Kidney cancer: Difference between revisions
m Reverted edits by 63.133.240.1 (talk) (HG) (3.1.19) |
Tag: Possible vandalism |
||
| Line 115: | Line 115: | ||
==Treatment== |
==Treatment== |
||
Treatment for kidney cancer depends on the type and stage of the disease. Surgery is the most common treatment as kidney cancer does not often respond to [[chemotherapy]] and [[radiotherapy]]. If the cancer has not spread it will usually be removed by surgery. In some cases this involves [[Nephrectomy|removing the whole kidney]] however most tumors are amenable to [[Nephrectomy|partial removal]] to eradicate the tumor and preserve the remaining normal portion of the kidney. Surgery is not always possible - for example the patient may have other medical conditions that prevent it, or the cancer may have spread around the body and doctors may not be able to remove it.<ref>[http://cancerhelp.cancerresearchuk.org/type/kidney-cancer/treatment/types/early-stage-kidney-cancer#surgery Early stage and locally advanced kidney cancer treatment : Cancer Research UK : CancerHelp UK<!-- Bot generated title -->]</ref> There is currently no evidence that body-wide medical therapy after surgery where there is no known residual disease, that is, [[adjuvant therapy]], helps to improve survival in kidney cancer. If the cancer cannot be treated with surgery other techniques such as [[Cryotherapy|freezing the tumour]] or [[Radiofrequency ablation|treating it with high temperatures]] may be used. However these are not yet used as standard treatments for kidney cancer.<ref>[http://cancerhelp.cancerresearchuk.org/type/kidney-cancer/treatment/types/advanced-kidney-cancer#other Advanced kidney cancer : Cancer Research UK : CancerHelp UK<!-- Bot generated title -->]</ref> Other treatment options include biological therapies (drug treatments that use natural substances from the body) such as [[everolimus|Everolimus (Afinitor)]], [[torisel|Temsirolimus (Torisel)]], [[nexavar|Sorafenib (Nexavar)]], [[sutent|Sunitinib (Sutent)]], and [[axitinib|Axitinib (Inlyta)]], the use of immunotherapy including [[interferon]] and [[interleukin-2]].<ref>[http://hemonc.org/Renal_cancer List of treatments for kidney cancer]</ref><ref>[http://www.nccn.org/professionals/physician_gls/pdf/kidney.pdf NCCN kidney cancer guidelines]</ref><ref>[http://cancerhelp.cancerresearchuk.org/type/kidney-cancer/treatment/biological/ Biological therapy for kidney cancer : Cancer Research UK : CancerHelp UK<!-- Bot generated title -->]</ref> Immunotherapy is successful in 10 to 15% of patients.<ref>{{cite web|url=http://media.cancercare.org/publications/original/16-ccc_kidney_cancer.pdf |title=CancerCare Connect - Treatment Update: Kidney Cancer |publisher=Cancer Care, Inc. |date=August 2012 |accessdate=2012-08-29 |author=Jonasch, Eric |author2=Messner, Carolyn }}</ref> |
Treatment for kidney cancer depends on the type and stage of the disease. Surgery is the most common treatment as kidney cancer does not often respond to [[chemotherapy]] and [[radiotherapy]]. If the cancer has not spread it will usually be removed by surgery. In some cases this involves [[Nephrectomy|removing the whole kidney]] however most tumors are amenable to [[Nephrectomy|partial removal]] to eradicate the tumor and preserve the remaining normal portion of the kidney. Surgery is not always possible - for example the patient may have other medical conditions that prevent it, or the cancer may have spread around the body and doctors may not be able to remove it.<ref>[http://cancerhelp.cancerresearchuk.org/type/kidney-cancer/treatment/types/early-stage-kidney-cancer#surgery Early stage and locally advanced kidney cancer treatment : Cancer Research UK : CancerHelp UK<!-- Bot generated title -->]</ref> There is currently no evidence that body-wide medical therapy after surgery where there is no known residual disease, that is, [[adjuvant therapy]], helps to improve survival in kidney cancer. If the cancer cannot be treated with surgery other techniques such as [[Cryotherapy|freezing the tumour]] or [[Radiofrequency ablation|treating it with high temperatures]] may be used. However these are not yet used as standard treatments for kidney cancer.<ref>[http://cancerhelp.cancerresearchuk.org/type/kidney-cancer/treatment/types/advanced-kidney-cancer#other Advanced kidney cancer : Cancer Research UK : CancerHelp UK<!-- Bot generated title -->]</ref> |
||
Other treatment options include biological therapies (drug treatments that use natural substances from the body) such as [[everolimus|Everolimus (Afinitor)]], [[torisel|Temsirolimus (Torisel)]], [[nexavar|Sorafenib (Nexavar)]], [[sutent|Sunitinib (Sutent)]], and [[axitinib|Axitinib (Inlyta)]], the use of immunotherapy including [[interferon]] and [[interleukin-2]].<ref>[http://hemonc.org/Renal_cancer List of treatments for kidney cancer]</ref><ref>[http://www.nccn.org/professionals/physician_gls/pdf/kidney.pdf NCCN kidney cancer guidelines]</ref><ref>[http://cancerhelp.cancerresearchuk.org/type/kidney-cancer/treatment/biological/ Biological therapy for kidney cancer : Cancer Research UK : CancerHelp UK<!-- Bot generated title -->]</ref> Immunotherapy is successful in 10 to 15% of patients.<ref>{{cite web|url=http://media.cancercare.org/publications/original/16-ccc_kidney_cancer.pdf |title=CancerCare Connect - Treatment Update: Kidney Cancer |publisher=Cancer Care, Inc. |date=August 2012 |accessdate=2012-08-29 |author=Jonasch, Eric |author2=Messner, Carolyn }}</ref> [[Sunitinib]] is the current standard of care in the adjuvant setting along with [[Pazopanib]]; these treatments are often followed by [[Everolimus]], [[Axitinib]], and [[Sorafenib]]. In the second line setting, [[Nivolumab]] demonstrated a statistically significant overall survival advantage in advanced clear renal cell carcinoma over [[Everolimus]] in 2015 and was approved by the [[FDA]]<ref>http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm473971.htm</ref>. [[Cabozantinib]] demonstrated both statistically significant superior progression free survival and overall survival<ref>http://ir.exelixis.com/phoenix.zhtml?c=120923&p=irol-newsArticle&ID=2133957</ref>; it has been granted category 1 classification by the [[NCCN]] along with [[Nivolumab]] for patients with one prior line of VEGFR targeted tyrosine kinase therapy <ref>http://www.nccn.org/disclosures/MinuteHandler.ashx?fileManagerId=280</ref> and is current under FDA review. |
|||
In [[Wilms' tumor]], chemotherapy, radiotherapy and surgery are the accepted treatments, depending on the stage of the disease when it is diagnosed.<ref name="wilms-tumour">[http://cancerhelp.cancerresearchuk.org/about-cancer/cancer-questions/wilms-tumour Wilms' tumour (kidney cancer in children) : Cancer Research UK : CancerHelp UK<!-- Bot generated title -->]</ref> |
In [[Wilms' tumor]], chemotherapy, radiotherapy and surgery are the accepted treatments, depending on the stage of the disease when it is diagnosed.<ref name="wilms-tumour">[http://cancerhelp.cancerresearchuk.org/about-cancer/cancer-questions/wilms-tumour Wilms' tumour (kidney cancer in children) : Cancer Research UK : CancerHelp UK<!-- Bot generated title -->]</ref> |
||
Revision as of 00:51, 3 March 2016
| Kidney cancer | |
|---|---|
| Specialty | Oncology, nephrology |
Kidney cancer, also known as renal cancer, is a type of cancer that starts in the cells in the kidney.
The two most common types of kidney cancer are renal cell carcinoma (RCC) and transitional cell carcinoma (TCC, also known as urothelial cell carcinoma) of the renal pelvis. These names reflect the type of cell from which the cancer developed.
The different types of kidney cancer (such as RCC and UCC) develop in different ways, meaning that the diseases have different long term outcomes, and need to be staged and treated in different ways. RCC is responsible for approximately 80% of primary renal cancers, and UCC accounts the majority of the remainder.[1]
Overall five year survival rates in the United States are 73%.[2]
Types


In addition to renal cell carcinoma and renal pelvis carcinoma, other, less common types of kidney cancer include:
- Squamous cell carcinoma
- Juxtaglomerular cell tumor (reninoma)
- Angiomyolipoma
- Bellini duct carcinoma
- Clear-cell sarcoma of the kidney
- Mesoblastic nephroma
- Wilms' tumor, usually is reported in children under the age of 5.
- Mixed epithelial stromal tumor[3]
Rarely, some other types of cancer and potentially cancerous tumors that more usually originate elsewhere can originate in the kidneys. These include:
- Clear cell adenocarcinoma
- Transitional cell carcinoma
- Inverted papilloma
- Renal lymphoma
- Teratoma[4]
- Carcinosarcoma[5]
- Carcinoid tumor of the renal pelvis[6]
Cancer in the kidney may also be secondary, the result of metastasis from a primary cancer elsewhere in the body.
Signs and symptoms
The most common signs and symptoms of kidney cancer are a mass in the abdomen and/or blood in the urine (or hematuria). Other symptoms may include tiredness, loss of appetite, weight loss, a high temperature and heavy sweating, and persistent pain in the abdomen.[7][8] However, many of these symptoms can be caused by other conditions, and there may also be no signs or symptoms in a person with kidney cancer, especially in the early stages of the disease.
Stages
-
Stage 1 kidney cancer
-
Stage 2 kidney cancer
-
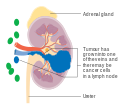
Stage 3 kidney cancer
-
Stage 4 kidney cancer
Causes
Factors that increase the risk of kidney cancer include smoking, which can double the risk of the disease; regular use of NSAIDs such as ibuprofen and naproxen, which may increase the risk by 51%[9] or may not;[10] obesity; faulty genes; a family history of kidney cancer; having kidney disease that needs dialysis; being infected with hepatitis C; and previous treatment for testicular cancer or cervical cancer.
There are also other possible risk factors such as kidney stones[11] and high blood pressure, which are being investigated.[12]
Pathophysiology
Kidney cancer originates in the kidney in two principal locations: the renal tubule and the renal pelvis. Most cancers in the renal tubule are renal cell carcinoma and clear cell adenocarcinoma. Most cancers in the renal pelvis are transitional cell carcinoma.
Treatment
Treatment for kidney cancer depends on the type and stage of the disease. Surgery is the most common treatment as kidney cancer does not often respond to chemotherapy and radiotherapy. If the cancer has not spread it will usually be removed by surgery. In some cases this involves removing the whole kidney however most tumors are amenable to partial removal to eradicate the tumor and preserve the remaining normal portion of the kidney. Surgery is not always possible - for example the patient may have other medical conditions that prevent it, or the cancer may have spread around the body and doctors may not be able to remove it.[13] There is currently no evidence that body-wide medical therapy after surgery where there is no known residual disease, that is, adjuvant therapy, helps to improve survival in kidney cancer. If the cancer cannot be treated with surgery other techniques such as freezing the tumour or treating it with high temperatures may be used. However these are not yet used as standard treatments for kidney cancer.[14]
Other treatment options include biological therapies (drug treatments that use natural substances from the body) such as Everolimus (Afinitor), Temsirolimus (Torisel), Sorafenib (Nexavar), Sunitinib (Sutent), and Axitinib (Inlyta), the use of immunotherapy including interferon and interleukin-2.[15][16][17] Immunotherapy is successful in 10 to 15% of patients.[18] Sunitinib is the current standard of care in the adjuvant setting along with Pazopanib; these treatments are often followed by Everolimus, Axitinib, and Sorafenib. In the second line setting, Nivolumab demonstrated a statistically significant overall survival advantage in advanced clear renal cell carcinoma over Everolimus in 2015 and was approved by the FDA[19]. Cabozantinib demonstrated both statistically significant superior progression free survival and overall survival[20]; it has been granted category 1 classification by the NCCN along with Nivolumab for patients with one prior line of VEGFR targeted tyrosine kinase therapy [21] and is current under FDA review.
In Wilms' tumor, chemotherapy, radiotherapy and surgery are the accepted treatments, depending on the stage of the disease when it is diagnosed.[22]
IMA901 is used to treat patients with cancer of the kidneys. It is composed of ten synthetic tumor-associated peptides (TUMAPs), which activate the body's own killer T-cells against the tumor. Unlike chemotherapy, this process targets the body's immune responses and mobilizes them to attack the cancer.[23]
Children
The majority of kidney cancers reported in children are Wilms' tumors. These tumors can begin to grow when a fetus is still developing in the uterus, and may not cause problems until the child is a few years old. Wilms' tumor is most common in children under the age of 5, but can rarely be diagnosed in older children or in adults. It is still not clear what causes most Wilms' tumors. The most common symptoms are swelling of the abdomen and blood in the urine.[22]
Epidemiology
Around 208,500 new cases of kidney cancer are diagnosed in the world each year, accounting for just under 2% of all cancers.[24] The highest rates are recorded in North America and the lowest rates in Asia and Africa.[25]
United States
The United States' NIH estimates for 2013 around 64,770 new cases of kidney cancer and 13,570 deaths from the disease.[26]
The incidence of kidney cancer is also increasing in the United States. This is thought to be a real increase, not only due to changes in the way the disease is diagnosed.[27]
Europe
The most recent estimates of incidence of kidney cancer suggest that there are 63,300 new cases annually in the EU25. In Europe, kidney cancer accounts for nearly 3% of all cancer cases.[28]
United Kingdom
Kidney cancer is the eighth most common cancer in the UK (around 10,100 people were diagnosed with the disease in 2011), and it is the fourteenth most common cause of cancer death (around 4,300 people died in 2012).[29]
See also
References
- ^ Mulders PF, Brouwers AH, Hulsbergen-van der Kaa CA, van Lin EN, Osanto S, de Mulder PH (February 2008). "[Guideline 'Renal cell carcinoma']". Ned Tijdschr Geneeskd (in Dutch and Flemish). 152 (7): 376–80. PMID 18380384.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "SEER Stat Fact Sheets: Kidney and Renal Pelvis Cancer". NCI. Retrieved 18 June 2014.
- ^ Thyavihally YB, Tongaonkar HB, Desai SB (September 2005). "Benign mixed epithelial stromal tumor of the renal pelvis with exophytic growth: case report". Int Semin Surg Oncol. 2: 18. doi:10.1186/1477-7800-2-18. PMC 1215508. PMID 16150156.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: postscript (link) CS1 maint: unflagged free DOI (link) - ^ Nzegwu MA, Aligbe JU, Akintomide GS, Akhigbe AO (May 2007). "Mature cystic renal teratoma in a 25-year-old woman with ipsilateral hydronephrosis, urinary tract infection and spontaneous abortion". Eur J Cancer Care (Engl). 16 (3): 300–2. doi:10.1111/j.1365-2354.2006.00755.x. PMID 17508953.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: postscript (link) - ^ Chiu KC, Lin MC, Liang YC, Chen CY (2008). "Renal carcinosarcoma: case report and review of literature". Ren Fail. 30 (10): 1034–9. doi:10.1080/08860220802403192. PMID 19016157.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: postscript (link) - ^ Kuroda N, Katto K, Tamura M, Shiotsu T, Hes O, Michal M, Nagashima Y, Ohara M, Hirouchi T, Mizuno K, Hayashi Y, Lee GH (January 2008). "Carcinoid tumor of the renal pelvis: consideration on the histogenesis". Pathol. Int. 58 (1): 51–4. doi:10.1111/j.1440-1827.2007.02188.x. PMID 18067641.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: postscript (link) - ^ Symptoms of kidney cancer : Cancer Research UK : CancerHelp UK
- ^ Katie Charles (January 19, 2011). "Kidney cancer: Innovative new treatments boost survival rates for cancer patients: Daily Checkup with Michael Palese". New York Daily News. Retrieved February 23, 2011.
- ^ "Commonly Used Pain Pills Increase Kidney Cancer Risk in Study". Bloomberg.
- ^ Lipworth, Loren; Robert E. Tarone; Joseph K McLaughlin (13 December 2005). "The Epidemiology of Renal Cell Carcinoma". Journal of Urology. 176 (6): 2353–235. doi:10.1016/j.juro.2006.07.130. PMID 17085101. Retrieved 2012-07-15.
- ^ Cheungpasitporn, W; Thongprayoon C; O'Corragain OA; Edmonds PJ; Ungprasert P; Kittanamongkolchai W; Erickson SB (9 September 2014). "The Risk of Kidney Cancer in Patients with Kidney Stones: A Systematic Review and Meta-analysis". QJM. 108: 205–12. doi:10.1093/qjmed/hcu195. PMID 25208892.
- ^ Risks and causes of kidney cancer : Cancer Research UK : CancerHelp UK
- ^ Early stage and locally advanced kidney cancer treatment : Cancer Research UK : CancerHelp UK
- ^ Advanced kidney cancer : Cancer Research UK : CancerHelp UK
- ^ List of treatments for kidney cancer
- ^ NCCN kidney cancer guidelines
- ^ Biological therapy for kidney cancer : Cancer Research UK : CancerHelp UK
- ^ Jonasch, Eric; Messner, Carolyn (August 2012). "CancerCare Connect - Treatment Update: Kidney Cancer" (PDF). Cancer Care, Inc. Retrieved 2012-08-29.
- ^ http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm473971.htm
- ^ http://ir.exelixis.com/phoenix.zhtml?c=120923&p=irol-newsArticle&ID=2133957
- ^ http://www.nccn.org/disclosures/MinuteHandler.ashx?fileManagerId=280
- ^ a b Wilms' tumour (kidney cancer in children) : Cancer Research UK : CancerHelp UK
- ^ Steffen Walter; Toni Weinschenk; Arnulf Stenzl; Romuald Zdrojowy; et al. (August 2012). "Multipeptide immune response to cancer vaccine IMA901 after single-dose cyclophosphamide associates with longer patient survival". Nature Medicine. pp. 1254–1261. doi:10.1038/nm.2883. PMID 22842478.
- ^ Lindblad, P. and Adami H.O, Kidney Cancer, in Textbook of Cancer.
- ^ GLOBOCAN 2002, Cancer Incidence, Mortality and Prevalence Worldwide 2002 estimates. 2006.
- ^ "Cancer of the Kidney and Renal Pelvis - SEER Stat Fact Sheets". National Cancer Institute, U.S. National Institutes of Health. Retrieved 2013-02-07.
- ^ Lynch, Charles F.; West, Michele M.; Davila, Jessica A.; Platz, Charles E. (2007). "Chapter 24: Cancers of the Kidney and Renal Pelvic". In Ries, LAG; Young, JL; Keel, GE; Eisner, MP; Horner, M-J (eds.). SEER Survival Monograph: Cancer Survival Among Adults: US SEER Program, 1988-2001, Patient and Tumor Characteristics. SEER Program. Vol. NIH Pub. No. 07-6215. Bethesda, MD: National Cancer Institute. pp. 193–202.
{{cite book}}: CS1 maint: postscript (link) - ^ Ferlay J, et al. (2007). "Estimates of the cancer incidence and mortality in Europe in 2006". Annals of Oncology. 18 (3): 581–92. doi:10.1093/annonc/mdl498. PMID 17287242.
- ^ "Kidney cancer statistics". Cancer Research UK. Retrieved 27 October 2014.
External links
- "U.S. NIH - Cancer of the Kidney and Renal Pelvis - Statistics".
- Clinically reviewed kidney cancer information for patients, from Cancer Research UK
- UK kidney cancer statistics from Cancer Research UK
- Cancer.Net: Kidney Cancer