Chorionic hematoma
Chorionic hematoma (also chorionic hemorrhage) is the pooling of blood (hematoma) between the chorion, a membrane surrounding the embryo, and the uterine wall.[1] With an incidence of 3.1% of all pregnancies,[1] it is the most common sonographic abnormality and the most common cause of first trimester bleeding.[2]
Cause and diagnosis
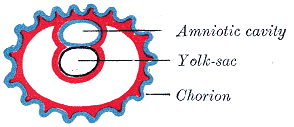
Chorionic hematomas can be caused by the separation of the chorion from the endometrium (inner membrane of the uterus). Hematomas are classified by their location between tissue layers:[3]
- Subchorionic hematomas, the most common type, are between the chorion and endometrium.
- Retroplacental hematomas are entirely behind the placenta and not touching the gestational sac.
- Subamniotic or preplacental hematomas are contained within amnion and chorion. Rare.
Most patients with a small subchorionic hematoma are asymptomatic.[4] Symptoms include vaginal bleeding, abdominal pain, premature labor and threatened abortion.[5]
Ultrasonography is the preferred method of diagnosis.[6] A chorionic hematoma appears on ultrasound as a hypoechoic crescent adjacent to the gestational sac. The hematoma is considered small if it is under 20% of the size of the sac and large if it is over 50%.[1]
Prognosis and treatment
The presence of subchorionic bleeding around the gestational sac does not have a significant association with miscarriage overall.[7] However, the case of intrauterine hematoma observed before 9 weeks of gestational age has been associated with an increased risk of miscarriage.[8] Bed rest for the duration of bleeding has been associated with a lower rate of miscarriage and a higher rate of term pregnancy.[9]
References
- ^ a b c Nagy, Sándor MD; Bush, Melissa MD; Stone, Joanne MD; Lapinski, Robert H. PhD; Gardó, Sándor MD, DSci. Clinical Significance of Subchorionic and Retroplacental Hematomas Detected in the First Trimester of Pregnancy [1]. Obstetrics & Gynecology: July 2003 - Volume 102 - Issue 1 - p 94-100
- ^ Avneesh Chhabra, MD et al. "Subchorionic Hemorrhage" [2], Medscape.
- ^ Trop, Isabelle and Levine, Deborah. Hemorrhage During Pregnancy: Sonography and MR Imaging [3]. Amer J Roentgenology 2001; 176:607-615.
- ^ Trop I, Levine D. Hemorrhage during pregnancy: sonography and MR imaging. AJR Am J Roentgenol. Mar 2001;176(3):607-15.
- ^ Hodgson DT, Lotfipour S, Fox JC. Vaginal bleeding before 20 weeks gestation due to placental abruption leading to disseminated intravascular coagulation and fetal loss after appearing to satisfy criteria for routine threatened abortion: a case report and brief review of the literature. J Emerg Med. May 2007;32(4):387-92
- ^ Abu-Yousef MM, Bleicher JJ, Williamson RA, Weiner CP. Subchorionic hemorrhage: sonographic diagnosis and clinical significance. AJR Am J Roentgenol. Oct 1987;149(4):737-40.
- ^ N. Stamatopoulos; C. Lu; F. Infante; U. Menakaya; I. Casikar; S. Reid; M. Mongelli; G. Condous (2013). "OP03.03: Does the presence of subchorionic haematoma increase the risk of miscarriage?". Ultrasound in Obstetrics & Gynecology. 42 (s1). doi:10.1002/uog.12736.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help) - ^ Maso, G.; Dʼottavio, G.; De Seta, F.; Sartore, A.; Piccoli, M.; Mandruzzato, G. (2005). "First-Trimester Intrauterine Hematoma and Outcome of Pregnancy". Obstetrics & Gynecology. 105 (2): 339. doi:10.1097/01.AOG.0000152000.71369.bd.
- ^ Ben-Haroush A, Yogev Y, Mashiach R, Meizner I. Pregnancy outcome of threatened abortion with subchorionic hematoma: possible benefit of bed-rest? Journal Isr Med Assoc J. 2003 Jun;5(6):422-4
