D-dimer
D-dimer is a fibrin degradation product, a small protein fragment present in the blood after a blood clot is degraded by fibrinolysis. It is so named because it contains two crosslinked D fragments of the fibrinogen protein.[1]
D-dimer concentration may be determined by a blood test to help diagnose thrombosis. Since its introduction in the 1990s, it has become an important test performed in patients suspected of thrombotic disorders. While a negative result practically rules out thrombosis, a positive result can indicate thrombosis but does not rule out other potential causes. Its main use, therefore, is to exclude thromboembolic disease where the probability is low. In addition, it is used in the diagnosis of the blood disorder disseminated intravascular coagulation.[1]
Principles
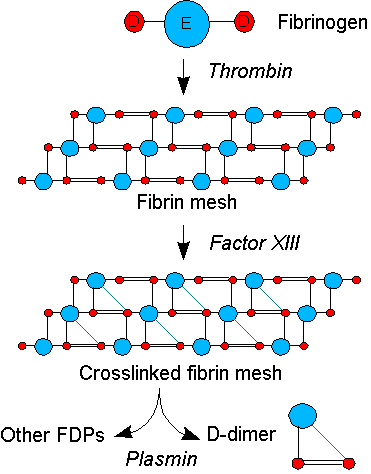
Coagulation, the formation of a blood clot or thrombus, occurs when the proteins of the "coagulation cascade" are activated, either by contact with damaged blood vessel wall (intrinsic pathway) or by activation of factor VII by tissue activating factors. Both pathways lead to the generation of thrombin, an enzyme that turns the soluble blood protein fibrinogen into fibrin, which aggregates into proteofibrils. Another thrombin-generated enzyme, factor XIII, then crosslinks the fibrin proteofibrils at the D fragment site, leading to the formation of an insoluble gel which serves as a scaffold for blood clot formation.[1]
The circulating enzyme plasmin, the main enzyme of fibrinolysis, cleaves the fibrin gel in a number of places. The resultant fragments, "high molecular weight polymers", are digested several times more by plasmin to lead to intermediate and then to small polymers (fibrin degradation products or FDPs). The cross-link between two D fragments remains intact, however, and these are exposed on the surface when the fibrin fragments are sufficiently digested. The typical D-dimer containing fragment contains two D domains and one E domain of the original fibrinogen molecule.[1]
D-dimers are not normally present in human blood plasma, except when the coagulation system has been activated, for instance because of the presence of thrombosis or disseminated intravascular coagulation. The D-dimer assay depends on the binding of a monoclonal antibody to a particular epitope on the D-dimer fragment. Several detection kits are commercially available; all of them rely on a different monoclonal antibody against D-dimer. Of some of these it is known to which area on the D-dimer the antibody binds. The binding of the antibody is then measured quantitatively by one of various laboratory methods.[1]
Indications
D-dimer testing is of clinical use when there is a suspicion of deep venous thrombosis (DVT) or pulmonary embolism (PE). In patients suspected of disseminated intravascular coagulation (DIC), D-dimers may aid in the diagnosis.[citation needed]
For DVT and PE, there are various scoring systems that are used to determine the a priori clinical probability of these diseases; the best-known were introduced by Wells et al. (2003).
- For a very high score, or pretest probability, a D-dimer will make little difference and anticoagulant therapy will be initiated regardless of test results, and additional testing for DVT or pulmonary embolism may be performed.
- For a moderate or low score, or pretest probability:[2]
- A negative D-dimer test will virtually rule out thromboembolism: the degree to which the D-dimer reduces the probability of thrombotic disease is dependent on the test properties of the specific test used in your clinical setting: most available D-dimer tests with a negative result will reduce the probability of thromboembolic disease to less than 1% if the pretest probability is less than 15-20%
- If the D-dimer reads high, then further testing (ultrasound of the leg veins or lung scintigraphy or CT scanning) is required to confirm the presence of thrombus. Anticoagulant therapy may be started at this point or withheld until further tests confirm the diagnosis, depending on the clinical situation.
In some hospitals, they are measured by laboratories after a form is completed showing the probability score and only if the probability score is low or intermediate. This would reduce the need for unnecessary tests in those who are high-probability.[3]
Test properties
Various kits have a 93-95% sensitivity and about 50% specificity in the diagnosis of thrombotic disease.[4]
- False positive readings can be due to various causes: liver disease, high rheumatoid factor, inflammation, malignancy, trauma, pregnancy, recent surgery as well as advanced age
- False negative readings can occur if the sample is taken either too early after thrombus formation or if testing is delayed for several days. Additionally, the presence of anti-coagulation can render the test negative because it prevents thrombus extension.
- Likelihood ratios are derived from sensitivity and specificity to adjust pretest probability.
History
D-dimer was originally described in the 1970s, and found its diagnostic application in the 1990s.[1]
References
- ^ a b c d e f Adam SS, Key NS, Greenberg CS (2009). "D-dimer antigen: current concepts and future prospects". Blood. 113 (13): 2878–87. doi:10.1182/blood-2008-06-165845. PMID 19008457.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Wells PS, Anderson DR, Rodger M; et al. (2003). "Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis". N. Engl. J. Med. 349 (13): 1227–35. doi:10.1056/NEJMoa023153. PMID 14507948.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Rathbun, SW (2004). "Clinical utility of D-dimer in patients with suspected pulmonary embolism and nondiagnostic lung scans or negative CT findings". Chest. 125 (125): 851. doi:10.1378/chest.125.3.851. PMID 15006941.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Schrecengost JE, LeGallo RD, Boyd JC, Moons KG, Gonias SL, Rose CE Jr, Bruns DE. Comparison of diagnostic accuracies in outpatients and hospitalized patients of D-dimer testing for the evaluation of suspected pulmonary embolism. Clin Chem 2003;49:1483-90. PMID 12928229.
