Patent ductus arteriosus: Difference between revisions
| Line 55: | Line 55: | ||
Neonates without adverse symptoms may simply be monitored as [[outpatient]]s, while symptomatic PDA can be treated with both [[surgery|surgical]] and nonsurgical methods.<ref>Zahaka, KG and Patel, CR. "Congenital defects'". Fanaroff, AA and Martin, RJ (eds.). ''Neonatal-perinatal medicine: Diseases of the fetus and infant.'' 7th ed. (2002):1120-1139. St. Louis: Mosby.</ref> Surgically, the DA may be closed by ligation (though support in premature infants is mixed),<ref name="pmid20808624">{{cite journal |author=Mosalli R, Alfaleh K, Paes B |title=Role of prophylactic surgical ligation of patent ductus arteriosus in extremely low birth weight infants: Systematic review and implications for clinical practice |journal=Ann Pediatr Cardiol |volume=2 |issue=2 |pages=120–6 |date=July 2009 |pmid=20808624 |pmc=2922659 |doi=10.4103/0974-2069.58313 |url=http://www.annalspc.com/article.asp?issn=0974-2069;year=2009;volume=2;issue=2;spage=120;epage=126;aulast=Mosalli}}</ref> wherein the DA is manually tied shut, or with intravascular coils or plugs that leads to formation of a thrombus in the DA. |
Neonates without adverse symptoms may simply be monitored as [[outpatient]]s, while symptomatic PDA can be treated with both [[surgery|surgical]] and nonsurgical methods.<ref>Zahaka, KG and Patel, CR. "Congenital defects'". Fanaroff, AA and Martin, RJ (eds.). ''Neonatal-perinatal medicine: Diseases of the fetus and infant.'' 7th ed. (2002):1120-1139. St. Louis: Mosby.</ref> Surgically, the DA may be closed by ligation (though support in premature infants is mixed),<ref name="pmid20808624">{{cite journal |author=Mosalli R, Alfaleh K, Paes B |title=Role of prophylactic surgical ligation of patent ductus arteriosus in extremely low birth weight infants: Systematic review and implications for clinical practice |journal=Ann Pediatr Cardiol |volume=2 |issue=2 |pages=120–6 |date=July 2009 |pmid=20808624 |pmc=2922659 |doi=10.4103/0974-2069.58313 |url=http://www.annalspc.com/article.asp?issn=0974-2069;year=2009;volume=2;issue=2;spage=120;epage=126;aulast=Mosalli}}</ref> wherein the DA is manually tied shut, or with intravascular coils or plugs that leads to formation of a thrombus in the DA. |
||
Because [[prostaglandin E1]] is responsible for keeping the ductus patent, [[NSAIDS]] (inhibitors of prostaglandin synthesis) such as [[indomethacin]] or a special form of [[ibuprofen]] have been used to help close a PDA.<ref name=medlineplus/><ref>[http://www.mayoclinic.com/health/patent-ductus-arteriosus/DS00631/DSECTION=treatments-and-drugs MayoClinic > Patent ductus arteriosus (PDA) ] Dec. 22, 2009</ref> This is an especially viable alternative for premature infants.{{Citation needed|date=April 2010}} |
Because [[prostaglandin E1]] is responsible for keeping the ductus patent, [[NSAIDS]] (inhibitors of prostaglandin synthesis) such as [[indomethacin]] or a special form of [[ibuprofen]] have been used to help close a PDA.<ref name=medlineplus/><ref>[http://www.mayoclinic.com/health/patent-ductus-arteriosus/DS00631/DSECTION=treatments-and-drugs MayoClinic > Patent ductus arteriosus (PDA) ] Dec. 22, 2009</ref> This is an especially viable alternative for premature infants.{{Citation needed|date=April 2010}}. Recent findings from a systematic review concluded that for closure of PDA in preterm and or low birth weight infants, Ibuprofen is as effective as Indomethacin and is the preferred drug of choice currently .It also causes fewer side effects such as transient renal insufficiency and reduces the risk of necrotising enterocolitis. <ref>{{Cite journal | author = Ohlsson A, Walia R, Shah SS . | title=Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants. | journal = Cochrane Database Syst Rev | issue = 2 | pages = CD003481| year = 2015 | doi = 10.1002/14651858.CD003481.pub6}}</ref> |
||
In certain cases, it may be beneficial to the neonate to prevent closure of the ductus arteriosus.{{Citation needed|date=April 2010}} For example, in [[transposition of the great vessels]], a PDA may prolong the newborn's life until surgical correction is possible. The ductus arteriosus can be induced to remain open by administering [[prostaglandin]] analogs such as [[alprostadil]] or [[misoprostol]] (prostaglandin E<sub>1 </sub> analogs){{Citation needed|date=April 2010}}. |
In certain cases, it may be beneficial to the neonate to prevent closure of the ductus arteriosus.{{Citation needed|date=April 2010}} For example, in [[transposition of the great vessels]], a PDA may prolong the newborn's life until surgical correction is possible. The ductus arteriosus can be induced to remain open by administering [[prostaglandin]] analogs such as [[alprostadil]] or [[misoprostol]] (prostaglandin E<sub>1 </sub> analogs){{Citation needed|date=April 2010}}. |
||
Revision as of 04:20, 24 February 2015
| Patent ductus arteriosus | |
|---|---|
| Specialty | Cardiology, pediatrics |
Patent ductus arteriosus (PDA) is a congenital disorder in the heart wherein a neonate's ductus arteriosus fails to close after birth. Early symptoms are uncommon, but in the first year of life include increased work of breathing and poor weight gain. With age, the PDA may lead to congestive heart failure if left uncorrected. The ductus arteriosus is a normal fetal blood vessel that closes soon after birth. In a PDA, the vessel does not close and remains "patent" (open) resulting in irregular transmission of blood between two of the most important arteries close to the heart, the aorta and the pulmonary artery. PDA is common in neonates with persistent respiratory problems such as hypoxia, and has a high occurrence in premature children. In hypoxic newborns, too little oxygen reaches the lungs to produce sufficient levels of bradykinin and subsequent closing of the DA. Premature children are more likely to be hypoxic and thus have PDA because of their underdeveloped heart and lungs.
A PDA allows a portion of the oxygenated blood from the left heart to flow back to the lungs by flowing from the aorta (which has higher pressure) to the pulmonary artery. If this shunt is substantial, the neonate becomes short of breath: the additional fluid returning to the lungs increases lung pressure to the point that the neonate has greater difficulty inflating the lungs. This uses more calories than normal and often interferes with feeding in infancy. This condition, as a constellation of findings, is called congestive heart failure.
In some cases, such as in transposition of the great vessels (the pulmonary artery and the aorta), a PDA may need to remain open. In this cardiovascular condition, the PDA is the only way that oxygenated blood can mix with deoxygenated blood. In these cases, prostaglandins are used to keep the DA open.
Signs and symptoms
While some cases of PDA are asymptomatic, common symptoms include:
- tachycardia
- respiratory problems
- dyspnea – shortness of breath
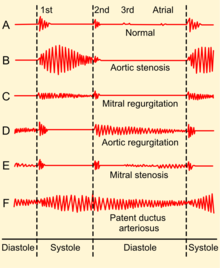
- continuous machine-like heart murmur (usually from aorta to pulmonary artery, with higher flow during systole and lower flow during diastole)
- cardiomegaly - enlarged heart, reflecting ventricular dilation and volume overload
- left subclavicular thrill
- bounding pulse
- widened pulse pressure
- Patients typically present in good health, with normal respirations and heart rate. If the ductus is moderate or large, widened pulse pressure and bounding peripheral pulses are frequently present, reflecting increased left ventricular stroke volume and diastolic runoff of blood into the initially lower-resistant pulmonary vascular bed. Prominent suprasternal and carotid pulsations may be noted secondary to increased left ventricular stroke volume.
- poor growth[1]
- differential cyanosis, i.e. cyanosis of the lower extremities but not of the upper body.
Adult PDA
Since PDA is usually identified in infants, it is less common in adults, but it can have serious consequences, and is usually corrected surgically if it is diagnosed.
Diagnosis
PDA is usually diagnosed using noninvasive techniques. Echocardiography, in which sound waves are used to capture the motion of the heart, and associated Doppler studies are the primary methods of detecting PDA. Electrocardiography (ECG), in which electrodes are used to record the electrical activity of the heart, is not particularly helpful as no specific rhythms or ECG patterns can be used to detect PDA.[citation needed]
A chest X-ray may be taken, which reveals the overall size of neonate's heart (as a reflection of the combined mass of the cardiac chambers) and the appearance of the blood flow to the lungs. A small PDA most often shows a normal-sized heart and normal blood flow to the lungs. A large PDA generally shows an enlarged cardiac silhouette and increased blood flow to the lungs.
Normal anatomy
In the developing fetus, the DA is the vascular connection between the pulmonary artery and the aortic arch that allows most of the blood from the right ventricle to bypass the fetus' fluid-filled compressed lungs. During fetal development, this shunt protects the right ventricle from pumping against the high resistance in the lungs, which can lead to right ventricular failure if the DA closes in utero.
When the newborn takes his or her first breath, the lungs open and pulmonary vascular resistance decreases. After birth, the lungs release bradykinin to constrict the smooth muscle wall of the DA and reduce bloodflow through the DA as it narrows and completely closes, usually within the first few weeks of life. In most newborns with a patent ductus arteriosus, the blood flow is reversed from that of in utero flow, i.e. the blood flow is from the higher-pressure aorta to the now lower-pressure pulmonary arteries.
In normal newborns, the DA is substantially closed within 12–24 hours after birth, and is completely sealed after three weeks. The primary stimulus for the closure of the ductus is the increase in neonatal blood oxygen content. Withdrawal from maternal circulating prostaglandins also contributes to ductal closure. The residual scar tissue from the fibrotic remnants of DA, called the ligamentum arteriosum, remains in the normal adult heart.
Treatment
Neonates without adverse symptoms may simply be monitored as outpatients, while symptomatic PDA can be treated with both surgical and nonsurgical methods.[2] Surgically, the DA may be closed by ligation (though support in premature infants is mixed),[3] wherein the DA is manually tied shut, or with intravascular coils or plugs that leads to formation of a thrombus in the DA.
Because prostaglandin E1 is responsible for keeping the ductus patent, NSAIDS (inhibitors of prostaglandin synthesis) such as indomethacin or a special form of ibuprofen have been used to help close a PDA.[1][4] This is an especially viable alternative for premature infants.[citation needed]. Recent findings from a systematic review concluded that for closure of PDA in preterm and or low birth weight infants, Ibuprofen is as effective as Indomethacin and is the preferred drug of choice currently .It also causes fewer side effects such as transient renal insufficiency and reduces the risk of necrotising enterocolitis. [5]
In certain cases, it may be beneficial to the neonate to prevent closure of the ductus arteriosus.[citation needed] For example, in transposition of the great vessels, a PDA may prolong the newborn's life until surgical correction is possible. The ductus arteriosus can be induced to remain open by administering prostaglandin analogs such as alprostadil or misoprostol (prostaglandin E1 analogs)[citation needed].
More recently, PDAs can be closed by percutaneous interventional method.[citation needed] Via the femoral vein or femoral artery, a platinum coil can be deployed via a catheter, which induces thrombosis (coil embolization). Alternatively, a PDA occluder device (AGA Medical)[citation needed], composed of nitinol mesh, is deployed from the pulmonary artery through the PDA. The larger skirt of the device sits on the aortic side, while the ampulla of the device hugs the walls of the PDA, with care taken to avoid occlusion of the pulmonary arterial lumen by the device.[citation needed] These methods permit closure without open heart surgery.
Prevention
Some evidence suggests giving indomethacin on the first day of life, prophylactically to all preterm infants (less than 37 weeks gestation), reduces the risk of developing a PDA (relative risk 0.29 95% CI 0.22, 0.38) and the complications associated with PDA. The need is also decreased for surgical intervention to treat PDA in premature infants prophylactically treated with indomethacin (relative risk of 0.51 95%CI 0.37, 0.71). Complications of PDA include intraventricular hemorrhage which can lead to severe brain damage. No evidence, however, shows giving indomethacin prophylactically improves survival for these infants (RR 0.96; 95% CI 0.81, 1.12). Also no significant evidence suggests prophylactic indomethacin decreases long-term disability (cerebral palsy, visual impairment, hearing impairment, decreased cognitive performance) rates.[6]
Etiology
A PDA can be idiopathic (i.e. without an identifiable cause), or secondary to another condition. Some common contributing factors in humans include:
- Preterm birth
- Congenital rubella syndrome
- Chromosomal abnormalities such as Down syndrome
Prognosis
Without treatments, the disease may progress from left-to-right (noncyanotic heart) shunt to right-to-left shunt (cyanotic heart) called Eisenmenger's syndrome. Also, a long-term effect would be pulmonary hypertension, which can lead to needing a heart and/or lung transplant.
History
Robert E. Gross, MD performed the first successful ligation of a patent ductus arteriosus on an eight-year-old girl at Children's Hospital Boston in 1938.[citation needed]
Additional images
-
Illustration of Patent Ductus Arteriosus
-
Patent ductus arteriosus
-
An echocardiogram of a stented persisting ductus arteriosus: One can see the aortic arch and the stent leaving. The pulmonary artery is not seen.
-
An echocardiogram of a coiled persisting ductus arteriosus: One can see the aortic arch, the pulmonary artery, and the coil between them.
References
- ^ a b MedlinePlus > Patent ductus arteriosus Update Date: 21 December 2009
- ^ Zahaka, KG and Patel, CR. "Congenital defects'". Fanaroff, AA and Martin, RJ (eds.). Neonatal-perinatal medicine: Diseases of the fetus and infant. 7th ed. (2002):1120-1139. St. Louis: Mosby.
- ^ Mosalli R, Alfaleh K, Paes B (July 2009). "Role of prophylactic surgical ligation of patent ductus arteriosus in extremely low birth weight infants: Systematic review and implications for clinical practice". Ann Pediatr Cardiol. 2 (2): 120–6. doi:10.4103/0974-2069.58313. PMC 2922659. PMID 20808624.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ MayoClinic > Patent ductus arteriosus (PDA) Dec. 22, 2009
- ^ Ohlsson A, Walia R, Shah SS . (2015). "Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants". Cochrane Database Syst Rev (2): CD003481. doi:10.1002/14651858.CD003481.pub6.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fowlie, PW; Davis PG; McGuire W (19 May 2010). "Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants (Review)". The Cochrane Database of Systematic Reviews (7): CD000174. doi:10.1002/14651858.CD000174.pub2.
^ Long-term Neurological Outcomes Following Neonatal Heart Surgery: Implications for Cerebral Protections in Adults. Sandra Bellezza MD. March 2, 2011
External links
- Patent Ductus Arteriosus (PDA) - Stanford Children's Health
- Patent Ductus Arteriosus information from Seattle Children's Hospital Heart Center
- Patent Ductus Arteriosus Causes from US Department of Health and Human Services
- Patent Ductus Arteriosus from Merck
- Fetal Circulation at berkeley.edu
- Information about PDA - The Hospital for Sick Children
- Down's Heart Group Easy to understand diagram and explanation of PDA.
- PDA Occluder Amplatzer PDA occluder device used for percutaneous closure of PDAs.
- Children's Hospital Boston Archives
- Patent ductus arteriosus information for parents.




