Guillain–Barré syndrome
| Guillain–Barré syndrome | |
|---|---|
| Specialty | Neurology |
Guillain–Barré syndrome (GBS) (French pronunciation: [ɡiˈlɛ̃ baˈʁe], English: /ˈɡiːlænˈbɑːreɪ/), sometimes Landry's paralysis or Guillain–Barré–Strohl syndrome, is an acute polyneuropathy, a disorder affecting the peripheral nervous system. Ascending paralysis, weakness beginning in the feet and hands and migrating towards the trunk, is the most typical symptom, and some subtypes cause change in sensation or pain, as well as dysfunction of the autonomic nervous system. It can cause life-threatening complications, in particular if the respiratory muscles are affected or if the autonomic nervous system is involved. The disease is usually triggered by an infection.
The diagnosis is usually made by nerve conduction studies and with studies of the cerebrospinal fluid. With prompt treatment by intravenous immunoglobulins or plasmapheresis, together with supportive care, the majority will recover completely. Guillain–Barré syndrome is rare, at one to two cases per 100,000 people annually, but is the most common cause of acute non-trauma-related paralysis. The syndrome is named after the French physicians Georges Guillain and Jean Alexandre Barré, who described it in 1916.
Classification
Six different subtypes of Guillain–Barré syndrome exist:[citation needed]
- Acute inflammatory demyelinating polyneuropathy (AIDP) is the most common form of GBS, and the term is often used synonymously with GBS. It is caused by an autoimmune response directed against Schwann cell membranes.
- Miller Fisher syndrome (MFS) is a rare variant of GBS. Accounting for about 5% of GBS cases, it manifests as a descending paralysis, proceeding in the reverse order of the more common form of GBS.[1] It usually affects the eye muscles first and presents with the triad of ophthalmoplegia, ataxia, and areflexia.[2] The ataxia predominantly affects the gait and trunk, with the limbs relatively spared. Anti-GQ1b antibodies are present in 90% of cases.
- Acute motor axonal neuropathy (AMAN),[3] also known as Chinese paralytic syndrome, attacks motor nodes of Ranvier and is prevalent in China and Mexico. It is probably due to an auto-immune response directed against the axoplasm of peripheral nerves. The disease may be seasonal and recovery can be rapid. Anti-GD1a antibodies[4] are present. Anti-GD3 antibodies are found more frequently in AMAN.
- Acute motor sensory axonal neuropathy (AMSAN) is similar to AMAN, but also affects sensory nerves with severe axonal damage. Like AMAN, it is probably due to an autoimmune response directed against the axoplasm of peripheral nerves. Recovery is slow and often incomplete.[5]
- Acute panautonomic neuropathy is the rarest variant of GBS, sometimes accompanied by encephalopathy. It is associated with a high mortality rate, owing to cardiovascular involvement, and associated dysrhythmias. Frequently occurring symptoms include impaired sweating, lack of tear formation, photophobia, dryness of nasal and oral mucosa, itching and peeling of skin, nausea, dysphagia, and constipation unrelieved by laxatives or alternating with diarrhea. Initial nonspecific symptoms of lethargy, fatigue, headache, and decreased initiative are followed by autonomic symptoms including orthostatic lightheadedness, blurring of vision, abdominal pain, diarrhea, dryness of eyes, and disturbed micturition. The most common symptoms at onset are related to orthostatic intolerance, as well as gastrointestinal and sudomotor dysfunction.[6] Parasympathetic impairment (abdominal pain, vomiting, constipation, ileus, urinary retention, dilated unreactive pupils; loss of accommodation) may also be observed.
- Bickerstaff's brainstem encephalitis (BBE), a further variant of Guillain–Barré syndrome, is characterized by acute onset of ophthalmoplegia, ataxia, disturbance of consciousness, hyperreflexia or Babinski's sign. The course of the disease can be monophasic or remitting-relapsing. Large, irregular hyperintense lesions located mainly in the brainstem, especially in the pons, midbrain and medulla, are described in the literature. Despite severe initial presentation, BBE usually has a good prognosis. Magnetic resonance imaging plays a critical role in the diagnosis of BBE. A considerable number of BBE patients have associated axonal Guillain–Barré syndrome, indicative that the two disorders are closely related and form a continuous spectrum.
Signs and symptoms
The disorder is characterized by symmetrical weakness that usually affects the lower limbs first, and rapidly progresses in an ascending fashion. Patients generally notice weakness in their legs, manifesting as "rubbery legs" or legs that tend to buckle, with or without dysesthesias (numbness or tingling). As the weakness progresses upward, usually over periods of hours to days, the arms and facial muscles also become affected. Frequently, the lower cranial nerves may be affected, leading to bulbar weakness, oropharyngeal dysphagia (drooling, or difficulty swallowing and/or maintaining an open airway) and respiratory difficulties. Most patients require hospitalization and about 30% require ventilatory assistance for treatment of type II respiratory failure.[7] Facial weakness is also common. Eye movement abnormalities are not commonly seen in ascending GBS, but are a prominent feature in the Miller-Fisher variant.
Sensory loss, if present, usually takes the form of loss of proprioception (position sense) and areflexia (complete loss of deep tendon reflexes), an important feature of GBS. Loss of pain and temperature sensation is usually mild. In fact, pain is a common symptom in GBS, presenting as deep aching pain, usually in the weakened muscles, which patients compare to the pain from overexercising. These pains are self-limited and may be treated with standard analgesics. Bladder dysfunction may occur in severe cases, but is usually short-lived.
In severe cases of GBS, loss of autonomic function is common, manifesting as wide fluctuations in blood pressure, orthostatic hypotension (a fall in blood pressure on standing, leading to an increased risk of collapse), and cardiac arrhythmias.
Acute paralysis in Guillain–Barré syndrome may be related to sodium channel blocking factor in the cerebrospinal fluid. Significant issues involving intravenous salt and water administration may occur unpredictably in this patient group, resulting in SIADH, a cause of low sodium levels in the blood.
Cause
All forms of Guillain–Barré syndrome are autoimmune diseases, due to an immune response to foreign antigens (such as infectious agents) that mistargets host nerve tissues unintentionally through a mechanism known as molecular mimicry.[8] The targets of such immune attack are thought to be gangliosides, compounds naturally present in large quantities in human peripheral nerve tissues. The most well-described antecedent infection is the bacterium Campylobacter jejuni,[9][10] In addition, cytomegalovirus has a known association with GBS.[11] In many cases, identification of a specific cause is impossible. Some cases may be triggered by the influenza virus, or by an immune reaction to the influenza virus.[12] An increased incidence of Guillain–Barré syndrome followed influenza immunization during the 1976-1977 swine flu pandemic;[13] however, epidemiological studies since then have demonstrated either an extremely small increased risk following immunization (under one additional case per million vaccinations) or no increased risk.[14][15]
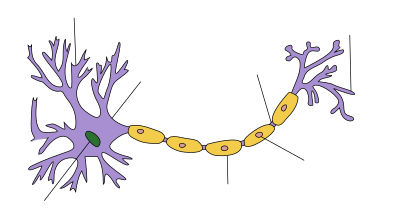
The end result of this autoimmune process is an attack on the peripheral nerves and damage to myelin, the fatty insulating layer of the nerve, and a nerve-conduction block leading to muscle paralysis that may be accompanied by sensory or autonomic disturbances.
In mild cases, nerve axon (the long slender conducting portion of a nerve) function remains intact and recovery can be rapid if remyelination occurs. In severe cases, axonal damage occurs, and recovery depends on the regeneration of this important tissue. About 80% of patients have myelin loss; in the remaining 20%, the pathological hallmark is axon loss.
Guillain–Barré, unlike disorders such as multiple sclerosis (MS) and Lou Gehrig's disease (ALS), is a purely peripheral nerve disorder and does not in general cause nerve damage to the brain or spinal cord.
Diagnosis
The diagnosis of GBS depends on findings such as rapid development of muscle paralysis, areflexia, absence of fever, and a likely inciting event. Cerebrospinal fluid analysis (through a lumbar spinal puncture) and electrodiagnostic tests of nerves and muscles (such as nerve conduction studies) are common tests ordered in the diagnosis of GBS.
Testing
In cerebrospinal fluid (CSF), characteristic findings include albumino-cytological dissociation. As opposed to infectious causes, this is an elevated protein level (100–1000 mg/dl), without an accompanying increased cell count (absence of pleocytosis). A sustained increased white blood cell count may indicate an alternative diagnosis such as infection.
Electromyography (EMG) and nerve conduction studies may show prolonged distal latencies, conduction slowing, conduction block, and temporal dispersion of compound action potential in demyelinating cases. F waves and H-reflexes may be prolonged or absent. Needle EMG is frequently normal in acute cases. Reduced, neuropathic recruitment in weak muscles can be seen. Fibrillations will be seen on needle EMG if some axonal injury occurs after three to four weeks. In primary axonal damage, the findings include reduced amplitude of the action potentials without conduction slowing.
Criteria
Features required for diagnosis are progressive weakness in legs and often arms, and areflexia (the absence of deep tendon reflexes).[16][17]
Features that strongly support diagnosis are progression of symptoms over days to four weeks, relative symmetry of symptoms, mild sensory symptoms or signs, cranial nerve involvement (especially bilateral weakness of facial muscles), autonomic dysfunction, pain (often present), high concentration of protein in CSF, and typical electrodiagnostic features.[16][17]
Features that should raise doubt about the diagnosis include severe pulmonary dysfunction with limited limb weakness at onset, severe sensory signs with limited weakness at onset, bladder or bowel dysfunction at onset, fever at onset, sharp sensory level, slow progression with limited weakness without respiratory involvement (subacute inflammatory demyelinating polyneuropathy or CIDP is more likely), marked persistent asymmetry of weakness, persistent bladder or bowel dysfunction, increased number of mononuclear cells in CSF (>50×106/L), and polymorphonuclear cells in CSF.[16][17]
Treatment
Supportive care is the cornerstone of successful management in the acute patient. Of greatest concern is respiratory failure due to paralysis of the diaphragm, the muscle most important for breathing. Intubation may be needed when evidence of impending failure of the muscles of breathing is present – when the vital capacity (VC) is less than 20 ml/kg, the negative inspiratory force (NIF) is less negative (i.e., closer to zero) than −25 cmH2O, more than 30% decrease in either VC or NIF within 24 hours, rapid progression of disorder, or autonomic instability.
Subsequent treatment consists of attempting to reduce the body's attack on the nervous system, either by plasmapheresis, filtering antibodies out of the blood stream, or by administering intravenous immunoglobulins (IVIg), to neutralize harmful antibodies and inflammation causing disease. These two treatments are equally effective and a combination of the two is not significantly better than either alone. Glucocorticoids have not been found to be effective in GBS.[18][19] Treatment is usually begun as soon as the diagnosis is made. Plasmapheresis hastens recovery when used within four weeks of the onset of symptoms.[19] IVIg has equivalent efficacy to plasmapheresis when started within two weeks of the onset of symptoms, and has fewer complications.[19] IVIg is usually used first because of its ease of administration and safety profile. Its use is not without risk; occasionally it causes hepatitis, or in rare cases, renal failure if used for longer than five days.
Following the acute phase, treatment often consists of rehabilitation with the help of a multidisciplinary team to focus on improving activities of daily living (ADLs). Occupational therapists may offer equipment (such as wheelchair and special cutlery) to help the patient achieve ADL independence. Physiotherapists assist to correct functional movement, avoiding harmful compensations that might have a negative effect in the long run. Also, some evidence supports physiotherapy in helping patients with Guillain–Barré syndrome to regain strength, endurance, and gait quality,[20] as well as helping them prevent contractures, bedsores, and cardiopulmonary difficulties.[21] Speech and language therapists help regain speaking and swallowing abilities, especially if the patient was intubated or received a tracheostomy.
Prognosis
Recovery usually starts after the fourth week from the onset of the disorder[citation needed]. About 80% of patients have a complete recovery within a few months to a year, although minor findings may persist, such as areflexia. About 5–10% recover with severe disability, with most of such cases involving severe proximal motor and sensory axonal damage with inability of axonal regeneration. Despite all improvements in treatment and supportive care, the death rate is still about 2–3%, even in the best intensive care units. Worldwide, the death rate runs slightly higher (4%), mostly from a lack of availability of life-support equipment during the lengthy plateau lasting four to six weeks, and in some cases up to one year, when a ventilator is needed in the worst cases. About 5–10% of patients have one or more late relapses, in which case they are then classified as having chronic inflammatory demyelinating polyneuropathy.
Poor prognostic factors include age over 40 years, history of preceding diarrheal illness, requiring ventilator support, high anti-GM1 titre, and poor upper-limb muscle strength.
Epidemiology
Worldwide, the annual incidence is about 0.6–4.0 occurrences per 100,000 people. Men are one and a half times more likely to be affected than women. The incidence increases with age; about one case per 100,000 occurs in people aged below 30 years and about four cases per 100,000 in those older than 75 years.[22] The incidence of GBS during pregnancy is 1.7 cases per 100,000 of the population.[23] Congenital and neonatal Guillain–Barré syndrome have also been reported.[24]
History
French physician Jean Landry first described the disorder in 1859. In 1916, Georges Guillain, Jean Alexandre Barré, and André Strohl diagnosed two soldiers with the illness and described the key diagnostic abnormality of increased spinal-fluid protein production, but normal cell count.[25]
GBS is also known as acute idiopathic polyradiculoneuritis, acute idiopathic polyneuritis, French polio, Landry's ascending paralysis and Landry–Guillain–Barré syndrome.
Canadian neurologist C. Miller Fisher described the variant that bears his name in 1956.[26]
Notable cases

- Ryūtarō Arimura, vocalist for Japanese rock band Plastic Tree: His case was detected and treated early, and Arimura was able to return to touring within three months.[27]
- Markus Babbel, former international footballer, contracted GBS in 2001, following a period suffering from the Epstein–Barr virus. He lost almost an entire year of his footballing career between the two illnesses, and never again demonstrated the same level of ability.[28]
- Tony Benn, British politician[29]
- Rachel Chagall, actress, contracted GBS in 1982. In 1987, she portrayed Gabriela Brimmer, a notable disabilities activist.[30]
- Tom Edlefsen, American tennis player, made the fourth round of Wimbledon in 1968, a year after he developed GBS.[31]
- Samuel Goldstein, American athlete and Paralympian[32]
- Andy Griffith, an American actor best known for The Andy Griffith Show and Matlock, developed GBS in 1983.[33]
- Joseph Heller, author, contracted GBS in 1981. This episode in his life is recounted in the autobiographical No Laughing Matter.[34]
- Luci Baines Johnson, daughter of President Lyndon Johnson and Lady Bird Johnson, was diagnosed and under treatment for GBS in April 2010.[35]
- Hugh McElhenny, former professional American football player with the San Francisco 49ers[36]
- Scott McKenzie (born Philip Wallach Blondheim), an American singer and songwriter most notable for his hit single and hippie anthem "San Francisco (Be Sure to Wear Flowers in Your Hair)", died August 18, 2012, at the age of 73 from GBS.[37]
- Lucky Oceans, Grammy Award-winning musician with Asleep at the Wheel, was diagnosed with GBS in 2008.[38]
- Len Pasquarelli, sports writer and analyst for ESPN and resident of the Pro Football Writers of America, was diagnosed in 2008.[39]
- Serge Payer, Canadian-born professional hockey player, after battling and overcoming the syndrome, set up the Serge Payer Foundation, which is dedicated to raising money for research into new treatments and cures for GBS.[40]
- William “The Refrigerator” Perry, former professional American football player with the Chicago Bears, was diagnosed with GBS in 2008.[41]
- Robert C. Samuels, journalist, contracted GBS in 1981. He recounts his struggle to survive in his book, Blue Water, White Water.[42].
- Georgena Sil, Canadian physicist and writer, after recovery, established Tuum Est, a nonprofit site devoted to legal rights of the physically disabled.[43]
- Norton Simon, American industrialist and philanthropist[44]
- Kay Smith (artist), current Illinois Artist Laureate, was diagnosed with Guillain-Barre syndrome at the age of 73, after extensive rehabilitation at the Rehabilitation Institute of Chicago she was able to continue painting and teaching[45]
- Kelly-Marie Stewart, British actress[46]
- Sabine Moussier, Mexican actress[47]
- Hans Vonk, Dutch conductor.[48]
- Morten Wieghorst, Danish former footballer and football coach[49]
- Danny Wuerffel, 1996 Heisman Trophy winner from the University of Florida[50]
- Mike Egener, Canadian hockey player[51]
- David Lim, Singaporean mountaineer
References
- ^ Davids, H. "Guillain-Barre Syndrome". Medscape Reference. Retrieved 3 Jan 2012.
- ^ Mori, M; Kuwabara, S; Fukutake, T; Hattori, T (2002). "Plasmapheresis and Miller Fisher syndrome: analysis of 50 consecutive cases". Journal of neurology, neurosurgery, and psychiatry. 72 (5): 680. doi:10.1136/jnnp.72.5.680. PMC 1737859. PMID 11971070.
- ^ McKhann GM, Cornblath DR, Ho T; et al. (1991). "Clinical and electrophysiological aspects of acute paralytic disease of children and young adults in northern China". Lancet. 338 (8767): 593–7. doi:10.1016/0140-6736(91)90606-P. PMID 1679153.
{{cite journal}}: Cite has empty unknown parameter:|month=(help); Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Ho TW, Mishu B, Li CY; et al. (1995). "Guillain-Barré syndrome in northern China. Relationship to Campylobacter jejuni infection and anti-glycolipid antibodies". Brain. 118 (3): 597–605. doi:10.1093/brain/118.3.597. PMID 7600081.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Griffin JW, Li CY, Ho TW; et al. (1995). "Guillain–Barré syndrome in northern China. The spectrum of neuropathological changes in clinically defined cases". Brain. 118 (3): 577–95. doi:10.1093/brain/118.3.577. PMID 7600080.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Suarez et al. 1994
- ^ Burt, Christiana C. (1 November 2009). "Respiratory failure". Surgery (Oxford). 27 (11): 475–479. doi:10.1016/j.mpsur.2009.09.007.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ CW, Ang (1 February 2004). "Guillain-Barré syndrome: a true case of molecular mimicry". Trends in Immunoology. 25 (2): 61–66. doi:10.1016/j.it.2003.12.004.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Yuki N (2008). "[Campylobacter genes responsible for the development and determinant of clinical features of Guillain-Barré syndrome]". Nippon Rinsho. Japanese Journal of Clinical Medicine (in Japanese). 66 (6): 1205–10. PMID 18540372.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Kuwabara S.; et al. (2004-08-10). "Does Campylobacter jejuni infection elicit "demyelinating" Guillain-Barré syndrome?". Neurology. 63 (3). Lippincott Williams & Wilkins: 529–33. doi:10.1212/01.WNL.0000133205.05169.04. PMID 15304587.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Orlikowski D; Porcher, R.; Sivadon-Tardy, V.; Quincampoix, J.-C.; Raphael, J.-C.; Durand, M.-C.; Sharshar, T.; Roussi, J.; Caudie, C. (2011). "Guillain–Barré Syndrome following Primary Cytomegalovirus Infection: A Prospective Cohort Study". Clin Infect Dis. 52 (7): 837–844. doi:10.1093/cid/cir074. PMID 21427390.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Sivadon-Tardy V.; et al. (Jan 1, 2009). "Guillain-Barré syndrome and influenza virus infection". Clinical Infectious Diseases. 48 (1). The University of Chicago Press: 48–56. doi:10.1086/594124. PMID 19025491.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Haber P; et al. (Nov 24, 2004). "Guillain-Barré syndrome following influenza vaccination". JAMA. 292 (20): 2478–81. doi:10.1001/jama.292.20.2478. PMID 15562126.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Lehmann HC P; et al. (Sep 2010). "Guillain-Barré syndrome following influenza vaccination". Lancet Infect Dis. 10 (9): 643–51. doi:10.1016/S1473-3099(10)70140-7. PMID 20797646.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Liang; Li, Li; Liu, Da-Wei; Li, Ke-Li; Wu, Wen-Di; Zhu, Bao-Ping; Wang, Hua-Qing; Luo, Hui-Ming; Cao, Ling-Sheng; et al. (2011). "Safety of Influenza A (H1N1) Vaccine in Postmarketing Surveillance in China". New England Journal of Medicine. 364 (7): 638–647. doi:10.1056/NEJMoa1008553. PMID 21288090.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - ^ a b c van Doorn PA, Ruts L, Jacobs BC (2008). "Clinical features, pathogenesis, and treatment of Guillain-Barré syndrome". Lancet Neurol. 7 (10): 939–50. doi:10.1016/S1474-4422(08)70215-1. PMID 18848313.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b c Lerner AJ. Diagnostic Criteria in Neurology (Current Clinical Neurology). Totowa, NJ: Humana Press. p. 186. ISBN 1-61737-594-2.
- ^ Merck Manual [Online]. Peripheral Neuropathy, Treatment. Retrieved 8-22-2009.
- ^ a b c Hughes RA, Wijdicks EF, Barohn R; et al. (2003). "Practice parameter: immunotherapy for Guillain-Barré syndrome: report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 61 (6): 736–40. doi:10.1212/WNL.61.6.736. PMID 14504313.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Davidson, I., Wilson, C., Walton, T., & Brissenden, S. (2009). Physiotherapy and Guillain–Barre syndrome: Results of a national survey. Physiotherapy, 95(3), 157–163.Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1016/j.physio.2009.04.001, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1016/j.physio.2009.04.001instead. - ^ Karavatas, S. G. (2005). The role of neurodevelopmental sequencing in the physical therapy management of a geriatric patient with Guillain–Barre syndrome. Topics in Geriatric Rehabilitation, 21(2), 133–135.
- ^ Pithadia AB, Kakadia N. (2010). "Guillain-Barré syndrome (GBS)" (PDF). Pharmacol Rep. 62 (2): 220–32. PMID 20508277.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Brooks, H (2000). "Pregnancy, anaesthesia and Guillain-Barré syndrome". Anaesthesia. 55 (9): 894–8. doi:10.1046/j.1365-2044.2000.01367.x. PMID 10947755.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Iannello, S (2004). Guillain–Barré syndrome: Pathological, clinical and therapeutical aspects. Nova Publishers. ISBN 1-59454-170-1.
- ^ Guillain-Barré-Strohl syndrome and Miller Fisher's syndrome at Who Named It?
- ^ Fisher CM (1956). "An unusual variant of acute idiopathic polyneuritis (syndrome of ophthalmolplegia, ataxia and areflexia)". N. Engl. J. Med. 255 (2): 57–65. doi:10.1056/NEJM195607122550201. PMID 13334797.
- ^ "Plastic Tree's vocalist, Arimura Ryutaro recovers from "Guillain-Barre syndrome"". Tokyohive.com. 2011-01-20. Retrieved 2012-10-20.
- ^ Wallace, Sam (2002-08-10). "Grateful Babbel a tower of strength again". London: Telegraph. Retrieved 2009-11-23.
- ^ Lea, Robert (2002-10-17). "Relative Values: Tony and Josh Benn". London: The Times. Retrieved 2009-01-15.
- ^ "Gaby, A True Story (1987)". Films involving Disabilities.
- ^ Los Angeles Times, "Tom Edlefsen Beats Virus", 30 June 1968
- ^ The case of Sam Goldstein and the swine flu vaccine, jta.org, May 5, 2009
- ^ "Andy in Guideposts Magazine".
- ^ Vogel, Speed; Heller, Joseph (2004). No Laughing Matter. New York: Simon & Schuster. ISBN 0-7432-4717-5.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ "Luci Baines Johnson hospitalized with nervous system disorder".
- ^ Raley, Dan (2004-09-02). "The untold story of Hugh McElhenny, the King of Montlake". Seattle PI. Retrieved 2010-01-07.
- ^ "Scott McKenzie Dead". Celebritydiagnosis.com. 2012-08-21. Retrieved 2012-10-20.
- ^ "Lucky Oceans in hospital". The Australian. 2008-10-13. Retrieved 2008-10-28.
- ^ "Chris Mortensen on Len Pasquarelli's comeback". ESPN.com. 2009-01-26. Retrieved 2009-01-26.
- ^ Serge Payer Foundation, Serge Payer Foundation Mission.
- ^ . YumaSun.com. 2008-09-08 http://www.yumasun.com/sports/tatum_44249___article.html/perry_night.html. Retrieved 2008-10-28.
{{cite news}}: Missing or empty|title=(help) - ^ Samuels, Robert C., New York Times 12 March 2012 review of Blue Water, White Water.
- ^ Georgena Sil (1993). "Coming to Grips with Guillain-Barré Syndrome". The Medical Post. 29 (5): 32.
- ^ "Norton Simon Biography". Retrieved 13 October 2009.
- ^ Artist Discovers That A Still Life Can Be Moving http://articles.chicagotribune.com/1997-05-18/news/9705180077_1_guillain-barre-syndrome-paint-tahiti
- ^ Sutton, Jessica. "Kelly-Marie Stewart: disability and motherhood". Retrieved 3 January 2013.
- ^ "People en español".
- ^ Kozinn, Allan (2004-08-31). "Hans Vonk, 63, Conductor Of the St. Louis Symphony". The New York Times. Retrieved 2009-08-26.
- ^ "Recovering Wieghorst is now talking". BBC News. 2000-11-01.
- ^ Dooley, Pat. "Wuerffel hospitalized to treat nervous system disorder". Gatorsports.com. Retrieved 16 June 2011.
- ^ http://www.coventryblaze.co.uk/index.php/news/latest-news/631-egener-illness-forces-contract-cancellation
Literature
- Pithadia AB, Kakadia N. (2010). "Guillain-Barré syndrome (GBS)" (PDF). Pharmacol Rep. 62 (2): 220–32. PMID 20508277.
{{cite journal}}: Unknown parameter|month=ignored (help) - Newswanger DL, Warren CR (2004). "Guillain-Barré syndrome" (PDF). Am Fam Physician. 69 (10): 2405–10. PMID 15168961.
{{cite journal}}: Unknown parameter|month=ignored (help)