron), the remainder is stored for later use in cells, mostly in the bone marrow and liver.[34] These stores are called ferritin complexes and are part of the human (and other animals) iron metabolism systems. Men store about 3.5g of iron in their body, and women store about 2.5g.[15]
Iron is a mineral that is important in the formation of red blood cells in the body, particularly as a critical component of hemoglobin.[24] About 70% of the iron found in the body is bound to hemoglobin.[15] Iron is primarily absorbed in the small intestine, in particular the duodenum and jejunum. Certain factors increase or decrease absorption of iron. For example, taking Vitamin C with a source of iron is known to increase absorption. Some medications such as tetracyclines and antacids can decrease absorption of iron.[15] After being absorbed in the small intestine, iron travels through blood, bound to transferrin, and eventually ends up in the bone marrow, where it is involved in red blood cell formation.[24] When red blood cells are degraded, the iron is recycled by the body and stored.[24]
When the amount of iron needed by the body exceeds the amount of iron that is readily available, the body can use iron stores (ferritin) for a period of time, and red blood cell formation continues normally.[34] However, as these stores continue to be used, iron is eventually depleted to the point that red blood cell formation is abnormal.[34] Ultimately, anemia ensues, which by definition is a hemoglobin lab value below normal limits.[34][3]
Diagnosis

Conventionally, a definitive diagnosis requires a demonstration of depleted body iron stores obtained by bone marrow aspiration, with the marrow stained for iron.[41][42] However, with the availability of reliable blood tests that can be more readily collected for iron-deficiency anemia diagnosis, a bone marrow aspiration is usually not obtained.[43] Furthermore, a study published April 2009 questions the value of stainable bone marrow iron following parenteral iron therapy.[44] Once iron deficiency anemia is confirmed, gastrointestinal blood loss is presumed to be the cause until proven otherwise since it can be caused by an otherwise asymptomatic colon cancer. Initial evaluation must include esophagogastroduodenoscopy and colonoscopy to evaluate for cancer or bleeding of the gastrointestinal tract.
History
A thorough medical history is important to the diagnosis of iron-deficiency anemia. The history can help to differentiate common causes of the condition such as a menstruation in woman or the presence of blood in the stool.[45] A travel history to areas in which hookworms and whipworms are endemic may also be helpful in guiding certain stool tests for parasites or their eggs.[46]
Although symptoms can play a role in identifying iron-deficiency anemia, they are often vague, which may limit their contribution to determining the diagnosis.
Blood tests
| Change | Parameter |
|---|---|
| ↓ | ferritin, hemoglobin, MCV, MCH |
| ↑ | TIBC, transferrin, RDW, FEP |
Anemia is often discovered by routine blood tests, which generally include a complete blood count (CBC). A sufficiently low hemoglobin (Hb) by definition makes the diagnosis of anemia, and a low hematocrit value is also characteristic of anemia. Further studies will be undertaken to determine the anemia's cause. If the anemia is due to iron deficiency, one of the first abnormal values to be noted on a CBC, as the body's iron stores begin to be depleted, will be a high red blood cell distribution width (RDW), reflecting an increased variability in the size of red blood cells (RBCs).[24][17]
A low mean corpuscular volume (MCV) also appears during the course of body iron depletion. It indicates a high number of abnormally small red blood cells. A low MCV, a low mean corpuscular hemoglobin or mean corpuscular hemoglobin concentration (MCH), and the corresponding appearance of RBCs on visual examination of a peripheral blood smear narrows the problem to a microcytic anemia (literally, a small red blood cell anemia).[17]
The blood smear of a person with iron-deficiency anemia shows many hypochromic (pale, relatively colorless) and small RBCs, and may also show poikilocytosis (variation in shape) and anisocytosis (variation in size).[17][43] Target cells may also be seen. With more severe iron-deficiency anemia, the peripheral blood smear may show hypochromic, pencil-shaped cells and, occasionally, small numbers of nucleated red blood cells.[47] The platelet count may be slightly above the high limit of normal in iron-deficiency anemia (termed a mild thrombocytosis), but severe cases can present with thrombocytopenia (low platelet count).[48]
Iron-deficiency anemia is confirmed by tests that include serum ferritin, serum iron level, serum transferrin, and total iron binding capacity (TIBC). A low serum ferritin is most commonly found. However, serum ferritin can be elevated by any type of chronic inflammation and thus is not consistently decreased in iron-deficiency anemia.[24] Serum iron levels may be measured, but serum iron concentration is not as reliable as the measurement of both serum iron and serum iron-binding protein levels (TIBC).[19] The ratio of serum iron to TIBC (called iron saturation or transferrin saturation index or percent) is a value with defined parameters that can help to confirm the diagnosis of iron-deficiency anemia; however, other conditions must also be considered, including other types of anemia.[19]
Another finding that can be used is the level of free erythrocyte protoporphyrin (FEP).[49] During haemoglobin synthesis, trace amounts of zinc will be incorporated into protoporphyrin in the place of iron which is lacking. We can separate the protoporphyrin from its zinc moeity and measure it, known as the FEP, providing an indirect measurement of the zinc-protoporphyrin complex. The level of FEP is expressed in either μg/dl of whole blood or μg/dl of RBC. An iron insufficiency in the bone marrow can be detected very early by a rise in FEP.
Further testing may be necessary to differentiate iron-deficiency anemia from other disorders, such as thalassemia minor.[50] It is very important not to treat people with thalassemia with an iron supplement, as this can lead to hemochromatosis. A hemoglobin electrophoresis provides useful evidence for distinguishing these two conditions, along with iron studies.[19][51]
Screening
It is unclear if screening pregnant women for iron-deficiency anemia during pregnancy improves outcomes in the United States.[52] The same holds true for screening children who are 6 to 24 months old.[53] Even so, screening is recommended by the US Preventative Services Task Force in pregnant women without symptoms and in infants considered high risk. This is a Level B recommendation. Screening is done with either a hemoglobin or hematocrit lab test.[38]
Treatment

Treatment should take into account the cause and severity of the condition.[5] If the iron-deficiency anemia is a result of blood loss or another underlying cause, treatment is geared toward addressing the underlying cause.[5] Most cases of iron deficiency anemia are treated with oral iron supplements.[54] In severe acute cases, treatment measures are taken for immediate management in the interim, such as blood transfusions or intravenous iron.[5]
Iron-deficiency anemia treatment for less severe cases includes dietary changes to incorporate iron-rich foods into regular oral intake and oral iron supplementation.[5] Foods rich in ascorbic acid (vitamin C) can also be beneficial, since ascorbic acid enhances iron absorption.[5] Oral iron supplements are available in multiple forms. Some are in the form of pills and some are drops for children.[5] Most forms of oral iron replacement therapy are absorbed well by the small intestine; however, there are certain preparations of iron supplements that are designed for longer release in the small intestine than other preparations.[54] Oral iron supplements are best taken up by the body on an empty stomach because food can decrease the amount of iron absorbed from the small intestine.[54] The dosing of oral iron replacement therapy is as much as 200mg per day. This is generally spread out as 3-4 pills taken throughout the day. Each pill containing about 50-65mg of iron.[54] The various forms of treatment are not without possible adverse effects. Iron supplementation by mouth commonly causes negative gastrointestinal effects, including constipation.[55] Constipation is reported by 15-20% of patients taking oral iron therapy.[54] Preparations of iron therapy that take longer to be absorbed by the small intestine(extended release iron therapy) are less likely to cause constipation.[54] It can take up to 6 months to 1 year to get blood levels of iron up to a normal range and provide the body with iron stores.[54]
As iron-deficiency anemia becomes more severe, if the anemia does not respond to oral treatments, or if the treated person does not tolerate oral iron supplementation, then other measures may become necessary.[5][55] Two of these treatment options are parenteral iron and red blood cell transfusion.[54] Parenteral iron is given through an IV.[54] Patients who receive parenteral iron are often those who did not tolerate oral iron or those who require iron on a long term basis.[54] Specifically, patients on dialysis, often get parenteral iron.[55] Individuals on dialysis who are taking forms of erythropoietin or some erythropoiesis-stimulating agent are given parenteral iron, which helps the body respond to the erythropoietin agents and produce red blood cells.[55][56] Intravenous iron can induce an allergic response that can be as serious as anaphylaxis, although different formulations have decreased the likelihood of this adverse effect.[55] In certain cases intravenous iron is both safer and more effective.[57] For patients with severe anemia such as from blood loss, or who have severe symptoms such as cardiovascular instability, a blood transfusion may be considered.[54]
Epidemiology


A moderate degree of iron-deficiency anemia affects approximately 610 million people worldwide or 8.8% of the population.[59] It is slightly more common in females (9.9%) than males (7.8%).[59] Up to 15% of children ages 1-3 years have iron deficiency anemia.[38] Mild iron deficiency anemia affects another 375 million.[59]
The prevalence of iron deficiency as a cause of anemia varies among countries; in the groups in which anemia is most common, including young children and a subset of non-pregnant women, iron deficiency accounts for a fraction of anemia cases in these groups (25% and 37%, respectively).[60] Iron deficiency is a more common cause of anemia in other groups, including pregnant women.[61]
Within the United States, iron-deficiency anemia affects about 2% of adult males, 10.5% of Caucasian women, and 20% of African-American and Mexican-American women.[62]
References
- ^ a b c d e Janz, TG; Johnson, RL; Rubenstein, SD (Nov 2013). "Anemia in the Emergency Department: Evaluation and Treatment". Emergency Medicine Practice. 15 (11): 1–15, quiz 15-6. PMID 24716235.
- ^ "What Are the Signs and Symptoms of Iron-Deficiency Anemia?". NHLBI. 26 March 2014. Archived from the original on 5 July 2017. Retrieved 17 July 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c d e f g h i j "What Is Iron-Deficiency Anemia? - NHLBI, NIH". www.nhlbi.nih.gov. 26 March 2014. Archived from the original on 16 July 2017. Retrieved 17 July 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b "How Is Iron-Deficiency Anemia Diagnosed?". NHLBI. 26 March 2014. Archived from the original on 15 July 2017. Retrieved 17 July 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c d e f g h i "How Is Iron-Deficiency Anemia Treated?". NHLBI. 26 March 2014. Archived from the original on 28 July 2017. Retrieved 17 July 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ a b GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ Stedman's Medical Dictionary (28th ed.). Philadelphia: Lippincott Williams & Wilkins. 2006. p. Anemia. ISBN 9780781733908.
- ^ a b "What Causes Iron-Deficiency Anemia?". NHLBI. 26 March 2014. Archived from the original on 14 July 2017. Retrieved 17 July 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "Micronutrient deficiencies". WHO. Archived from the original on 13 July 2017. Retrieved 17 July 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ "How Can Iron-Deficiency Anemia Be Prevented?". NHLBI. 26 March 2014. Archived from the original on 28 July 2017. Retrieved 17 July 2017.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c "Iron deficiency anemia". Mayo Clinic. March 4, 2011. Archived from the original on November 27, 2012. Retrieved December 11, 2012.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Combs, Gerald F. (2012). The Vitamins. Academic Press. p. 477. ISBN 9780123819802. Archived from the original on 2017-08-18.
{{cite book}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, Regional, and National Age-Sex Specific All-Cause and Cause-Specific Mortality for 240 Causes of Death, 1990-2013: a Systematic Analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
{{cite journal}}:|first1=has generic name (help)CS1 maint: numeric names: authors list (link) - ^ a b c d e Edward T Bope; Rick D Kellerman (2018). Conn's Current Therapy. Philedelphia: Elsevier.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ "Archived copy". Archived from the original on 2012-07-12. Retrieved 2012-05-15.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) Pallor in diagnosis of iron deficiency in children - ^ a b c d e f g Goldman, Lee; Schafer, Andrew (2016). Goldman-Cecil Medicine. pp. 1052–1059, 1068–1073, 2159–2164. ISBN 978-1-4557-5017-7.
- ^ a b Ferri, Fred (2018). Ferri's Clinical Advisor 2018. pp. 87–88, e1–e3713. ISBN 978-0-323-28049-5.
- ^ a b c d McPherson, Richard; Pincus, Matthew (2017). Henry's Clinical Diagnosis and Management by Laboratory Methods. pp. 84–101, 559–605. ISBN 978-0-323-29568-0.
- ^ "koilonychia". Flickr. Retrieved 2018-11-30.
- ^ Rangarajan, Sunad; D'Souza, George Albert. (April 2007). "Restless legs syndrome in Indian patients having iron deficiency anemia in a tertiary care hospital". Sleep Medicine. 8 (3): 247–51. doi:10.1016/j.sleep.2006.10.004. PMID 17368978.
- ^ Kliegman, Robert; Stanton, Bonita; St Geme, Joseph; Schor, Nina (2016). Nelson Textbook of Pediatrics. pp. 2323–2326. ISBN 978-1-4557-7566-8.
- ^ a b Polin, Richard; Ditmar, Mark (2016). Pediatric Secrets. pp. 296–340. ISBN 978-0-323-31030-7.
- ^ a b c d e f g h i Howard, Martin; Hamilton, Peter (2013). Haematology: An Illustrated Colour Text. pp. 24–25. ISBN 978-0-7020-5139-5.
- ^ a b "NPS News 70: Iron deficiency anaemia". NPS Medicines Wise. October 1, 2010. Archived from the original on February 22, 2011. Retrieved November 5, 2010.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c d e M. Tarek Elghetany, Katherine I. Schexneider and Katalin Banki (2017). Henry's Clinical Diagnosis and Management by Laboratory Methods. Elsevier. pp. 559–605.
- ^ a b Broaddus, V. Courtney; Mason, Robert; Ernst, Joel; et al. (2016). Murray and Nadel's Textbook of Respiratory Medicine. pp. 682–698. ISBN 978-1-4557-3383-5.
{{cite book}}: Explicit use of et al. in:|first3=(help) - ^ "Archived copy". Archived from the original on 2014-02-21. Retrieved 2014-03-05.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)CS1 maint: archived copy as title (link) World Health Organization Fact Sheet No. 366, Soil-Transmitted Helminth Infections, updated June 2013 - ^ a b c d e f Ganz T., Kaushansky K, Lichtman MA, Prchal JT, Levi MM, Press OW, Burns LJ, Caligiuri M. Iron Deficiency and Overload in Williams Hematology, 9e. New York, NY: McGraw Hill.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b Decsi, T.; Lohner, S. (2014). "Gaps in meeting nutrient needs in healthy toddlers". Ann Nutr Metab. 65 (1): 22–28. doi:10.1159/000365795. PMID 25227596.
- ^ "Iron". Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Iron (PDF). National Academy Press. 2001. pp. 290–393. ISBN 0-309-07279-4. PMID 25057538.
- ^ "Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies" (PDF). European Food Safety Authority. 2017.
- ^ Yeo, Charles (2013). Shackelford's Surgery of the Alimentary Tract. pp. 821–838. ISBN 978-1-4377-2206-2.
- ^ a b c d e f g Porwit, Anna; McCullough, Jeffrey; Erber, Wendy (2011). Blood and Bone Marrow Pathology. pp. 173–195. ISBN 9780702031472.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b Feldman, Mark; Friedman, Lawrence; Brandt, Lawrence (2016). Sleisenger and Fordtran's Gastrointestinal and Liver Disease. pp. 297–335. ISBN 978-1-4557-4692-7.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Lozoff, Betsy (December 1, 2007). "Iron Deficiency and Child Development". Food and Nutrition Bulletin. 28 (4): S560–S561. doi:10.1177/15648265070284S409. PMID 18297894.
- ^ American Academy of Pediatrics textbook of pediatric care. McInerny, Thomas K.,, American Academy of Pediatrics. (2nd ed.). [Elk Grove Village, IL]. ISBN 9781610020473. OCLC 952123506.
{{cite book}}: CS1 maint: others (link) - ^ a b c d Primack BA, Mahaniah KJ. Anemia. In: South-Paul JE, Matheny SC, Lewis EL. eds. CURRENT Diagnosis & Treatment: Family Medicine, 4e New York, NY: McGraw-Hill; . Accessed November 30, 2018.
- ^ Adamson JW., Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J. Harrison's Principles of Internal Medicine 20e. New York, NY: McGraw-Hill.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b c Ganz T. Iron Deficiency and Overload. In: Kaushansky K, Lichtman MA, Prchal JT, Levi MM, Press OW, Burns LJ, Caligiuri M. eds. Williams Hematology, 9e New York, NY: McGraw-Hill; Accessed December 06, 2018.
- ^ Mazza, J; Barr, RM; McDonald, JW; Valberg, LS (1978). "Usefulness of the serum ferritin concentration in the detection of iron deficiency in a general hospital". Canadian Medical Association Journal. 119 (8): 884–886. PMC 1819106. PMID 737638. Archived from the original on 8 May 2009. Retrieved 2009-05-04.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Kis, AM; Carnes, M (1998). "Detecting Iron Deficiency in Anemic Patients with Concomitant Medical Problems". J Gen Intern Med. 13 (7): 455–61. doi:10.1046/j.1525-1497.1998.00134.x. PMC 1496985. PMID 9686711.
- ^ a b Kellerman, Rick; Bope, Edward (2018). Conn's Current Therapy 2018. pp. 403–405. ISBN 978-0-323-52769-9.
- ^ Thomason, RW; Almiski, MS. (2009). "Evidence That Stainable Bone Marrow Iron Following Parenteral Iron Therapy Does Not Correlate With Serum Iron Studies and May Not Represent Readily Available Storage Iron". American Journal of Clinical Pathology. 131 (4): 580–585. doi:10.1309/AJCPBAY9KRZF8NUC. PMID 19289594. Retrieved 2009-05-04.
- ^ Brady, PG (2007). "Iron deficiency anemia: a call for aggressive diagnostic evaluation". Southern Medical Journal. 100 (10): 966–967. doi:10.1097/SMJ.0b013e3181520699. PMID 17943034. Retrieved July 23, 2012.
- ^ Bennett, J; Dolin, R; Blaser, M (2015). Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, Updated Edition. pp. 3196–3198. ISBN 978-0-323-40161-6.
- ^ Stephen J. McPhee, Maxine A. Papadakis. Current medical diagnosis and treatment 2009 page.428
- ^ Lanzkowsky, Philip; Lipton, Jeffrey; Fish, Jonathan (2016). Lanzkowsky's Manual of Pediatric Hematology and Oncology. pp. 69–83. ISBN 978-0-12-801368-7.
- ^ Joint World Health Organization/Centers for Disease Control and Prevention Technical Consultation on the Assessment of Iron Status at the Population Level (2004 : Geneva, Switzerland). (2007). Assessing the iron status of populations: including literature reviews: report of a Joint World Health Organization/Centers for Disease Control and Prevention Technical Consultation on the Assessment of Iron Status at the Population Level, Geneva, Switzerland, 6–8 April 2004, 2nd ed. World Health Organization. http://www.who.int/iris/handle/10665/75368
- ^ O'Connell, Theodore (2017). Instant Work-ups: A Clinical Guide to Medicine. pp. 23–31. ISBN 978-0-323-37641-9.
- ^ Hines, Roberta; Marschall, Katherine (2018). Stoelting's Anesthesia and Co-existing Disease. pp. 477–506. ISBN 978-0-323-40137-1.
- ^ Siu, AL; U.S. Preventive Services Task, Force (6 October 2015). "Screening for Iron Deficiency Anemia and Iron Supplementation in Pregnant Women to Improve Maternal Health and Birth Outcomes: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. 163 (7): 529–36. doi:10.7326/m15-1707. PMID 26344176.
- ^ Siu, Albert L. (2015-10-01). "Screening for Iron Deficiency Anemia in Young Children: USPSTF Recommendation Statement". Pediatrics. 136 (4): 746–752. doi:10.1542/peds.2015-2567. ISSN 0031-4005. PMID 26347426.
- ^ a b c d e f g h i j k Adamson JW. Iron Deficiency and Other Hypoproliferative Anemias. In: Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J. eds. Harrison's Principles of Internal Medicine, 19e' New York, NY: McGraw-Hill; 2014.
- ^ a b c d e Kasper, Dennis; Fauci, Anthony; Hauser, Stephen; Longo, Dan; Jameson, J. Larry; Loscalzo, Joseph, Dennis; Fauci, Anthony; Hauser, Stephen; Longo, Dan; Jameson, J. Larry; Loscalzo, Joseph (2015). "126". Harrison's Principles of Internal Medicine, 19e. ISBN 978-0-07-180215-4.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ "KDIGO clinical practice guideline for anemia in chronic kidney disease". Agency for Healthcare Research and Quality. August 2012.
{{cite web}}: Cite has empty unknown parameter:|dead-url=(help) - ^ Auerbach, M; Deloughery, T (2 December 2016). "Single-dose intravenous iron for iron deficiency: a new paradigm". Hematology. American Society of Hematology. Education Program. 2016 (1): 57–66. doi:10.1182/asheducation-2016.1.57. PMID 27913463.
- ^ "Mortality and Burden of Disease Estimates for WHO Member States in 2002". World Health Organization. 2002. Archived from the original (xls) on 2013-01-16.
{{cite web}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c Vos, T; Flaxman, AD; Naghavi, M; Lozano, R; Michaud, C; Ezzati, M; Shibuya, K; Salomon, JA; et al. (Dec 15, 2012). "Years Lived with Disability (YLDs) for 1160 Sequelae of 289 Diseases and Injuries 1990-2010: a Systematic Analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ^ Petry, Nicolai; Olofin, Ibironke; Hurrell, Richard F.; Boy, Erick; Wirth, James P.; Moursi, Mourad; Donahue Angel, Moira; Rohner, Fabian (2016-11-02). "The Proportion of Anemia Associated with Iron Deficiency in Low, Medium, and High Human Development Index Countries: A Systematic Analysis of National Surveys". Nutrients. 8 (11): 693. doi:10.3390/nu8110693.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Sifakis, S.; Pharmakides, G. (2000-04-01). "Anemia in Pregnancy". Annals of the New York Academy of Sciences. 900 (1): 125–136. doi:10.1111/j.1749-6632.2000.tb06223.x. ISSN 1749-6632.
- ^ Killip, S; Bennett, JM; Chambers, MD (1 March 2007). "Iron deficiency anemia". American Family Physician. 75 (5): 671–8. PMID 17375513. Archived from the original on 11 March 2016.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help)
External links
- The Importance of Iron – From IronTherapy.Org
- Interactive material on Iron Metabolism – From IronAtlas.com
- Establishing the cause of anemia – From AnaemiaWorld.com
- Handout: Iron Deficiency Anemia – From the National Anemia Action Council
- NPS News 70: Iron deficiency anaemia: NPS – Better choices, Better health – From the National Prescribing Service
