Surfactant protein A1
| SFTPA1 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | SFTPA1, COLEC4, PSAP, PSP-A, PSPA, SFTP1, SFTPA1B, SP-A, SP-A1, SPA, SPA1, surfactant protein A1, SP-A1 beta, SP-A1 delta, SP-A1 gamma, SP-A1 epsilon, ILD1 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 178630; MGI: 109518; HomoloGene: 3946; GeneCards: SFTPA1; OMA:SFTPA1 - orthologs | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Surfactant protein A1 (SP-A1), also known as Pulmonary surfactant-associated protein A1 (PSP-A) is a protein that in humans is encoded by the SFTPA1 gene.[5][6]
Summary
[edit]SP-A1 is primarily synthesised in type II alveolar cells in the lung, as part of a complex of lipids and proteins known as pulmonary surfactant. The function of this complex is to reduce surface tension in the alveoli and prevent their collapse during expiration. The protein component of surfactant helps in the modulation of the innate immune response, and inflammatory processes.

SP-A1 is a member of a subfamily of C-type lectins called collectins. Together with SP-A2, they are the most abundant proteins of pulmonary surfactant. SP-A1 binds to the carbohydrates found in the surface of several microorganisms and helps in the defense against respiratory pathogens.[7][8][9]
Surfactant homeostasis is critical for breathing (and thus survival) in the prematurely born infant, but also for maintaining lung health, and normal lung function throughout life. Changes in the amount or composition of surfactant can alter its function and are associated with respiratory diseases.[10][11][12][13]
SFTPA1 expression
[edit]The lung is the main site of SFTPA1 synthesis, but SFTPA1 mRNA expression has also been detected in the trachea, prostate, pancreas, thymus, colon, eye, salivary gland and other tissues.[14] Using specific monoclonal antibodies for Surfactant protein A, the protein can be detected in lung alveolar type II pneumocytes, club cells, and alveolar macrophages, but no extrapulmonary SP-A immunoreactivity was observed.[14]
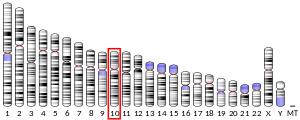
Gene
[edit]SFTPA1 is located in the long arm q of chromosome 10, close to SFTPA2. The SFTPA1 gene is 4505 base pairs in length, and 94% similar to SFTPA2. The structure of SFTPA1 consists of four coding exons (I-IV), and several 5'UTR untranslated exons (A, B, B', C, C', D, D').[15][16] The expression of SFTPA1 is regulated by cellular factors including proteins, small RNAs (microRNAs), glucocorticoids, etc. Its expression is also regulated by epigenetic and environmental factors.[17]
Differences in the SFTPA1 gene sequence at the coding region determine SP-A genetic variants or haplotypes among individuals.[16] More than 30 variants have been identified and characterized for SFTPA1 (and SFTPA2) in the population. SFTPA1 variants result from nucleotide changes in the codons of amino acids 19, 50, 62, 133, and 219. Two of these do not modify the SP-A1 protein sequence (amino acids 62 and 133), whereas the rest result in amino acid substitutions (amino acid 19, 50, 133, and 219). Four SP-A1 variants (6A, 6A2, 6A3, 6A4) are in higher frequency in the general population. The most frequently found variant is 6A2.[18][19]
Structure
[edit]Surfactant protein A (SP-A) is a protein of 248 amino acids usually found in large oligomeric structures. The mature SP-A1 monomer is a 35kDa protein that differs from SP-A2 in four amino acids at the coding region. The structure of SP-A1 monomers consists of four domains: an N-terminal, a collagen-like domain, a neck region, and a carbohydrate recognition domain. The C-terminal carbohydrate recognition domain (CRD) allows binding to various types of microorganisms and molecules.[18][19] The amino acid differences that distinguish between SP-A1 and SP-A2 genes and between their corresponding variants are located at the collagen-like domain. The amino acid differences that distinguish among SFTPA1 variants are located both at the carbohydrate recognition and the collagen-like domains.[18][20]
SP-A1 monomers group with other SP-A1 or SP-A2 monomers in trimeric structural subunits of 105kDa. Six of these structures group in 630 kDa structures that resemble flower bouquets. These oligomers contain a total of eighteen SP-A1 and/or SP-A2 monomers.[18]
Functions
[edit]- Binding of pathogens, allergens, and other molecules
- Increasing phagocytosis and chemotaxis of alveolar macrophages
- Induction of proliferation of immune cells
- Stimulation of proinflammatory cytokine production
- Modulation of the generation of reactive oxygen species
- Serving as a hormone in parturition
- Maintaining the structure of tubular myelin (an extracellular form of surfactant)
Innate immunity
[edit]The role of SFTPA1 in innate immunity has been extensively studied. SP-A has the ability to bind and agglutinate bacteria, fungi, viruses, and other non-biological antigens. Some of the functions by which both SFTPA1 and SFTPA2 contribute to innate immunity include:
- opsonization of bacteria for phagocytosis by alveolar macrophages
- recruitment of monocytes and neutrophils to the site of inflammation/infection
- enhancement of pathogen-killing mechanisms: phagocytosis, release of reactive oxygen species, release of nitric oxide
- control of cytokine production by immune cells
- transition of innate immunity to adaptive immunity (by interaction with cell surface receptors of dendritic cells to allow antigen presentation)
Environmental insults such as air pollution, and exposure to high concentrations of ozone and particulate matter can affect SP-A expression and function, via mechanisms that involve epigenetic regulation of SFTPA1 expression.[17]
Clinical significance
[edit]Deficiency in SP-A levels is associated with infant respiratory distress syndrome in prematurely born infants with developmental insufficiency of surfactant production and structural immaturity in the lungs.[21]
SFTPA1 genetic variants, SNPs, haplotypes, and other genetic variations have been associated with acute and chronic lung disease in several populations of neonates, children, and adults.[10] Genetic variations in SFTPA1 have been associated with susceptibility to idiopathic pulmonary fibrosis, a lung disease characterized by shortness of breath, pulmonary infiltrates and inflammation that results in acute lung damage with subsequent scarring of lung tissue.[22] Genetic variations in SFTPA1 are also a cause of susceptibility to respiratory distress syndrome in premature infants, a lung disease characterized by deficient gas exchange, diffuse atelectasis, high-permeability lung edema and fibrin-rich alveolar deposits "surfactant protein A1".. The ratio of SP-A1 to total SP-A has been correlated with lung disease (e.g. asthma, cystic fibrosis) and aging.[23][24] Methylation of SFTPA1 promoter sequences has also been found in lung cancer tissue.[25][26]
SFTPA1 mRNA transcript variants
[edit]| Variant id | 5'UTR splice | Coding | 3'UTR sequence | GenBank id |
|---|---|---|---|---|
| AD'6A | AD' | 6A | 6A | HQ021433 |
| AD'6A2 | AD' | 6A2 | 6A2 | HQ021434 |
| AD'6A3 | AD' | 6A3 | 6A3 | HQ021435 |
| AD'6A4 | AD' | 6A4 | 6A4 | HQ021436 |
| AB'D'6A | AB'D' | 6A | 6A | JX502764 |
| AB'D'6A2 | AB'D' | 6A2 | 6A2 | HQ021437 |
| AB'D'6A3 | AB'D' | 6A3 | 6A3 | HQ021438 |
| AB'D'6A4 | AB'D' | 6A4 | 6A4 | HQ021439 |
| ACD'6A | ACD' | 6A | 6A | JX502765 |
| ACD'6A2 | ACD' | 6A2 | 6A2 | HQ021440 |
| ACD'6A3 | ACD' | 6A3 | 6A3 | HQ021441 |
| ACD'6A4 | ACD' | 6A4 | 6A4 | HQ021442 |
| SFTPA1 variant 1 | AB'D' | 6A3 | 6A3 | NM_005411.4 |
| SFTPA1 variant 2 | ACD' | 6A3 | 6A3 | NM_001093770.2 |
| SFTPA1 variant 3 | ABD' | 6A3 | 6A3 | NM_001164644.1 |
| SFTPA1 variant 4 | AD' | 6A3 | 6A3 | NM_001164647.1 |
| SFTPA1 variant 5 | ACD' | 6A3 (truncated) | 6A3 | NM_001164645.1 |
| SFTPA1 variant 6 | AB'D' | 6A3 (truncated) | 6A3 | NM_001164646.1 |
Gene regulation
[edit]Gene expression of SFTPA1 is regulated at different levels including gene transcription, post-transcriptional processing, stability and translation of mature mRNA.[6] One of the important features of human surfactant protein A mRNAs is that they have a variable five prime untranslated region (5'UTR) generated from splicing variation of exons A, B, C, and D.[27][28] At least 10 forms of human SFTPA1 and SFTPA2 5'UTRs have been identified that differ in nucleotide sequence, length, and relative amount.[29] Specific SFTPA1 or SFTPA2 5'UTRs have also been characterized. Some SFTPA1 specific 5'UTRs include exons B' or C. These two exons contain upstream AUGs (uAUGs) that can potentially act as sites for translation initiation (see eukaryotic translation), affecting protein translation and SFTPA1 relative content. The majority of SFTPA1 transcripts lack exon B, a sequence implicated in transcription and translation enhancement, indicating a differential regulation of SFTPA1 and SFTPA2 expression.[30] The AD' form is the most represented among SFTPA1 transcripts (81%),[29] and experimental work has shown that this sequence can stabilize mRNA and enhance translation, but the mechanisms implicated in this regulation are still under investigation.[31][32][33] While differences at the 5'UTR are shown to regulate both transcription and translation,[30] polymorphisms at the 3'UTR of SP-A1 variants are shown to primarily, differentially affect translation efficiency[32] via mechanisms that involve binding of proteins[34] and/or [microRNAs].[32] The impact of this regulation on SFTPA1 and SFTPA2 protein levels may contribute to individual differences in susceptibility to lung disease.[23][24] Environmental insults and pollutants also affect SFTPA1 expression. Exposure of lung cells to particulate matter affects splicing of 5'UTR exons of SFTPA1 transcripts. Pollutants and viral infections also affect SFTPA1 translation mechanisms (see eukaryotic translation, translation (biology)).[31][35]
Notes
[edit]
The 2013 version of this article was updated by an external expert under a dual publication model. The corresponding academic peer reviewed article was published in Gene and can be cited as: Joanna Floros (1 December 2013). "Genetic complexity of the human surfactant-associated proteins SP-A1 and SP-A2". Gene. 531 (2): 126–132. doi:10.1016/J.GENE.2012.09.111. PMC 3570704. PMID 23069847. |
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000122852 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000021789 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Entrez Gene: Surfactant protein A1".
- ^ a b Silveyra P, Floros J (Dec 2013). "Genetic complexity of the human surfactant-associated proteins SP-A1 and SP-A2". Gene. 531 (2): 126–32. doi:10.1016/j.gene.2012.09.111. PMC 3570704. PMID 23069847.
- ^ Crouch EC (Aug 1998). "Collectins and pulmonary host defense". American Journal of Respiratory Cell and Molecular Biology. 19 (2): 177–201. doi:10.1165/ajrcmb.19.2.140. PMID 9698590.
- ^ Crouch E, Hartshorn K, Ofek I (Feb 2000). "Collectins and pulmonary innate immunity". Immunological Reviews. 173: 52–65. doi:10.1034/j.1600-065x.2000.917311.x. PMID 10719667. S2CID 22948014.
- ^ Phelps DS (2001). "Surfactant regulation of host defense function in the lung: a question of balance". Pediatric Pathology & Molecular Medicine. 20 (4): 269–92. doi:10.1080/15513810109168822. PMID 11486734. S2CID 19109567.
- ^ a b Silveyra P, Floros J (2012). "Genetic variant associations of human SP-A and SP-D with acute and chronic lung injury". Frontiers in Bioscience. 17 (2): 407–29. doi:10.2741/3935. PMC 3635489. PMID 22201752.
- ^ Floros J, Kala P (1998). "Surfactant proteins: molecular genetics of neonatal pulmonary diseases". Annual Review of Physiology. 60: 365–84. doi:10.1146/annurev.physiol.60.1.365. PMID 9558469.
- ^ Floros J, Wang G (May 2001). "A point of view: quantitative and qualitative imbalance in disease pathogenesis; pulmonary surfactant protein A genetic variants as a model". Comparative Biochemistry and Physiology A. 129 (1): 295–303. doi:10.1016/S1095-6433(01)00325-7. PMID 11369553.
- ^ Whitsett JA, Wert SE, Weaver TE (2010). "Alveolar surfactant homeostasis and the pathogenesis of pulmonary disease". Annual Review of Medicine. 61: 105–19. doi:10.1146/annurev.med.60.041807.123500. PMC 4127631. PMID 19824815.
- ^ a b Madsen J, Tornoe I, Nielsen O, Koch C, Steinhilber W, Holmskov U (Nov 2003). "Expression and localization of lung surfactant protein A in human tissues". American Journal of Respiratory Cell and Molecular Biology. 29 (5): 591–7. CiteSeerX 10.1.1.321.5856. doi:10.1165/rcmb.2002-0274OC. PMID 12777246.
- ^ Floros J, Hoover RR (Nov 1998). "Genetics of the hydrophilic surfactant proteins A and D". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1408 (2–3): 312–22. doi:10.1016/S0925-4439(98)00077-5. PMID 9813381.
- ^ a b DiAngelo S, Lin Z, Wang G, Phillips S, Ramet M, Luo J, Floros J (Dec 1999). "Novel, non-radioactive, simple and multiplex PCR-cRFLP methods for genotyping human SP-A and SP-D marker alleles". Disease Markers. 15 (4): 269–81. doi:10.1155/1999/961430. PMC 3851098. PMID 10689550.
- ^ a b Silveyra P, Floros J (2012). "Air pollution and epigenetics: effects on SP-A and innate host defence in the lung". Swiss Medical Weekly. 142: w13579. doi:10.4414/smw.2012.13579. PMC 3601480. PMID 22553125.
- ^ a b c d Floros J, Wang G, Mikerov AN (2009). "Genetic complexity of the human innate host defense molecules, surfactant protein A1 (SP-A1) and SP-A2--impact on function". Critical Reviews in Eukaryotic Gene Expression. 19 (2): 125–37. doi:10.1615/critreveukargeneexpr.v19.i2.30. PMC 2967201. PMID 19392648.
- ^ a b Floros, Joanna; Wang, Guirong; Lin, Zhenwu (June 2005). "ingentaconnect Genetic Diversity of Human SP-A, a Molecule with Innate host Defe..." Current Pharmacogenomics. 3 (2): 87–95. doi:10.2174/1570160054022935.
- ^ Wang G, Myers C, Mikerov A, Floros J (Jul 2007). "Effect of cysteine 85 on biochemical properties and biological function of human surfactant protein A variants". Biochemistry. 46 (28): 8425–35. doi:10.1021/bi7004569. PMC 2531219. PMID 17580966.
- ^ deMello DE, Heyman S, Phelps DS, Floros J (May 1993). "Immunogold localization of SP-A in lungs of infants dying from respiratory distress syndrome". The American Journal of Pathology. 142 (5): 1631–40. PMC 1886897. PMID 8494055.
- ^ Selman M, King TE, Pardo A (Jan 2001). "Idiopathic pulmonary fibrosis: prevailing and evolving hypotheses about its pathogenesis and implications for therapy". Annals of Internal Medicine. 134 (2): 136–51. doi:10.7326/0003-4819-134-2-200101160-00015. PMID 11177318. S2CID 10955241.
- ^ a b Tagaram HR, Wang G, Umstead TM, Mikerov AN, Thomas NJ, Graff GR, Hess JC, Thomassen MJ, Kavuru MS, Phelps DS, Floros J (May 2007). "Characterization of a human surfactant protein A1 (SP-A1) gene-specific antibody; SP-A1 content variation among individuals of varying age and pulmonary health". American Journal of Physiology. Lung Cellular and Molecular Physiology. 292 (5): L1052–63. doi:10.1152/ajplung.00249.2006. PMID 17189324. S2CID 21421799.
- ^ a b Wang Y, Voelker DR, Lugogo NL, Wang G, Floros J, Ingram JL, Chu HW, Church TD, Kandasamy P, Fertel D, Wright JR, Kraft M (Oct 2011). "Surfactant protein A is defective in abrogating inflammation in asthma". American Journal of Physiology. Lung Cellular and Molecular Physiology. 301 (4): L598–606. doi:10.1152/ajplung.00381.2010. PMC 3191759. PMID 21784968.
- ^ Vaid M, Floros J (Jan 2009). "Surfactant protein DNA methylation: a new entrant in the field of lung cancer diagnostics? (Review)". Oncology Reports. 21 (1): 3–11. doi:10.3892/or_00000182. PMC 2899699. PMID 19082436.
- ^ Lin Z, Thomas NJ, Bibikova M, Seifart C, Wang Y, Guo X, Wang G, Vollmer E, Goldmann T, Garcia EW, Zhou L, Fan JB, Floros J (Jul 2007). "DNA methylation markers of surfactant proteins in lung cancer". International Journal of Oncology. 31 (1): 181–91. doi:10.3892/ijo.31.1.181. PMID 17549420.
- ^ Karinch AM, Deiter G, Ballard PL, Floros J (Jun 1998). "Regulation of expression of human SP-A1 and SP-A2 genes in fetal lung explant culture". Biochimica et Biophysica Acta (BBA) - Gene Structure and Expression. 1398 (2): 192–202. doi:10.1016/S0167-4781(98)00047-5. PMID 9689918.
- ^ Karinch AM, Floros J (Apr 1995). "Translation in vivo of 5' untranslated-region splice variants of human surfactant protein-A". The Biochemical Journal. 307 (2): 327–30. doi:10.1042/bj3070327. PMC 1136651. PMID 7733864.
- ^ a b Karinch AM, Floros J (Jan 1995). "5' splicing and allelic variants of the human pulmonary surfactant protein A genes". American Journal of Respiratory Cell and Molecular Biology. 12 (1): 77–88. doi:10.1165/ajrcmb.12.1.7811473. PMID 7811473.
- ^ a b Silveyra P, Raval M, Simmons B, Diangelo S, Wang G, Floros J (Nov 2011). "The untranslated exon B of human surfactant protein A2 mRNAs is an enhancer for transcription and translation". American Journal of Physiology. Lung Cellular and Molecular Physiology. 301 (5): L795–803. doi:10.1152/ajplung.00439.2010. PMC 3290452. PMID 21840962.
- ^ a b Wang G, Guo X, Silveyra P, Kimball SR, Floros J (Apr 2009). "Cap-independent translation of human SP-A 5'-UTR variants: a double-loop structure and cis-element contribution". American Journal of Physiology. Lung Cellular and Molecular Physiology. 296 (4): L635–47. doi:10.1152/ajplung.90508.2008. PMC 2670766. PMID 19181744.
- ^ a b c Silveyra P, Wang G, Floros J (Oct 2010). "Human SP-A1 (SFTPA1) variant-specific 3' UTRs and poly(A) tail differentially affect the in vitro translation of a reporter gene". American Journal of Physiology. Lung Cellular and Molecular Physiology. 299 (4): L523–34. doi:10.1152/ajplung.00113.2010. PMC 2957414. PMID 20693318.
- ^ Wang G, Guo X, Floros J (Sep 2005). "Differences in the translation efficiency and mRNA stability mediated by 5'-UTR splice variants of human SP-A1 and SP-A2 genes". American Journal of Physiology. Lung Cellular and Molecular Physiology. 289 (3): L497–508. doi:10.1152/ajplung.00100.2005. PMID 15894557.
- ^ Wang G, Guo X, Floros J (May 2003). "Human SP-A 3'-UTR variants mediate differential gene expression in basal levels and in response to dexamethasone". American Journal of Physiology. Lung Cellular and Molecular Physiology. 284 (5): L738–48. doi:10.1152/ajplung.00375.2002. PMID 12676764. S2CID 13268207.
- ^ Bruce SR, Atkins CL, Colasurdo GN, Alcorn JL (Oct 2009). "Respiratory syncytial virus infection alters surfactant protein A expression in human pulmonary epithelial cells by reducing translation efficiency". American Journal of Physiology. Lung Cellular and Molecular Physiology. 297 (4): L559–67. doi:10.1152/ajplung.90507.2008. PMC 2770795. PMID 19525387.
Further reading
[edit]- Lu J (Jun 1997). "Collectins: collectors of microorganisms for the innate immune system". BioEssays. 19 (6): 509–18. doi:10.1002/bies.950190610. PMID 9204768. S2CID 23565862.
- Floros J, Hoover RR (Nov 1998). "Genetics of the hydrophilic surfactant proteins A and D". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1408 (2–3): 312–22. doi:10.1016/S0925-4439(98)00077-5. PMID 9813381.
- Khubchandani KR, Snyder JM (Jan 2001). "Surfactant protein A (SP-A): the alveolus and beyond". FASEB Journal. 15 (1): 59–69. CiteSeerX 10.1.1.326.5508. doi:10.1096/fj.00-0318rev. PMID 11149893. S2CID 1934315.
- Katyal SL, Singh G, Locker J (Apr 1992). "Characterization of a second human pulmonary surfactant-associated protein SP-A gene". American Journal of Respiratory Cell and Molecular Biology. 6 (4): 446–52. doi:10.1165/ajrcmb/6.4.446. PMID 1372511.
- Childs RA, Wright JR, Ross GF, Yuen CT, Lawson AM, Chai W, Drickamer K, Feizi T (May 1992). "Specificity of lung surfactant protein SP-A for both the carbohydrate and the lipid moieties of certain neutral glycolipids". The Journal of Biological Chemistry. 267 (14): 9972–9. doi:10.1016/S0021-9258(19)50187-9. PMID 1577827.
- Endo H, Oka T (Jun 1991). "An immunohistochemical study of bronchial cells producing surfactant protein A in the developing human fetal lung". Early Human Development. 25 (3): 149–56. doi:10.1016/0378-3782(91)90111-F. PMID 1935736.
- Voss T, Melchers K, Scheirle G, Schäfer KP (Jan 1991). "Structural comparison of recombinant pulmonary surfactant protein SP-A derived from two human coding sequences: implications for the chain composition of natural human SP-A". American Journal of Respiratory Cell and Molecular Biology. 4 (1): 88–94. doi:10.1165/ajrcmb/4.1.88. PMID 1986781.
- Haagsman HP, White RT, Schilling J, Lau K, Benson BJ, Golden J, Hawgood S, Clements JA (Dec 1989). "Studies of the structure of lung surfactant protein SP-A". The American Journal of Physiology. 257 (6 Pt 1): L421–9. doi:10.1152/ajplung.1989.257.6.L421. PMID 2610270.
- Fisher JH, Kao FT, Jones C, White RT, Benson BJ, Mason RJ (Jun 1987). "The coding sequence for the 32,000-dalton pulmonary surfactant-associated protein A is located on chromosome 10 and identifies two separate restriction-fragment-length polymorphisms". American Journal of Human Genetics. 40 (6): 503–11. PMC 1684155. PMID 2884868.
- White RT, Damm D, Miller J, Spratt K, Schilling J, Hawgood S, Benson B, Cordell B (1985). "Isolation and characterization of the human pulmonary surfactant apoprotein gene". Nature. 317 (6035): 361–3. Bibcode:1985Natur.317..361W. doi:10.1038/317361a0. PMID 2995821. S2CID 4357498.
- Floros J, Steinbrink R, Jacobs K, Phelps D, Kriz R, Recny M, Sultzman L, Jones S, Taeusch HW, Frank HA (Jul 1986). "Isolation and characterization of cDNA clones for the 35-kDa pulmonary surfactant-associated protein". The Journal of Biological Chemistry. 261 (19): 9029–33. doi:10.1016/S0021-9258(19)84483-6. PMID 3755136.
- Schaeffer E, Guillou F, Part D, Zakin MM (Nov 1993). "A different combination of transcription factors modulates the expression of the human transferrin promoter in liver and Sertoli cells". The Journal of Biological Chemistry. 268 (31): 23399–408. doi:10.1016/S0021-9258(19)49476-3. PMID 8226864.
- Khoor A, Gray ME, Hull WM, Whitsett JA, Stahlman MT (Sep 1993). "Developmental expression of SP-A and SP-A mRNA in the proximal and distal respiratory epithelium in the human fetus and newborn". The Journal of Histochemistry and Cytochemistry. 41 (9): 1311–9. doi:10.1177/41.9.8354874. PMID 8354874.
- Strayer DS, Yang S, Jerng HH (Sep 1993). "Surfactant protein A-binding proteins. Characterization and structures". The Journal of Biological Chemistry. 268 (25): 18679–84. doi:10.1016/S0021-9258(17)46683-X. PMID 8360162.
- Kölble K, Lu J, Mole SE, Kaluz S, Reid KB (Aug 1993). "Assignment of the human pulmonary surfactant protein D gene (SFTP4) to 10q22-q23 close to the surfactant protein A gene cluster". Genomics. 17 (2): 294–8. doi:10.1006/geno.1993.1324. PMID 8406480.
- deMello DE, Heyman S, Phelps DS, Floros J (May 1993). "Immunogold localization of SP-A in lungs of infants dying from respiratory distress syndrome". The American Journal of Pathology. 142 (5): 1631–40. PMC 1886897. PMID 8494055.
- Chroneos ZC, Abdolrasulnia R, Whitsett JA, Rice WR, Shepherd VL (Jul 1996). "Purification of a cell-surface receptor for surfactant protein A". The Journal of Biological Chemistry. 271 (27): 16375–83. doi:10.1074/jbc.271.27.16375. PMID 8663107.
- Planer BC, Ning Y, Kumar SA, Ballard PL (Aug 1997). "Transcriptional regulation of surfactant proteins SP-A and SP-B by phorbol ester". Biochimica et Biophysica Acta (BBA) - Gene Structure and Expression. 1353 (2): 171–9. doi:10.1016/S0167-4781(97)00070-5. PMID 9294011.