Benign prostatic hyperplasia
| Benign prostatic hyperplasia | |
|---|---|
| Specialty | Urology |
Benign prostatic hyperplasia (BPH), also called benign enlargement of the prostate (BEP), adenofibromyomatous hyperplasia and benign prostatic hypertrophy (technically incorrect usage), is a benign increase in size of the prostate.
BPH involves hyperplasia of prostatic stromal and epithelial cells, resulting in the formation of large, fairly discrete nodules in the periurethral region of the prostate. When sufficiently large, the nodules compress the urethral canal to cause partial, or sometimes virtually complete, urinary tract obstruction by the urethra, which interferes with the normal flow of urine. It leads to symptoms of urinary hesitancy, frequent urination, increased risk of urinary tract infections, urinary retention, or contribute to or cause insomnia. Although prostate specific antigen levels may be elevated in these patients because of increased organ volume and inflammation due to urinary tract infections, BPH does not lead to cancer or increase the risk of cancer.[1]
BPH involves hyperplasia (an increase in the number of cells) rather than hypertrophy (a growth in the size of individual cells), but the two terms are often used interchangeably, even amongst urologists.[2]
Adenomatous prostatic growth is believed to begin at approximately age 30 years. An estimated 50% of men have histologic evidence of BPH by age 50 years and 75% by age 80 years; in 40–50% of these men, BPH becomes clinically significant.[3]
Signs and symptoms
Benign prostatic hyperplasia symptoms are classified as storage or voiding.
Storage symptoms include urinary frequency, urgency (compelling need to void that cannot be deferred), urgency incontinence, and voiding at night (nocturia).
Voiding symptoms include urinary stream hesitancy (needing to wait for the stream to begin), intermittency (when the stream starts and stops intermittently), straining to void, and dribbling. Pain and dysuria are usually not present. These storage and voiding symptoms are evaluated using the International Prostate Symptom Score (IPSS) questionnaire, designed to assess the severity of BPH.[4]
BPH can be a progressive disease, especially if left untreated. Incomplete voiding results in stasis of bacteria in the bladder residue and an increased risk of urinary tract infection. Urinary bladder stones are formed from the crystallization of salts in the residual urine. Urinary retention, termed acute or chronic, is another form of progression. Acute urinary retention is the inability to void, while in chronic urinary retention the residual urinary volume gradually increases, and the bladder distends. This can result in bladder hypotonia. Some patients who suffer from chronic urinary retention may eventually progress to renal failure, a condition termed obstructive uropathy.
Causes
Most experts consider androgens (testosterone and related hormones) to play a permissive role. This means that androgens have to be present for BPH to occur, but do not necessarily directly cause the condition. This is supported by the fact that castrated boys do not develop BPH when they age. On the other hand, administering exogenous testosterone is not associated with a significant increase in the risk of BPH symptoms.[citation needed] Dihydrotestosterone (DHT), a metabolite of testosterone, is a critical mediator of prostatic growth. DHT is synthesized in the prostate from circulating testosterone by the action of the enzyme 5α-reductase, type 2. This enzyme is localized principally in the stromal cells; hence, those cells are the main site for the synthesis of DHT.
DHT can act in an autocrine fashion on the stromal cells or in paracrine fashion by diffusing into nearby epithelial cells. In both of these cell types, DHT binds to nuclear androgen receptors and signals the transcription of growth factors that are mitogenic to the epithelial and stromal cells. DHT is 10 times more potent than testosterone because it dissociates from the androgen receptor more slowly. The importance of DHT in causing nodular hyperplasia is supported by clinical observations in which an inhibitor of 5α-reductase such as finasteride is given to men with this condition. Therapy with a 5α-reductase inhibitor markedly reduces the DHT content of the prostate and, in turn, reduces prostate volume and, in many cases, BPH symptoms.[citation needed]
Testosterone promotes prostate cell proliferation,[5] but relatively low levels of serum testosterone are found in patients with BPH.[6][7] One small study has shown that medical castration lowers the serum and prostate hormone levels unevenly, having less effect on testosterone and dihydrotestosterone levels in the prostate.[8]
While there is some evidence that estrogen may play a role in the etiology of BPH, this effect appears to be mediated mainly through local conversion of androgens to estrogen in the prostate tissue rather than a direct effect of estrogen itself.[9] In canine in vivo studies castration, which significantly reduced androgen levels but left estrogen levels unchanged, caused significant atrophy of the prostate.[10] Studies looking for a correlation between prostatic hyperplasia and serum estrogen levels in humans have generally shown none.[7][11]
In 2008, Yigal Gat et al. published evidence that BPH is caused by failure in the spermatic venous drainage system resulting in increased hydrostatic pressure and local testosterone levels elevated more than 100 fold above serum levels.[12] If confirmed, this mechanism explains why serum androgen levels do not seem to correlate with BPH and why giving exogenous testosterone would not make much difference. This also has implications for treatment (see Minimally invasive therapies below).
On a microscopic level, BPH can be seen in the vast majority of men as they age, in particular over the age of 70 years, around the world. However, rates of clinically significant, symptomatic BPH vary dramatically depending on lifestyle. Men who lead a western lifestyle have a much higher incidence of symptomatic BPH than men who lead a traditional or rural lifestyle. This is supported by research[citation needed] in China showing that men in rural areas have very low rates of clinical BPH, while men living in cities adopting a western lifestyle have a skyrocketing incidence of this condition, though it is still below rates seen in the West. It also seems[citation needed] that there is some connection between microcalcifications between prostate cancer and BPH, as is demonstrated in 50-75% of men over 50 years.[clarification needed]
Pathophysiology
Both the glandular epithelial cells and the stromal cells (including muscular fibers) undergo hyperplasia in BPH.[13]:694 Most sources agree that of the two tissues, stromal hyperplasia predominates, but the exact ratio of the two is unclear.[13]:694
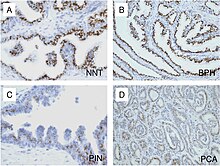
Anatomically, BPH is most strongly associated with the posterior urethral glands (PUG) and transitional zone (TZ) of the prostate. The earliest microscopic signs of BPH usually begin between the age of 30 and 50 years old in the PUG, which are posterior to the proximal urethra.[13]:694 In BPH, the majority of growth occurs in the TZ.[13]:694 In addition to these two classic areas, the peripheral zone (PZ) of the prostate is also involved to a lesser extent.[13]:695 Prostatic cancer typically occurs in the PZ. However, BPH nodules, usually from the TZ are often biopsied anyway to rule out cancer in the TZ.[13]:695 However, cancers of the prostate most frequently occur in the PZ rather than the TZ, thus, chippings taken from the PZ are of limited use.
Diagnosis


Rectal examination (palpation of the prostate through the rectum) may reveal a markedly enlarged prostate, usually affecting the middle lobe.
Often, blood tests are performed to rule out prostatic malignancy: Elevated prostate specific antigen (PSA) levels needs further investigations such as reinterpretation of PSA results, in terms of PSA density and PSA free percentage, rectal examination and transrectal ultrasonography. These combined measures can provide early detection.
Ultrasound examination of the testicles, prostate, and kidneys is often performed, again to rule out malignancy and hydronephrosis.
Screening and diagnostic procedures for BPH are similar to those used for prostate cancer. Some signs to look for include:[14]
- Weak urinary stream
- Prolonged emptying of the bladder
- Abdominal straining
- Hesitancy
- Irregular need to urinate
- Incomplete bladder emptying
- Post-urination dribble
- Irritation during urination
- Frequent urination
- Nocturia (need to urinate during the night)
- Urgency
- Incontinence (involuntary leakage of urine)
- Bladder pain
- Dysuria (painful urination)
- Problems in ejaculation
Management
Lifestyle
Lifestyle alterations to address the symptoms of BPH include decreasing fluid intake before bedtime, moderating the consumption of alcohol and caffeine-containing products, and following a timed voiding schedule. Patients can also attempt to avoid products and medications that may exacerbate symptoms of BPH, including antihistamines, diuretics, and decongestants, opiates, and tricyclic antidepressants, however this should be done with input from a medical professional.[15]
Medications
The two main medications for management of BPH are alpha blockers and 5α-reductase inhibitors.
Alpha blockers (technically α1-adrenergic receptor antagonists) are the most common choice for initial therapy in the USA[16][17] and Europe.[18] Alpha blockers used for BPH include doxazosin,[19] terazosin, alfuzosin,[20][21] tamsulosin, and silodosin. All five are equally effective but have slightly different side effect profiles.[22] The older drugs phenoxybenzamine and prazosin are not recommended.[23] Alpha blockers relax smooth muscle in the prostate and the bladder neck, thus decreasing the blockage of urine flow. Common side effects of alpha blockers include orthostatic hypotension, (a head rush or dizzy spell when standing up or stretching), ejaculation changes, headaches, nasal congestion, and weakness. Non-selective alpha blockers such as Terazosin and Doxazosin may also require titration as they can cause syncope if the dose is too high. Side effects can also include erectile dysfunction.[24]
The 5α-reductase inhibitors finasteride[25] and dutasteride[26] are another treatment option. These medications inhibit 5a-reductase, which in turn inhibits production of DHT, a hormone responsible for enlarging the prostate. Effects may take longer to appear than alpha blockers, but they persist for many years.[27] When used together with alpha blockers, a reduction of BPH progression to acute urinary retention and surgery has been noted in patients with larger prostates.[28] Side effects include decreased libido and ejaculatory or erectile dysfunction.[25]
Antimuscarinics such as tolterodine may also be used, especially in combination with alpha blockers.[29] They act by decreasing acetylcholine effects on the smooth muscle of the bladder, thus helping control symptoms of an overactive bladder.[citation needed]
In 2011, the U.S. Food and Drug Administration approved Cialis (tadalafil) to treat the signs and symptoms of benign prostatic hyperplasia (BPH), and for the treatment of BPH and erectile dysfunction (ED), when the conditions occur simultaneously.[30] Cialis was approved in 2003 for the treatment of ED.[31]
Sildenafil citrate shows some symptomatic relief, suggesting a possible common etiology with erectile dysfunction.[32] Tadalafil was considered then rejected by NICE in the UK for the treatment of symptoms associated with BPH.[33]
Minimally invasive therapies
The European Urology Review[34] published in 2009 that two Israeli doctors, Yigal Gat and Menahem Goren, have developed the Gat-Goren nonsurgical method for BPH.[35] Using an interventional radiological technique that reduces prostate volume and reverses BPH symptoms, the treatment, known as super-selective intra-prostatic androgen deprivation (SPAD) therapy, involves a percutaneous venography and sclerotherapy of the internal spermatic vein network, including associated venous bypasses and retroperitoneal collaterals. The European Urology Review also declared that using the Gat Goren nonsurgical method results in decreased prostate volume, which leads to significantly decreased nocturia, improved urine stream, and also improves emptying of the urinary bladder, and that without the potential side effects and complications of the classic surgery.
Although medication is often prescribed as the first treatment option, there are many patients who do not achieve success with this line of treatment. Those patients may not achieve sustained improvement in symptoms or they may stop taking the medication because of side-effects.[36] There are options for treatment in a urologist's office before proceeding to surgery. The two most common types of office-based therapies are transurethral microwave thermotherapy (TUMT) and transurethral needle ablation (TUNA). Both of these procedures rely on delivering enough energy to create sufficient heat to cause cell death (necrosis) in the prostate. The goal of the therapies is to cause enough necrosis so that, when the dead tissue is reabsorbed by the body, the prostate shrinks, relieving the obstruction of the urethra. These procedures are typically performed with local anesthesia, and the patient returns home the same day. Some urologists have studied and published long-term data on the outcomes of these procedures, with data out to five years. The most recent American Urological Association (AUA) Guidelines for the Treatment of BPH in 2003 lists minimally invasive therapies including TUMT and TUNA as acceptable alternatives for certain patients with BPH.[37]
Transurethral microwave therapy (TUMT) was originally approved by the United States Food and Drug Administration (FDA) in 1996, with the first generation system by EDAP Technomed. Since 1996, other companies have received FDA approval for TUMT devices, including Urologix, Dornier, Thermatrix, Celsion, and Prostalund. Multiple clinical studies have been published on TUMT. The general principle underlying all the devices is that a microwave antenna that resides in a urethral catheter is placed in the intraprostatic area of the urethra. The catheter is connected to a control box outside of the patient's body and is energized to emit microwave radiation into the prostate to heat the tissue and cause necrosis. It is a one-time treatment that takes approximately 30 minutes to 1 hour, depending on the system used. It takes approximately 4 to 6 weeks for the damaged tissue to be reabsorbed into the patient's body. Some of the devices incorporate circulating coolant through the treatment area with the intent of preserving the urethra while the microwave energy heats the prostatic tissue surrounding the urethra.
Transurethral needle ablation (TUNA) operates with a different type of energy, radio frequency (RF) energy, but is designed along the same premise as TUMT devices, that the heat the device generates will cause necrosis of the prostatic tissue and shrink the prostate. The TUNA device is inserted into the urethra using a rigid scope much like a cystoscope. The energy is delivered into the prostate using two needles that emerge from the sides of the device, through the urethral wall and into the prostate. The needle-based ablation devices are very effective at heating a localized area to a high enough temperature to cause necrosis. The treatment is typically performed in one session, but may require multiple sticks of the needles depending on the size of the prostate.
Surgery
If medical treatment fails, and the patient elects not to try office-based therapies or the physician determines the patient is a better candidate for transurethral resection of prostate (TURP), surgery may need to be performed. In general, TURP is still considered the gold standard of prostate interventions for patients who require a procedure. This involves removing (part of) the prostate through the urethra. However after this endscopic surgery the ejaculations are dry and the person becomes sterile. For a male who wishes to father a child this is not the procedure of choice. Over the past couple of decades efforts to find newer surgical methods have resulted in newer approaches and different types of energies being used to treat the enlarged gland. However some of the newer methods for reducing the size of an enlarged prostate, have not been around long enough to fully establish their safety or side-effects. These include various methods to destroy or remove part of the excess tissue while trying to avoid damaging what remains. Transurethral electrovaporization of the prostate (TVP), laser TURP, visual laser ablation (VLAP), ethanol injection, and others are studied as alternatives.
Newer techniques involving lasers in urology have emerged in the last 5–10 years, starting with the VLAP technique involving the Nd:YAG laser with contact on the prostatic tissue. A similar technology called Photoselective Vaporization of the Prostate (PVP) with the GreenLight (KTP or LBO crystal) laser have emerged very recently. This procedure involves a high-power 180-watt 532 nm wavelength laser with a 650-micrometre laser fiber inserted into the prostate. This fiber has an internal reflection with a 70-degree deflecting angle. It is used to vaporize the tissue to the prostatic capsule. GreenLight 532 nm lasers target haemoglobin as the chromophore and typically have a penetration depth of 0.8mm (two times deeper than holmium).
Another procedure termed Holmium Laser Ablation of the Prostate (HoLAP) has also been gaining acceptance around the world. Like KTP, the delivery device for HoLAP procedures is a 550 um disposable side-firing fiber that directs the beam from a high-power 100-watt laser at a 70-degree angle from the fiber axis. The holmium wavelength is 2,140 nm, which falls within the infrared portion of the spectrum and is invisible to the naked eye. Whereas GreenLight relies on haemoglobin as a chromophore, water within the target tissue is the chromophore for Holmium lasers. The penetration depth of Holmium lasers is <0.4 mm, avoiding complications associated with tissue necrosis often found with the deeper penetration and lower peak powers of Nd:YAG lasers used in the 1990s.
HoLEP, Holmium Laser Enucleation of the Prostate, is another Holmium laser procedure reported to carry fewer risks compared with either TURP or open prostatectomy.[38] HoLEP is largely similar to the HoLAP procedure; the main difference is that this procedure is typically performed on larger prostates. Instead of ablating the tissue, the laser cuts a portion of the prostate, which is then cut into smaller pieces and flushed with irrigation fluid. As with the HoLAP procedure, there is little bleeding during or after the procedure.
Both wavelengths, GreenLight and Holmium, ablate approximately one to two grams of tissue per minute.
Post surgery care often involves placement of a Foley catheter or a temporary prostatic stent to permit healing and allow urine to drain from the bladder.
In summary, the surgical techniques used are:
- Open prostatectomy: not usually performed nowadays, even if results are very good.
- Trans-urethral resection of the prostate (TURP): the gold standard.
- Transurethral incision of the prostate (TUIP): rarely performed; the technique is similar to TURP but less definitive.
- Laser vaporization of the prostate: common treatment.
- Transurethral microwave therapy (TUMT): similar to laser ablation, but less effective and much less used.
- Transurethral needle ablation (TUNA): not very effective.
- Holmium laser enucleation of the prostate (HoLEP): more and more used, it will probably replace TURP in the future.
Alternative medicine
Herbal remedies are a commonly sought treatment for BPH,[39] and several are approved in European countries, and available in the USA. Saw palmetto extract from Serenoa repens is one of the most commonly used and studied, having showed some promise in early studies.[40] Later trials of higher methodological quality have shown it to be no better than placebo in both symptom relief and decreasing prostate size.[41][42][43]
Other herbal medicines include beta-sitosterol[44] from Hypoxis rooperi (African star grass) and pygeum (extracted from the bark of Prunus africana),[45] while there is less substantial support for the efficacy of pumpkin seed (Cucurbita pepo) and stinging nettle (Urtica dioica) root.[46]
Epidemiology

Globally, benign prostatic hyperplasia affects about 210 million males as of 2010 (6% of the population).[48] The prostate gets larger in most men as they get older. For a symptom-free man of 46 years, the risk of developing BPH over the next 30 years is 45%. Incidence rates increase from 3 cases per 1000 man-years at age 45–49 years, to 38 cases per 1000 man-years by the age of 75–79 years. While the prevalence rate is 2.7% for men aged 45–49, it increases to 24% by the age of 80 years.[49]
References
- ^ http://www.ncbi.nlm.nih.gov/pubmed/22792684
- ^ Bostwick, D. G. (2002). "The Pathology of Benign Prostatic Hyperplasia". In Kirby, Roger S.; McConnell, John D.; Fitzpatrick, John M.; Roehrborn, Claus G.; Boyle, Peter (eds.). Textbook of Benign Prostatic Hyperplasia. London: Isis Medical Media. ISBN 978-1-901865-55-4.[page needed]
- ^ Rubenstein, Jonathan; McVary, Kevin T. (6 February 2008). "Transurethral Microwave Thermotherapy of the Prostate (TUMT)". eMedicine.
- ^ Barry MJ, Fowler FJ, O'Leary MP; et al. (November 1992). "The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association". The Journal of Urology. 148 (5): 1549–57, discussion 1564. PMID 1279218.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Feldman, Brian J.; Feldman, David (2001). "The development of androgen-independent prostate cancer". Nature Reviews Cancer. 1 (1): 34–45. doi:10.1038/35094009. PMID 11900250.
- ^ Lagiou, Pagona; Mantzoros, Christos S.; Tzonou, Anastasia; Signorello, Lisa B.; Lipworth, Loren; Trichopoubs, Dimitrios (1997). "Serum Steroids in Relation to Benign Prostatic Hyperplasia". Oncology. 54 (6): 497–501. doi:10.1159/000227609. PMID 9394847.
- ^ a b Roberts, Rosebud O.; Jacobson, Debra J.; Rhodes, Thomas; Klee, George G.; Leiber, Michael M.; Jacobsen, Steven J. (2004). "Serum sex hormones and measures of benign prostatic hyperplasia". The Prostate. 61 (2): 124–31. doi:10.1002/pros.20080. PMID 15305335.
- ^ Page, S. T.; Lin, D. W.; Mostaghel, E. A.; Hess, D. L.; True, L. D.; Amory, J. K.; Nelson, P. S.; Matsumoto, A. M.; Bremner, W. J. (2006). "Persistent Intraprostatic Androgen Concentrations after Medical Castration in Healthy Men". Journal of Clinical Endocrinology & Metabolism. 91 (10): 3850–6. doi:10.1210/jc.2006-0968. PMID 16882745.
{{cite journal}}: Invalid|display-authors=9(help) - ^ Ho, C. K M; Nanda, J.; Chapman, K. E; Habib, F. K (2008). "Oestrogen and benign prostatic hyperplasia: effects on stromal cell proliferation and local formation from androgen". Journal of Endocrinology. 197 (3): 483–91. doi:10.1677/JOE-07-0470. PMID 18492814.
- ^ Niu, YJ; Ma, TX; Zhang, J; Xu, Y; Han, RF; Sun, G (2003). "Androgen and prostatic stroma". Asian journal of andrology. 5 (1): 19–26. PMID 12646998.
- ^ Ansari, Mohammad Abduljalil; Begum, Dilruba; Islam, Fakhrul (2008). "Serum sex steroids, gonadotrophins and sex hormone-binding globulin in prostatic hyperplasia". Annals of Saudi Medicine. 28 (3): 174–8. doi:10.4103/0256-4947.51727. PMID 18500180.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Gat, Y; Gornish, M; Heiblum, M; Joshua, S (2008). "Reversal of benign prostate hyperplasia by selective occlusion of impaired venous drainage in the male reproductive system: novel mechanism, new treatment". Andrologia. 40 (5): 273–281. doi:10.1111/j.1439-0272.2008.00883.x. PMID 18811916.
- ^ a b c d e f Wasserman, Neil F. (1 September 2006). "Benign Prostatic Hyperplasia: A Review and Ultrasound Classification". Radiologic Clinics of North America. 44 (5): 689–710. doi:10.1016/j.rcl.2006.07.005. PMID 17030221.
- ^ Janis, Craitlyn (19 May 2008). "A Brief Overview of Benign Prostatic Hyperplasia (BPH)". Associated Content.
{{cite web}}: Missing or empty|url=(help)[self-published source?][unreliable medical source?] - ^ "Benign prostatic hyperplasia". University of Maryland Medical Center.
- ^ Roehrborn, Claus G.; Nuckolls, James G.; Wei, John T.; Steers, William; BPH Registry and Patient Survey Steering Committee (2007). "The Benign Prostatic Hyperplasia Registry and Patient Survey: study design, methods and patient baseline characteristics". BJU International. 100 (4): 813–9. doi:10.1111/j.1464-410X.2007.07061.x. PMID 17822462.
- ^ Black, L; Naslund, MJ; Gilbert Jr, TD; Davis, EA; Ollendorf, DA (2006). "An examination of treatment patterns and costs of care among patients with benign prostatic hyperplasia". The American journal of managed care. 12 (4 Suppl): S99–S110. PMID 16551208.
- ^ Hutchison, A; Farmer, R; Verhamme, K; Berges, R; Navarrete, R (2007). "The Efficacy of Drugs for the Treatment of LUTS/BPH, A Study in 6 European Countries". European Urology. 51 (1): 207–15 discussion 215–6. doi:10.1016/j.eururo.2006.06.012. PMID 16846678.
- ^ MacDonald, Roderick; Wilt, Timothy J.; Howe, R. William (2004). "Doxazosin for treating lower urinary tract symptoms compatible with benign prostatic obstruction: a systematic review of efficacy and adverse effects". BJU International. 94 (9): 1263–70. doi:10.1111/j.1464-410X.2004.05154.x. PMID 15610102.
- ^ MacDonald, Roderick; Wilt, Timothy J. (2005). "Alfuzosin for treatment of lower urinary tract symptoms compatible with benign prostatic hyperplasia: A systematic review of efficacy and adverse effects". Urology. 66 (4): 780–8. doi:10.1016/j.urology.2005.05.001. PMID 16230138.
- ^ Roehrborn, Claus G (2001). "Efficacy and safety of once-daily alfuzosin in the treatment of lower urinary tract symptoms and clinical benign prostatic hyperplasia: a randomized, placebo-controlled trial". Urology. 58 (6): 953–9. doi:10.1016/S0090-4295(01)01448-0. PMID 11744466.
- ^ Djavan, Bob; Marberger, Michael (1999). "A Meta-Analysis on the Efficacy and Tolerability of α1-Adrenoceptor Antagonists in Patients with Lower Urinary Tract Symptoms Suggestive of Benign Prostatic Obstruction". European Urology. 36 (1): 1–13. doi:10.1159/000019919. PMID 10364649.
- ^ Aua Practice Guidelines, Committee (2003). "AUA Guideline on Management of Benign Prostatic Hyperplasia (2003). Chapter 1: Diagnosis and Treatment Recommendations". The Journal of Urology. 170 (2 Pt 1): 530–47. doi:10.1097/01.ju.0000078083.38675.79. PMID 12853821.
- ^ Santillo, VM; Lowe FC (2006). "Treatment of benign prostatic hyperplasia in patients with cardiovascular disease". Drugs and Aging. 10 (23): 795–805. PMID 17067183.
- ^ a b Gormley, Glenn J.; Stoner, Elizabeth; Bruskewitz, Reginald C.; Imperato-Mcginley, Julianne; Walsh, Patrick C.; McConnell, John D.; Andriole, Gerald L.; Geller, Jack; et al. (1992). "The Effect of Finasteride in Men with Benign Prostatic Hyperplasia". New England Journal of Medicine. 327 (17): 1185–91. doi:10.1056/NEJM199210223271701. PMID 1383816.
- ^ Roehrborn, C; Boyle, P; Nickel, JC; Hoefner, K; Andriole, G; ARIA3001 ARIA3002 and ARIA3003 Study Investigators (2002). "Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia". Urology. 60 (3): 434–41. doi:10.1016/S0090-4295(02)01905-2. PMID 12350480.
{{cite journal}}: CS1 maint: numeric names: authors list (link) - ^ Roehrborn, C; Bruskewitz, R; Nickel, J; McConnell, J; Saltzman, B; Gittelman, M; Malek, G; Gottesman, J; et al. (2004). "Sustained Decrease in Incidence of Acute Urinary Retention and Surgery With Finasteride for 6 Years in Men With Benign Prostatic Hyperplasia". The Journal of Urology. 171 (3): 1194–8. doi:10.1097/01.ju.0000112918.74410.94. PMID 14767299.
- ^ Kaplan, S; McConnell, J; Roehrborn, C; Meehan, A; Lee, M; Noble, W; Kusek, J; Nybergjr, L; Medical Therapy of Prostatic Symptoms (MTOPS) Research Group (2006). "Combination Therapy With Doxazosin and Finasteride for Benign Prostatic Hyperplasia in Patients With Lower Urinary Tract Symptoms and a Baseline Total Prostate Volume of 25 Ml or Greater". The Journal of Urology. 175 (1): 217–20, discussion 220–1. doi:10.1016/S0022-5347(05)00041-8. PMID 16406915.
{{cite journal}}: Invalid|display-authors=9(help) - ^ Kaplan, S. A.; Roehrborn, C. G.; Rovner, E. S.; Carlsson, M.; Bavendam, T.; Guan, Z. (2006). "Tolterodine and Tamsulosin for Treatment of Men With Lower Urinary Tract Symptoms and Overactive Bladder: A Randomized Controlled Trial". JAMA: the Journal of the American Medical Association. 296 (19): 2319–28. doi:10.1001/jama.296.19.2319. PMID 17105794.
- ^ "FDA approves Cialis to treat benign prostatic hyperplasia". U.S. Food and Drug Administration (FDA). Retrieved 7 May 2013.
- ^ "Drugs@FDA:FDA Approved Drug Products". U.S. Food and Drug Administration (FDA). Retrieved 7 May 2013.
- ^ McVary, Kevin T.; Monnig, William; Camps Jr., Joseph L.; Young, Jay M.; Tseng, Li-Jung; Van Den Ende, Gene (2007). "Sildenafil Citrate Improves Erectile Function and Urinary Symptoms in Men With Erectile Dysfunction and Lower Urinary Tract Symptoms Associated With Benign Prostatic Hyperplasia: A Randomized, Double-Blind Trial". The Journal of Urology. 177 (3): 1071–7. doi:10.1016/j.juro.2006.10.055. PMID 17296414.
- ^ "Hyperplasia (benign prostatic) - tadalafil (terminated appraisal) (TA273)". National Institute for Health and Clinical Excellence (NICE). Retrieved 27 January 2013.
- ^ Gat, Yigal; Gornish, Michael (2009). "Reversal of Benign Prostate Hyperplasia by Super-selective Intraprostatic Androgen Deprivation Therapy" (PDF). European Urology Review. Touch Briefings: 10–4.
- ^ www.prostata.co.il – The Gat Goren Method's official website
- ^ Roehrborn, CG (2008). "Current Medical Therapies for Men With Lower Urinary Tract Symptoms and Benign Prostatic Hyperplasia: Achievements and Limitations". Reviews in urology. 10 (1): 14–25. PMC 2312341. PMID 18470272.
- ^ AUA Clinical guidelines for management of BPH
- ^ Gilling, Peter J.; Aho, Tevita F.; Frampton, Christopher M.; King, Colleen J.; Fraundorfer, Mark R. (2008). "Holmium Laser Enucleation of the Prostate: Results at 6 Years". European Urology. 53 (4): 744–9. doi:10.1016/j.eururo.2007.04.052. PMID 17475395.
- ^ Lieber, M M (1998). "Pharmacologic therapy for prostatism". Mayo Clinic Proceedings. 73 (6): 590–6. doi:10.4065/73.6.590. PMID 9621869.
- ^ Boyle, P; Robertson, C; Lowe, F; Roehrborn, C (2000). "Meta-analysis of clinical trials of Permixon in the treatment of symptomatic benign prostatic hyperplasia". Urology. 55 (4): 533–9. doi:10.1016/S0090-4295(99)00593-2. PMID 10736497.
- ^ Bent, Stephen; Kane, Christopher; Shinohara, Katsuto; Neuhaus, John; Hudes, Esther S.; Goldberg, Harley; Avins, Andrew L. (2006). "Saw Palmetto for Benign Prostatic Hyperplasia". New England Journal of Medicine. 354 (6): 557–66. doi:10.1056/NEJMoa053085. PMID 16467543.
- ^ Dedhia, R; McVary, K (2008). "Phytotherapy for Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia". The Journal of Urology. 179 (6): 2119–25. doi:10.1016/j.juro.2008.01.094. PMID 18423748.
- ^ Tacklind, J; MacDonald, R; Rutks, I; Wilt, TJ (2009). Tacklind, James (ed.). "Serenoa repens for benign prostatic hyperplasia". Cochrane Database of Systematic Reviews (2): CD001423. doi:10.1002/14651858.CD001423.pub2. PMC 3090655. PMID 19370565.
- ^ Wilt, Timothy; Ishani, Areef; MacDonald, Roderick; Stark, Gerold; Mulrow, Cynthia D; Lau, Joseph; Wilt, Timothy (1999). Wilt, Timothy J (ed.). "Beta-sitosterols for benign prostatic hyperplasia". Cochrane Database of Systematic Reviews (2): CD001043. doi:10.1002/14651858.CD001043. PMID 10796740.
- ^ Wilt, Timothy; Ishani, Areef; Wilt, Timothy; Rutks, I; Stark, G (1998). Wilt, Timothy J (ed.). "Pygeum africanum for benign prostatic hyperplasia". Cochrane Database of Systematic Reviews (1): CD001044. doi:10.1002/14651858.CD001044. PMID 11869585.
- ^ Wilt, Timothy J; Ishani, Areef; Rutks, Indulis; MacDonald, Roderick (2007). "Phytotherapy for benign prostatic hyperplasia". Public Health Nutrition. 3 (4A): 459–72. doi:10.1017/S1368980000000549. PMID 11276294.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved 11 November 2009.
- ^ Vos, Theo; et al. (1 December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010". The Lancet. 380 (9859): 2163–2196. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
{{cite journal}}: Explicit use of et al. in:|author2=(help) - ^ Verhamme, K; Dieleman, JP; Bleumink, GS; Van Der Lei, J; Sturkenboom, MC; Artibani, W; Begaud, B; Berges, R; et al. (2002). "Incidence and Prevalence of Lower Urinary Tract Symptoms Suggestive of Benign Prostatic Hyperplasia in Primary Care—The Triumph Project". European Urology. 42 (4): 323–8. doi:10.1016/S0302-2838(02)00354-8. PMID 12361895.
Further reading
- Christensen, Tyler L.; Andriole, Gerald L. (February 2009). "Benign Prostatic Hyperplasia: Current Treatment Strategies". Consultant. 49 (2): 115–22.
