Fetus
A fetus (or foetus or fœtus) is a developing mammal or other viviparous vertebrate, after the embryonic stage and before birth. The plural is fetuses, or sometimes feti.
In humans, the fetal stage of prenatal development begins about eight weeks after fertilization, when the major structures and organ systems have formed,[2] until birth.[3]
Etymology and spelling variations
The word fetus is from the Latin fetus, meaning offspring, bringing forth, hatching of young.[4] It has Indo-European roots related to sucking or suckling.[5]
Fœtus is an English variation on the Latin spelling, and has been in use since at least 1594, according to the Oxford English Dictionary, which describes "fœtus" as "incorrectly written". The variant fœtus may have originated with an error by Saint Isidore of Seville, in AD 620.[6] The preferred spelling in the United States is fetus, but the variants foetus and fœtus persist in other English-speaking countries and in some medical contexts, as well as in some other languages (e.g., French). heLLO JENg JENG (ALDAINE)
Human fetus

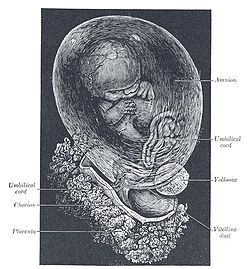
The fetal stage begins about eight weeks after fertilization. The fetus is not as sensitive to damage from environmental exposures as the embryo was, though toxic exposures can often cause physiological abnormalities or minor congenital malformation.[7] Fetal growth can be terminated by various factors, including miscarriage, feticide committed by a third party, or induced abortion. Throughout the fetal stage, the fetus continues to be connected to the placenta by the umbilical cord, which supplies the fetus with oxygenated, nutrient-rich blood from the placenta, and conversely returns the deoxygenated, nutrient-depleted blood to the placenta. The fetus is surrounded by amniotic fluid, which (among other things) cushions against blows to the mother's abdomen, allows for easier fetal movement, promotes muscular/skeletal development, and helps protect the fetus from heat loss.
Development
The following timeline describes some of the specific changes in fetal anatomy and physiology by fertilization age (i.e. the time elapsed since fertilization). Obstetricians often find it convenient to instead measure gestational age from two weeks earlier than fertilization, but the term “gestational age” is often ambiguous, and there is no uniform method for counting it.[8] Embryologists typically measure age from fertilization.[9] For purposes of this article, age is measured from fertilization, except as noted.
8 weeks: condition at start of fetal stage

The risk of miscarriage decreases sharply at the beginning of the fetal stage, and loss is "virtually complete by the end of the embryonic period."[11][12] At this point, all major structures, including hands, feet, head, brain, and other organs are present, but they will continue to grow, develop, and become more functional.[13] When the fetal stage commences, a fetus is typically about 30 mm (1.2 inches) in length from crown to rump, and weighs about 8 grams.[14] The heart is beating.[15] The fingers and toes have separated from each other,[16] and some fingerprint formation can be seen from the beginning of the fetal stage.[17][18] By the fetal stage, the embryonic tail is gone, and an atrophied embryonic tail bud remains.[19][20]
The first movements occur around this time, and those movements include sideward bendings of the head.[21] Generally speaking, fetal movement can be classified as either elicited (e.g. reflexive) or spontaneous, and spontaneous movements may be triggered by either the spine or the brain. Whether a spontaneous movement is supraspinally determined (i.e. caused by signals from the brain) can be inferred by comparison to movements of an anencephalic fetus, which has no brain.[22]
8 to 15 weeks after fertilization
The fetus makes general movements and startles from about nine weeks.[21] Movements include complex motor patterns, and localized movement of the arms and legs, together with hiccups, stretches and yawns.[21][23] The breathing-like movement of the fetus is necessary for stimulation of lung development, rather than for obtaining oxygen.[24]
At nine weeks the fetus is able to bend fingers around an object; in response to a touch on the foot, the fetus bends the legs or curls the toes to move away from an object.[25] During weeks 9-12, the face is “well-formed” and the fetus is three to six inches in length.[26] From weeks 9 to 12, the head makes up nearly half of the fetus' size, the fetal eyelids close and remain closed for several months, and the appearance of the genitals in males and females becomes more apparent.[26] The fetus begins drinking amniotic fluid about twelve weeks after fertilization,[27] for hydration and nutrition.[28] Tooth buds appear, the limbs are long and thin, and red blood cells are produced in the liver, however the majority of red blood cells will be made later in gestation (at 21 weeks) by bone marrow.[26] A fine hair called lanugo develops on the head. The gastrointestinal tract, still forming, starts to collect sloughed skin and lanugo, as well as hepatic products, forming meconium (stool). [26] Fetal skin is almost transparent. More muscle tissue and bones have developed, and the bones become harder. The first measurable signs of EEG movement occur in the 12th week.[29] By the end of this stage, the fetus has reached about 15 cm (6 inches).
16 to 25 weeks after fertilization
The lanugo covers the entire body. Eyebrows, eyelashes, fingernails, and toenails appear. The fetus has increased muscle development. Alveoli (air sacs) are forming in lungs. The nervous system develops enough to control some body functions. The cochlea are now developed, though the myelin sheaths in the neural portion of the auditory system will continue to develop until 18 months after birth. The respiratory system has developed to the point where gas exchange is possible. The quickening, which refers to the first maternally discernable fetal movements, are often felt during this period, although the fetus has been moving throughout the fetal stage. A woman pregnant for the first time (i.e. a primiparous woman) typically feels fetal movements at about 18-19 weeks, whereas a woman who has already given birth at least two times (i.e. a multiparous woman) will typically feel movements around 16 weeks.[30] By the end of the fifth month, the fetus is about 20 cm (8 inches).
26 to 38 weeks after fertilization

The amount of body fat rapidly increases. Lungs are not fully mature. Thalamic brain connections, which mediate sensory input, form. Bones are fully developed, but are still soft and pliable. Iron, calcium, and phosphorus become more abundant. Fingernails reach the end of the fingertips. The lanugo begins to disappear, until it is gone except on the upper arms and shoulders. Small breast buds are present on both sexes. Head hair becomes coarse and thicker. Birth is imminent and occurs around the 38th week. The fetus is considered full-term between weeks 35 and 40,[31] which means that the fetus is considered sufficiently developed for life outside the uterus.[32] It may be 48 to 53 cm (19 to 21 inches) in length, when born. Control of movement is limited at birth, and purposeful voluntary movements develop all the way until puberty.[33][34]
Variation in growth
There is much variation in the growth of the fetus. When fetal size is less than expected, that condition is known as intrauterine growth restriction (IUGR) also called fetal growth restriction (FGR); factors affecting fetal growth can be maternal, placental, or fetal.[35]
Maternal factors include maternal weight, body mass index, nutritional state, emotional stress, toxin exposure (including tobacco, alcohol, heroin, and other drugs which can also harm the fetus in other ways), and uterine blood flow.
Placental factors include size, microstructure (densities and architecture), umbilical blood flow, transporters and binding proteins, nutrient utilization and nutrient production.
Fetal factors include the fetus genome, nutrient production, and hormone output. Also, female fetuses tend to weigh less than males, at full term.[35]
Fetal growth is often classified as follows: small for gestational age (SGA), appropriate for gestational age (AGA), and large for gestational age (LGA).[36] SGA can result in low birth weight, although premature birth can also result in low birth weight. Low birth weight increases risk for perinatal mortality (death shortly after birth), asphyxia, hypothermia, polycythemia, hypocalcemia, immune dysfunction, neurologic abnormalities, and other long-term health problems. SGA may be associated with growth delay, or it may instead be associated with absolute stunting of growth.
Viability

The lower limit of viability is approximately five months gestational age, and usually later.[37] According to The Developing Human:
Viability is defined as the ability of fetuses to survive in the extrauterine environment... There is no sharp limit of development, age, or weight at which a fetus automatically becomes viable or beyond which survival is assured, but experience has shown that it is rare for a baby to survive whose weight is less than 500 gm or whose fertilization age is less than 22 weeks. Even fetuses born between 26 and 28 weeks have difficulty surviving, mainly because the respiratory system and the central nervous system are not completely differentiated... If given expert postnatal care, some fetuses weighing less than 500 gm may survive; they are referred to as extremely low birth weight or immature infants.... Prematurity is one of the most common causes of morbidity and prenatal death.[38]
During the past several decades, neonatal care has improved with advances in medical science, and therefore the limit of viability has have moved earlier.[39] As of 2006, the two youngest children to survive premature birth are thought to be James Elgin Gill (born on 20 May 1987 in Ottawa, Canada, at 21 weeks and 5 days gestational age),[40][41] and Amillia Taylor (born on 24 October 2006 in Miami, Florida, at 21 weeks and 6 days gestational age).[42][43] Both children were born just under 20 weeks from fertilization, or a few days past the midpoint of an average full-term pregnancy. Despite their premature births, both developed into healthy children.
Fetal pain
The subject of fetal pain and suffering is controversial. There may be an "emerging consensus among developmental neurobiologists that the establishment of thalamocortical connections" (at about 26 weeks) is a critical event with regard to fetal perception of pain.[44] Nevertheless, because pain can involve sensory, emotional and cognitive factors, it is "impossible to know" when painful experiences may become possible, even if it is known when thalamocortical connections are established.[44] Some experts have asserted that a fetus can sense pain as early as 13 ½ weeks.[45] In summary, there is good evidence that from about 26 weeks gestation the fetal brain can be considered a functional unit capable of processing noxious sensory input,[44] and pain before that point may also be possible.[46] The science of fetal pain is not completely certain, and the nature of pain remains elusive.[47]
Whether a fetus has the ability to feel pain and to suffer is part of the abortion debate.[48] [49] For example, in the United States, legislation has been proposed by pro-life advocates requiring abortion providers to tell a woman that the fetus may feel pain during the abortion procedure, and that require her to accept or decline anesthesia for the fetus.[50]
Circulatory system

The circulatory system of a human fetus works differently from that of born humans, mainly because the lungs are not in use: the fetus obtains oxygen and nutrients from the woman through the placenta and the umbilical cord.[51]
Blood from the placenta is carried to the fetus by the umbilical vein. About half of this enters the fetal ductus venosus and is carried to the inferior vena cava, while the other half enters the liver proper from the inferior border of the liver. The branch of the umbilical vein that supplies the right lobe of the liver first joins with the portal vein. The blood then moves to the right atrium of the heart. In the fetus, there is an opening between the right and left atrium (the foramen ovale), and most of the blood flows from the right into the left atrium, thus bypassing pulmonary circulation. The majority of blood flow is into the left ventricle from where it is pumped through the aorta into the body. Some of the blood moves from the aorta through the internal iliac arteries to the umbilical arteries, and re-enters the placenta, where carbon dioxide and other waste products from the fetus are taken up and enter the woman's circulation.[51]
Some of the blood from the right atrium does not enter the left atrium, but enters the right ventricle and is pumped into the pulmonary artery. In the fetus, there is a special connection between the pulmonary artery and the aorta, called the ductus arteriosus, which directs most of this blood away from the lungs (which aren't being used for respiration at this point as the fetus is suspended in amniotic fluid).[51]
Postnatal development
With the first breath after birth, the system changes suddenly. The pulmonary resistance is dramatically reduced ("pulmo" is from the Latin for "lung"). More blood moves from the right atrium to the right ventricle and into the pulmonary arteries, and less flows through the foramen ovale to the left atrium. The blood from the lungs travels through the pulmonary veins to the left atrium, increasing the pressure there. The decreased right atrial pressure and the increased left atrial pressure pushes the septum primum against the septum secundum, closing the foramen ovale, which now becomes the fossa ovalis. This completes the separation of the circulatory system into two halves, the left and the right.
The ductus arteriosus normally closes off within one or two days of birth, leaving behind the ligamentum arteriosum. The umbilical vein and the ductus venosus closes off within two to five days after birth, leaving behind the ligamentum teres and the ligamentum venosus of the liver respectively.
Differences from the adult circulatory system
Remnants of the fetal circulation can be found in adults:[52][53]
| Fetal | Adult |
|---|---|
| foramen ovale | fossa ovalis |
| ductus arteriosus | ligamentum arteriosum |
| extra-hepatic portion of the fetal left umbilical vein | ligamentum teres hepatis (the "round ligament of the liver"). |
| intra-hepatic portion of the fetal left umbilical vein (the ductus venosus) | ligamentum venosum |
| proximal portions of the fetal left and right umbilical arteries | umbilical branches of the internal iliac arteries |
| distal portions of the fetal left and right umbilical arteries | medial umbilical ligaments (urachus) |
In addition to differences in circulation, the developing fetus also employs a different type of oxygen transport molecule than adults (adults use adult hemoglobin). Fetal hemoglobin enhances the fetus' ability to draw oxygen from the placenta. Its association curve to oxygen is shifted to the left, meaning that it will take up oxygen at a lower concentration than adult hemoglobin will. This enables fetal hemoglobin to absorb oxygen from adult hemoglobin in the placenta, which has a lower pressure of oxygen than at the lungs.
-
3D ultrasound of 3-inch fetus (about 14 weeks gestational age)
-
Fetus at 17 weeks
-
Fetus at 20 weeks
Developmental problems
Congenital anomalies are anomalies that are acquired before birth. Infants with certain congenital anomalies of the heart can survive only as long as the ductus remains open: in such cases the closure of the ductus can be delayed by the administration of prostaglandins to permit sufficient time for the surgical correction of the anomalies. Conversely, in cases of patent ductus arteriosus, where the ductus does not properly close, drugs that inhibit prostaglandin synthesis can be used to encourage its closure, so that surgery can be avoided.
A developing fetus is highly susceptible to anomalies in its growth and metabolism, increasing the risk of birth defects. One area of concern is the pregnant woman's lifestyle choices made during pregnancy [54] Diet is especially important in the early stages of development. Studies show that supplementation of the woman's diet with folic acid reduces the risk of spina bifida and other neural tube defects. Another dietary concern is whether the woman eats breakfast. Skipping breakfast could lead to extended periods of lower than normal nutrients in the woman's blood, leading to a higher risk of prematurity, or other birth defects in the fetus. During this time alcohol consumption may increase the risk of the development of Fetal alcohol syndrome, a condition leading to mental retardation in some infants.[55] Smoking during pregnancy may also lead to reduced birth weight. Low birth weight is defined as 2500 grams (5.5 lb). Low birth weight is a concern for medical providers due to the tendency of these infants, described as premature by weight, to have a higher risk of secondary medical problems.
Legal issues
In the United States, some states have laws that impose strict punishments for those who inflict violence that results in damage to a fetus or the unwanted termination of a pregnancy. The severity of the punishment, and the stage of fetal development where laws start to apply vary from state to state.[56]
Abortion of a fetus is legal in many countries such as Australia, Canada, the United Kingdon, and the United States. Many of those countries that allow abortion during the fetal stage have gestational time limits, so that late-term abortions are not normally allowed.[57]
Non-human fetuses


Any developing mammal or other viviparous vertebrate will pass through a fetal stage after the embryonic stage and before birth. The fetuses of most mammals are situated similarly to the homo sapiens fetus within their mothers.[58] However, the anatomy of the area surrounding a fetus is different in litter-bearing animals compared to humans: each fetus of a litter-bearing animal is surrounded by placental tissue and is lodged along one of two long uteri instead of the single uterus found in a human female.
Development at birth varies considerably among animals, and even among mammals. Altricial species are relatively helpless at birth and require considerable parental care and protection. In contrast, precocial animals are born with open eyes, have hair or down, have large brains, and are immediately mobile and somewhat able to flee from, or defend themselves against, predators. Primates are precocial at birth, with the exception of humans.[59]
The duration of gestation in placental mammals (i.e. mammals other than monotremes and marsupials) varies from 18 days in jumping mice to 23 months in elephants.[60] Generally speaking, fetuses of larger land mammals require longer gestation periods.[60]
See also
- Pregnancy (human)
- Child
- Superfetation
- Neural development
- Fetoscopy
- Fetal position
- Fetal rights
- Women's rights
References
- ^ Gray, Henry and Lewis, Warren. Anatomy of the Human Body, page 57 (Lea and Febiger 1918). Via Google Books. Retrieved (2009-02-03).
- ^ MedicineNet.com. See also Dictionary.com.
- ^ Some authorities suggest that the embryonic stage may last only seven weeks. See Encyclopedia Britannica: "In humans, the organism is called an embryo for the first seven or eight weeks after conception, after which it is called a fetus." Also see The Columbia Encyclopedia (Sixth Edition). Retrieved 2007-03-05: "the fetal stage begins seven to eight weeks after fertilization of the egg, when the embryo assumes the basic shape of the newborn and all the organs are present."
- ^ Harper, Douglas. (2001). Online Etymology Dictionary. Retrieved 2007-01-20.
- ^ The American Heritage Dictionary of the English Language, Fourth Edition. Retrieved 2007-01-22.
- ^ Aronson, Jeff (1997). "When I use a word...:Oe no!". British Medical Journal. 315 (1). BMJ Publishing Group Ltd. Retrieved 2006-06-29.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Drews, Ulrich. Color Atlas of Embryology, page 360 (Thieme 1995).
- ^ ’’'Dorland's Medical Dictionary.’’ Also see "Mini-Review: Prenatal ages and stages - measures and errors," Teratology, Volume 61 Issue 5, Pages 382-384 (2000). Also see Rahman, Anika et al. “A Global Review of Laws on Induced Abortion”, 1985-1997, International Family Planning Perspectives, volume 24 (1998).
- ^ Segen, J.C. The Dictionary of Modern Medicine, page 187: "obstetricians calculate gestational age; embryologists are more correct as they calculate the ovulation or fertilization age." Also see Dudek, Ronald et al. Embryology. Also see Drews, Ulrich. Color Atlas of Embryology.
- ^ Marc H. Bornstein, Michael E. Lamb. Developmental Science: An Advanced Textbook, page 227 (2005): “At 8 weeks, fetuses measure 3.18 cm from crown to rump (1.25 inches).”
- ^ Rodeck, Charles; Whittle, Martin. Fetal Medicine: Basic Science and Clinical Practice (Elsevier Health Sciences 1999), page 835.
- ^ • Q&A: Miscarriage. (August 6 , 2002). BBC News. Retrieved 2007-04-22: “The risk of miscarriage lessens as the pregnancy progresses. It decreases dramatically after the 8th week.”
• Lennart Nilsson, A Child is Born 91 (1990): at eight weeks, "the danger of a miscarriage … diminishes sharply."
• “Women’s Health Information”, Hearthstone Communications Limited: “The risk of miscarriage decreases dramatically after the 8th week as the weeks go by.” Retrieved 2007-04-22. - ^ The Columbia Encyclopedia (Sixth Edition). Retrieved 2007-03-05.
- ^ Klossner, N. Jayne Introductory Maternity Nursing (2005): "The fetal stage is from the beginning of the 9th week after fertilization and continues until birth"
- ^ Greenfield, Marjorie. “Dr. Spock.com". Retrieved 2007-01-20.
- ^ Rana, M. and Rana Abdul. Human Embryology Made Easy, page 101 (CRC Press, 1998).
- ^ Mathew, L. et al. “Dermatoglyphic peculiarities in children with oral clefts,” Journal of Indian Society of Pedodontics and Preventive Dentistry, Volume 23, pages 179-182 (2005): “finger and palm prints are formed during the first 6-7 weeks of the embryonic period and are completed after 10-20 weeks of gestation.”
- ^ Zabinski, Mark. Forensic Series Seminar, Pastore Chemical Laboratory, University of Rhode Island (February 2003) (news report retrieved 2007-01-20).
- ^ "Fetal development: What happens during the first trimester?" Mayo Clinic.
- ^ “9.1 Developmental stages” (online course in embryology for medicine students developed by the universities of Fribourg, Lausanne and Bern with the support of the Swiss Virtual Campus).
- ^ a b c Prechtl, Heinz. "Prenatal and Early Postnatal Development of Human Motor Behavior" in Handbook of brain and behaviour in human development, Kalverboer and Gramsbergen eds., pp. 415-418 (2001 Kluwer Academic Publishers): "The first movements to occur are sideward bendings of the head....At 9-10 weeks postmestrual age complex and generalized movements occur. These are the so-called general movements (Prechtl et al., 1979) and the startles. Both include the whole body, but the general movements are slower and have a complex sequence of involved body parts, while the startle is a quick, phasic movement of all limbs and trunk and neck."
- ^ De Vries, Johanna et al. “Fetal Motility in the First Half of Pregnancy”, in Continuity of Neural Functions from Prenatal to Postnatal Life, pages 4 and 63 (1984 Cambridge University Press, edited by Heinz F. R. Prechtl).
- ^ Butterworth, George and Harris, Margaret. Principles of developmental psychology (Psychology Press 1994).
- ^ Institute of Medicine of the National Academies, Preterm Birth: Causes, Consequences, and Prevention (2006). Retrieved 2007-03-04.
- ^ Valman, H. and Pearson, J. "What the Fetus Feels", British Medical Journal, (January 26, 1980). Retrieved 2007-03-04.
- ^ a b c d Medline Plus Medical Encyclopedia
- ^ Motor Development in Children: Postgraduate Course of the Pierfranco E Luisa Mariani Foundation, Milan State University, 10-12 March 1993.
- ^ Jones, Sandy et al. Great Expectations, page 69 (Sterling Publishing 2004).
- ^ Vogel, Friedrich. Genetics and the Electroencephalogram (Springer 2000): "Slow EEG activity (0.5 – 2 c/s) can be demonstrated in the fetus even at the conceptual age of three months." Retrieved 2007-03-05.
- ^ Levene, Malcolm et al. Essentials of Neonatal Medicine (Blackwell 2000), page 8. Retrieved 2007-03-04.
- ^ Your Pregnancy: 36 Weeks BabyCenter.com Retrieved June 1, 2007.
- ^ "full-term" defined by Memidex/WordNet.
- ^ Stanley, Fiona et al. "Cerebral Palsies: Epidemiology and Causal Pathways", page 48 (2000 Cambridge University Press): "Motor competance at birth is limited in the human neonate. The voluntary control of movement develops and matures during a prolonged period up to puberty...."
- ^ Becher, Julie-Claire. "Insights into Early Fetal Development", Behind the Medical Headlines (Royal College of Physicians of Edinburgh and Royal College of Physicians and Surgeons of Glasgow October 2004)
- ^ a b Holden, Chris and MacDonald, Anita. Nutrition and Child Health (Elsevier 2000). Retrieved 2007-03-04.
- ^ Queenan, John. Management of High-Risk Pregnancy (Blackwell 1999). Retrieved 2007-03-04.
- ^ Halamek, Louis. "Prenatal Consultation at the Limits of Viability", NeoReviews, Vol.4 No.6 (2003): "most neonatologists would agree that survival of infants younger than approximately 22 to 23 weeks’ estimated gestational age [i.e. 20 to 21 weeks' estimated fertilization age] is universally dismal and that resuscitative efforts should not be undertaken when a neonate is born at this point in pregnancy."
- ^ Moore, Keith and Persaud, T. The Developing Human: Clinically Oriented Embryology, page 103 (Saunders 2003).
- ^ Roe v. Wade, 410 U.S. 113 (1973) ("viability is usually placed at about seven months (28 weeks) but may occur earlier, even at 24 weeks.") Retrieved 2007-03-04.
- ^ "Powell's Books - Guinness World Records 2004 (Guinness Book of Records) by". Retrieved 2007-11-28.
- ^ "Miracle child". Retrieved 2007-11-28.
- ^ "Most-premature baby allowed home". BBC News. 2007-02-21. Retrieved 2007-05-05.
{{cite news}}: Check date values in:|date=(help) - ^ Baptist Hospital of Miami, Fact Sheet (2006).
- ^ a b c Johnson, Martin and Everitt, Barry. Essential reproduction (Blackwell 2000): "The multidimensionality of pain perception, involving sensory, emotional, and cognitive factors may in itself be the basis of conscious, painful experience, but it will remain difficult to attribute this to a fetus at any particular developmental age." Retrieved 2007-02-21.
- ^ Collins, Vincent et al."Fetal Pain and Abortion: the Medical Evidence", Studies in Law and Medicine, No 18 (1984): "because the requisite neurological structures are present at that time and because they are functioning, as evidenced by the aversive response of the human fetus, it may be concluded with reasonable medical certainty that the fetus can sense pain at least by 13 ½ weeks."
- ^ Lee, Susan J., Ralston, Henry J. Peter, Drey, Eleanor A., Partridge, John Colin, & Rosen, Mark A. (2005). "Fetal Pain: A Systematic Multidisciplinary Review of the Evidence", Journal of the American Medical Association, 294 (8), 947-954. Retrieved 2007-02-26: "Evidence regarding the capacity for fetal pain is limited but indicates that fetal perception of pain is unlikely before the third trimester .... electroecephalography suggests the capacity for functional pain perception in preterm neonates does not exist before 29 or 30 weeks .... Pain is an emotional and psychological experience that requires conscious recognotion of a noxious stimulus." Two authors of the 2005 study published in JAMA did not report their abortion-related activities, which pro-life groups called a conflict of interest; the editor of JAMA responded that JAMA probably would have mentioned those activities if they had been disclosed, but still would have published the study. See Denise Grady, “Study Authors Didn't Report Abortion Ties”, New York Times (2005-08-26). The study published in JAMA has also been criticized on scientific grounds. See Anand, K. "A Scientific Appraisal of Fetal Pain and Conscious Sensory Perception", written testimony to Congress (2005). Retrieved 2007-03-10.
- ^ See “Science, politics and fetal pain; Abortion issue muddies real debate on fetal pain perception”, About Kids Health, The Hospital for Sick Children (2006-05-18), via Archive.org: "Although there is a political and moral component to this particular debate, questions about the nature of pain, pain perception and the mechanism of pain have been ongoing for years. For example, it was once widely believed that infants do not experience pain, a belief now shown to be incorrect. At the same time, allodynia, a condition in which even a gentle touch becomes painful, and congenital insensitivity to pain, or an inability to feel pain under any circumstance including injury, illustrate the bizarre and still-elusive nature of pain."
- ^ White, R. Frank. "Are We Overlooking Fetal Pain and Suffering During Abortion?", American Society of Anesthesiologists Newsletter (October 2001). Retrieved 2007-03-10.
- ^ David, Barry & and Goldberg, Barth. "Recovering Damages for Fetal Pain and Suffering", Illinois Bar Journal (December 2002). Retrieved 2007-03-10.
- ^ Weisman, Jonathan. "House to Consider Abortion Anesthesia Bill", Washington Post 2006-12-05. Retrieved 2007-02-06.
- ^ a b c Whitaker, Kent. Comprehensive Perinatal and Pediatric Respiratory Care (Delmar 2001). Retrieved 2007-03-04.
- ^ Dudek, Ronald and Fix, James. Board Review Series Embryology (Lippincott 2004). Retrieved 2007-03-04.
- ^ University of Michigan Medical School, Fetal Circulation and Changes at Birth. Retrieved 2007-03-04.
- ^ Dalby, JT. (1978).Environmental effects on prenatal development Journal of Pediatric Psychology, 3, 105-109.
- ^ Streissguth, A. (1997). Fetal Alcohol Syndrome: A Guide for Families and Communities. Baltimore: Brookes Publishing. ISBN 1-55766-283-5.
- ^ National Conference of State Legislatures. (June 2006). "Fetal Homicide". Retrieved January 19 2007.
- ^ Anika Rahman, Laura Katzive and Stanley K. Henshaw. A Global Review of Laws on Induced Abortion, 1985-1997, International Family Planning Perspectives (Volume 24, Number 2, June 1998).
- ^ ZFIN, Pharyngula Period (24-48 h). Modified from: Kimmel et al., 1995. Developmental Dynamics 203:253-310. Downloaded 5 March 2007.
- ^ Lewin, Roger. Human Evolution, page 78 (Blackwell 2004).
- ^ a b Sumich, James and Dudley, Gordon. Laboratory and Field Investigations in Marine Life, page 320 (Jones & Bartlett 2008).
External links
- "Prenatal Image Gallery Index" from The Endowment for Human Development (providing numerous motion pictures of human fetal movement that can be viewed online).
- "In the Womb," video from National Geographic.



