Acne: Difference between revisions
→Misconceptions about causes: clean up |
No edit summary |
||
| Line 13: | Line 13: | ||
'''Acne vulgaris''' is an [[inflammatory]] disease of the [[skin]], caused by changes in the pilosebaceous units (skin structures consisting of a [[hair follicle]] and its associated [[sebaceous gland]]). Acne lesions are commonly referred to as [[pimples]], spots or zits. |
'''Acne vulgaris''' is an [[inflammatory]] disease of the [[skin]], caused by changes in the pilosebaceous units (skin structures consisting of a [[hair follicle]] and its associated [[sebaceous gland]]). Acne lesions are commonly referred to as [[pimples]], spots or zits. |
||
The condition is most common in [[puberty]]. It is considered an abnormal response to normal levels of the male [[hormone]] [[testosterone]]. The response for most people diminishes over time and acne thus tends to disappear, or at least decrease, after one reaches his or her early twenties. There is, however, no way to predict how long it will take for it to disappear entirely, and some individuals will continue to suffer from acne decades later, into their thirties and forties and even beyond. {{Fact|date=March 2007}} Acne affects a large percentage of humans at some stage in life. |
The condition is most common in [[puberty]] and often leads to people being called "pizza face". It is considered an abnormal response to normal levels of the male [[hormone]] [[testosterone]]. The response for most people diminishes over time and acne thus tends to disappear, or at least decrease, after one reaches his or her early twenties. There is, however, no way to predict how long it will take for it to disappear entirely, and some individuals will continue to suffer from acne decades later, into their thirties and forties and even beyond. {{Fact|date=March 2007}} Acne affects a large percentage of humans at some stage in life. |
||
The term ''acne'' comes from a corruption of the [[Greek language|Greek]] ''άκμή'' (acme in the sense of a skin eruption) in the writings of [[Aëtius Amidenus]]. The vernacular term ''bacne'' or ''backne'' is often used to indicate acne found specifically on one's back. |
The term ''acne'' comes from a corruption of the [[Greek language|Greek]] ''άκμή'' (acme in the sense of a skin eruption) in the writings of [[Aëtius Amidenus]]. The vernacular term ''bacne'' or ''backne'' is often used to indicate acne found specifically on one's back. |
||
Revision as of 04:50, 29 March 2007
| Acne | |
|---|---|
| Specialty | Dermatology, family medicine |
Acne vulgaris is an inflammatory disease of the skin, caused by changes in the pilosebaceous units (skin structures consisting of a hair follicle and its associated sebaceous gland). Acne lesions are commonly referred to as pimples, spots or zits.
The condition is most common in puberty and often leads to people being called "pizza face". It is considered an abnormal response to normal levels of the male hormone testosterone. The response for most people diminishes over time and acne thus tends to disappear, or at least decrease, after one reaches his or her early twenties. There is, however, no way to predict how long it will take for it to disappear entirely, and some individuals will continue to suffer from acne decades later, into their thirties and forties and even beyond. [citation needed] Acne affects a large percentage of humans at some stage in life.
The term acne comes from a corruption of the Greek άκμή (acme in the sense of a skin eruption) in the writings of Aëtius Amidenus. The vernacular term bacne or backne is often used to indicate acne found specifically on one's back.
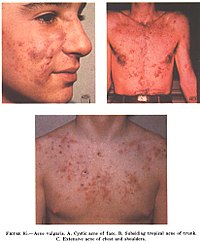
Symptoms
The most common form of acne is known as "acne vulgaris", meaning "common acne." Excessive secretion of oils from the sebaceous glands accompanies the plugging of the pores with naturally occurring dead skin cells (corneocytes) blocking hair follicles. The accumulation of these corneocytes in the duct appears to be due to a failure of the normal keratinization process in the skin which usually leads to shedding of skin cells lining the pores. Oil secretions are said to build up beneath the blocked pore, providing a perfect environment for the skin bacteria Propionibacterium acnes and the lipophilic (oil/lipid-loving) yeast Malassezia[citation needed] to multiply uncontrollably. Under the microscope, however, there is no evidence of pooled trapped sebum. Indeed the oil percolates through the plugged duct onto the surface. In response to the bacterial and yeast populations, the skin inflames, producing the visible lesion. The face, chest, back, shoulders and upper arms are especially affected. The typical acne lesions are: comedones, papules, pustules, nodules and inflammatory cysts. These are the more inflamed form of pus-filled or reddish bumps, even boil-like tender swellings. Non-inflamed 'sebaceous cysts', more properly called epidermoid cysts, occur either in association with acne or alone but are not a constant feature. After resolution of acne lesions, prominent unsightly scars may remain.
Aside from scarring, its main effects are psychological, such as reduced self-esteem[1] and depression or suicide.[2] Acne usually appears during adolescence, when people already tend to be most socially insecure. Early and aggressive treatment is therefore advocated to lessen the overall impact to individuals.[1]
Causes of acne
Exactly why some people get acne and some do not is not fully known. It is known to be partly hereditary. Several factors are known to be linked to acne:
- Hormonal activity, such as menstrual cycles and puberty
- Diet
- Stress, through increased output of hormones from the adrenal (stress) glands.
- Hyperactive sebaceous glands, secondary to the three hormone sources above.
- Accumulation of dead skin cells.
- Bacteria in the pores, to which the body becomes 'allergic'.
- Skin irritation or scratching of any sort will activate inflammation.
- Use of anabolic steroids.
- Any medication containing halogens (iodides, chlorides, bromides), lithium, barbiturates, or androgens.
- Exposure to high levels of chlorine compounds, particularly chlorinated dioxins, can cause severe, long-lasting acne, known as Chloracne.
Traditionally, attention has focused mostly on hormone-driven over-production of sebum as the main contributing factor of acne. More recently, more attention has been given to narrowing of the follicle channel as a second main contributing factor. Abnormal shedding of the cells lining the follicle, abnormal cell binding ("hyperkeratinization") within the follicle, and water retention in the skin (swelling the skin and so pressing the follicles shut) have all been put forward as important mechanisms. Several hormones have been linked to acne: the male hormones testosterone, dihydrotestosterone (DHT) and dehydroepiandrosterone sulfate (DHEAS), as well as insulin-like growth factor 1 (IGF-I). In addition, acne-prone skin has been shown to be insulin resistant [citation needed].
Development of acne vulgaris in later years is uncommon, although this is the age group for Rosacea which may have similar appearances. True acne vulgaris in adults may be a feature of an underlying condition such as pregnancy and disorders such as polycystic ovary syndrome or the rare Cushing's syndrome. Dermatologists are seeing more cases of menopause-associated acne as fewer women replace the natural anti-acne ovarian hormone estradiol whose production fails as women arrive at menopause. The lack of estradiol also causes thinning hair, hot flashes, thin skin, wrinkles, vaginal dryness, and predisposes to osteopenia and osteoporosis as well as triggering acne (known as acne climacterica in this situation).
Misconceptions about causes
There are many misconceptions and rumors about what does and does not cause the condition:
Diet
Diet. One study suggested that chocolate, french fries, potato chips and sugar, among others, affect acne. A high GI (glycemic index) diet that causes sharp rises in blood sugar worsens acne. This, however, has been refuted by dermatologists and has been accepted as myth.[3] If this study's conclusions are verified then a low GI diet may help acne, but a recent review of somewhat dated scientific literature cannot affirm either way.[4] A recent study, based on a survey of 47,335 women, did find a positive epidemiological association between acne and consumption of partially skimmed milk, instant breakfast drink, sherbet, cottage cheese and cream cheese.[5] The researchers hypothesize that the association may be caused by hormones (such as several sex hormones and bovine IGF-I) present in cow milk. Although the association between milk and acne has been definitively shown, the ingredient in the milk responsible for the acne is still unclear. Most dermatologists are awaiting confirmatory research linking diet and acne but some support the idea that acne sufferers should experiment with their diets, and refrain from consuming such fare if they find such food affects the severity of their acne.[6]
Seafood, on the other hand, may contain relatively high levels of iodine. Iodine is known to make existing acne worse but there is probably not enough to cause an acne outbreak.[7]< Still, people who are prone to acne may want to avoid excessive consumption of foods high in iodine.
It has also been suggested that there is a link between a diet high in refined sugars and other processed foods and acne. According to this hypothesis, the startling absence of acne in non-westernized societies could be explained by the low glycemic index of these cultures' diets. Others have cited possible genetic reasons for there being no acne in these populations, but similar populations shifting to Western diets do develop acne. Note also that the populations studied consumed no milk or other dairy products.[8] Further research is necessary to establish whether a reduced consumption of high-glycemic foods (such as soft drinks, sweets, white bread) can significantly alleviate acne, though consumption of high-glycemic foods should in any case be kept to a minimum, for general health reasons.[9] Avoidance of 'junk food' with its high fat and sugar content is also recommended.[10] On the other hand there is no evidence that fat alone makes skin more oily or acne worse.
Hygiene
Deficient personal hygiene. Acne is not caused by dirt. This misconception probably comes from the fact that comedones look like dirt stuck in the openings of pores. The black color is simply not dirt but compact keratin. In fact, the blockages of keratin that cause acne occur deep within the narrow follicle channel, where it is impossible to wash them away. These plugs are formed by the failure of the cells lining the duct to separate and flow to the surface in the sebum created there by the body.
Sex
Sex. Common myths state that masturbation causes acne and, conversely, that celibacy or sexual intercourse can cure it. Though it has been widely accepted that these are not true due to lack of scientific study on the subject, it is also important to note sexual activity has been observed to result in hormonal spikes, which has been linked to acne.[11]
Treatments
Timeline of acne treatment
The history of acne reaches back to the dawn of recorded history. In Ancient Egypt, it is recorded that several pharaohs were acne sufferers. From Ancient Greece comes the English word 'acne' (meaning 'point' or 'peak'). Acne treatments are also of considerable antiquity:
- Ancient Rome : bathing in hot, and often sulfurous, mineral water was one of the few available acne treatments. One of the earliest texts to mention skin problems is De Medicina by the Roman writer Celsus.
- 1800s: Nineteenth century dermatologists used sulphur in the treatment of acne. It was believed to dry the skin.
- 1920s: Benzoyl Peroxide is used
- 1930s: Laxatives were used as a cure for what were known as 'chastity pimples'
- 1950s: When antibiotics became available, it was discovered that they had beneficial effects on acne. They were taken orally to begin with. Much of the benefit was not from killing bacteria but from the anti-inflammatory effects of tetracycline and its relatives. Topical antibiotics became available later.
- 1960s: Tretinoin (original Trade Name Retin A) was found effective for acne. This preceeded the development of oral isotretinoin (sold as Accutane and Roaccutane) since the early 1980s.
- 1980s: Accutane is introduced in America
- 1990s: Laser treatment introduced
- 2000s: Blue/red light therapy
Some old treatments, like laxatives, have fallen into disuse but others, like spas, are recovering their popularity.
Available treatments
There are many products sold for the treatment of acne, many of them without any scientifically-proven effects. Generally speaking successful treatments give little improvement within the first week or two; and then the acne decreases over approximately 3 months, after which the improvement starts to flatten out. Treatments that promise improvements within 2 weeks are likely to be largely disappointing. Short bursts of cortisone, quick bursts of antibiotics and many of the laser therapies offer a quick reduction in the redness, swelling and inflammation when used correctly, but none of these empty the pore of all the materials that trigger the inflammation. Emptying the pores takes months.
Modes of improvement are not necessarily fully understood but in general treatments are believed to work in at least 4 different ways (with many of the best treatments providing multiple simultaneous effects):
- normalising shedding into the pore to prevent blockage
- killing P. acnes
- antinflammatory effects
- hormonal manipulation
A combination of treatments can greatly reduce the amount and severity of acne in many cases. Those treatments that are most effective tend to have greater potential for side effects and need a greater degree of monitoring, so a step-wise approach is often taken. Many people consult with doctors when deciding which treatments to use, especially when considering using any treatments in combination. There are a number of treatments that have been proven effective:

Exfoliating the skin
This can be done either mechanically, using an abrasive cloth or a liquid scrub, or chemically. Common chemical exfoliating agents include salicylic acid and glycolic acid, which encourage the peeling of the top layer of skin to prevent a build-up of dead skin cells which combine with skin oil to block pores. It also helps to unblock already clogged pores.[citation needed] Note that the word "peeling" is not meant in the visible sense of shedding, but rather as the destruction of the top layer of skin cells at the microscopic level. Depending on the type of exfoliation used, some visible flaking is possible. Moisturizers and anti-acne topicals containing chemical exfoliating agents are commonly available over-the-counter. Mechanical exfoliation is less commonly used as many benefits derived from the exfoliation are negated by the act of mechanically rubbing and irritating the skin.
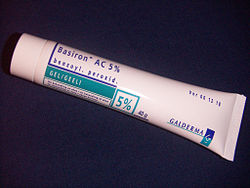
Topical Bactericidals
Widely available OTC bactericidal products containing benzoyl peroxide may be used in mild to moderate acne. The gel or cream containing benzoyl peroxide is rubbed, twice daily, into the pores over the affected region. Bar soaps or washes may also be used and vary from 2 to 10% in strength. In addition to its therapeutic effect as a keratolytic (a chemical that dissolves the keratin plugging the pores) benzoyl peroxide also prevents new lesions by killing P.acnes. Unlike antibiotics, benzoyl peroxide has the advantage of being a strong oxidizer (essentially a mild bleach) and thus does not appear to generate bacterial resistance. However, it routinely causes dryness, local irritation and redness. A sensible regimen may include the daily use of low-concentration (2.5%) benzoyl peroxide preparations, combined with suitable non-comedogenic moisturisers to help avoid overdrying the skin.[12] This has occasioned widespread editorial comment.[13]
Phototherapy
Blue and red light
It has long been known that short term improvement can be achieved with sunlight. However, studies have shown that sunlight worsens acne long-term, presumably due to UV damage. [citation needed] More recently, visible light has been successfully employed to treat acne (Phototherapy) - in particular intense blue light generated by purpose-built fluorescent lighting, dichroic bulbs, LEDs or lasers. Used twice weekly, this has been shown to reduce the number of acne lesions by about 64%;[14] and is even more effective when applied daily. The mechanism appears to be that a porphyrin (Coproporphyrin III) produced within P. acnes generates free radicals when irradiated by blue light.[15] Particularly when applied over several days, these free radicals ultimately kill the bacteria.[16] Since porphyrins are not otherwise present in skin, and no UV light is employed, it appears to be safe, and has been licensed by the U.S. FDA.[17] The treatment apparently works even better if used with red visible light (660 nanometer) resulting in a 76% reduction of lesions after 3 months of daily treatment for 80% of the patients;[18] and overall clearance was similar or better than benzoyl peroxide. Unlike most of the other treatments few if any negative side effects are typically experienced, and the development of bacterial resistance to the treatment seems very unlikely. After treatment, clearance can be longer lived than is typical with topical or oral antibiotic treatments; several months is not uncommon. The equipment or treatment, however, is relatively new and reasonably expensive.
Photodynamic therapy
In addition, basic science and clinical work by dermatologists Yoram Harth and Alan Shalita and others has produced evidence that intense blue/violet light (405-425 nanometer) can decrease the number of inflammatory acne lesion by 60-70% in 4 weeks of therapy, particularly when the P.acnes is pretreated with delta-aminolevulinic acid (ALA), which increases the production of porphyrins. However this photodynamic therapy is controversial and apparently not published in a peer reviewed
Less widely used treatments
- Azelaic acid (brand names Azelex, Finevin, Skinoren) is suitable for mild, comedonal acne.[19]
- Zinc. Orally administered zinc gluconate has been shown to be effective in the treatment of inflammatory acne, although less so than tetracyclines.[20][21]
- Tea Tree Oil (Melaleuca Oil) has been used with some success, and has been shown to be an effective anti-inflammatory in skin infections [22]
- Heat therapy - Zeno product uses heat at a specific temperature to kill bacteria and to treat mild to moderate acne.[citation needed]
- Niacinamide, (Vitamin B3) used topically in the form of a gel, has been shown in a 1995 study to be more effective than a topical antibiotic used for comparison, as well as having less side effects.[23] Topical niacinamide is available both on prescription and over-the-counter. Some users choose to make their own at home, mixing together crushed niacinamide pills with aloe vera gel.[citation needed] The property of topical niacinamide's benefit in treating acne seems to be it's anti-inflammatory nature. It is also purported to result in increased synthesis of collagen, keratin, involucrin and flaggrin.[citation needed]
- In some cases, people found that bathing in salt water (pure from the ocean) noticed lessened redness and decreased size in their acne.
Future treatments
Laser surgery has been in use for some time to reduce the scars left behind by acne, but research is now being done on lasers for prevention of acne formation itself. The laser is used to produce one of the following effects:
- to burn away the follicle sac from which the hair grows
- to burn away the sebaceous gland which produces the oil
- to induce formation of oxygen in the bacteria, killing them
Since lasers and intense pulsed light sources cause thermal damage to the skin there are concerns that laser or intense pulsed light treatments for acne will induce hyperpigmented macules (spots) or cause long term dryness of the skin. As of 2005, this is still mostly at the stage of medical research rather than established treatment.
Because acne appears to have a significant hereditary link, there is some expectation that cheap whole-genome DNA sequencing may help isolate the body mechanisms involved in acne more precisely, possibly leading to a more satisfactory treatment. (Crudely put, take the DNA of large samples of people with significant acne and of people without, and let a computer search for statistically strong differences in genes between the two groups). However, as of 2005, DNA sequencing is not yet cheap, and all this may still be decades off. It is also possible that gene therapy could be used to alter the skin's DNA.
Phage therapy has been proposed to kill P. acnes, and has seen some use, particularly in Georgia.[24]
Preferred treatments by types of acne vulgaris
- Comedonal (non-inflammatory) acne: local treatment with azelaic acid, salicylic acid, topical retinoids, benzoyl peroxide.
- Mild papulo-pustular (inflammatory) acne: benzoyl peroxide or topical retinoids, topical antibiotics (such as erythromycin).
- Moderate inflammatory acne: benzoyl peroxide or topical retinoids combined with oral antibiotics (tetracyclines). Isotretinoin is an option.
- Severe inflammatory acne, nodular acne, acne resistant to the above treatments: isotretinoin, or contraceptive pills with cyproterone for females with virilization or drospirenone.
- Most physicians state that topical retinoids are the preferred treatment for all forms of acne vulgaris.
- There are also certain treatments for acne mentioned in Ayurveda using herbs such as Aloevera, Aruna, Haldi, and Papaya.[25]
Acne scars
Severe acne often leaves small scars where the skin gets a "volcanic" shape. Acne scars are difficult and expensive to treat, and it is unusual for the scars to be successfully removed completely.[citation needed]
The psychological and emotional effects caused by acne scars can be as devastating to one's confidence as the acne once was.
Acne scars generally fall into two categories: physical scars and pigmented scars. Physical acne scars are often referred to as "Icepick" scars. This is because the scars tend to cause an indentation in the skins surface. Pigmented scars is a slightly misleading term, suggesting a change in the skin's pigmentation. This is not true. Pigmented scars are usually the result of nodular or cystic acne (the painful 'bumps' lying under the skin). They often leave behind an inflamed red mark. Often, the pigmentation scars can be avoided simply by avoiding aggravation of the nodule or cyst. When sufferers try to 'pop' cysts or nodules, pigmentation scarring becomes significantly worse, and may even bruise the affected area. Pigmentation scars often fade with time, and those who suffered from acne before, and have developed scars are generally relieved that the acne has gone, and emotional effects of acne scars tend to be less distressing.
Acne scars are unsightly, and it is for this reason they can be psychologically and emotionally distressing. However, there are a range of treatments available. If acne scars are causing severe psychological distress, social withdrawal and/or emotional ill-health, a physician should be contacted.
Grading scale
There are multiple grading scales for grading the severity of acne vulgaris,[26] three of these being: Leeds acne grading technique: Counts and categorises lesions into inflammatory and non-inflammatory (ranges from 0-10.0). 'Cook's acne grading scale: Uses photographs to grade severity from 0 to 8 (0 being the least severe and 8 being the most severe). Pillsbury scale: Simple classifies the severity of the acne from 1 (least severe) to 4 (most severe).
See also
References
- James W (2005). "Clinical practice. Acne". N Engl J Med. 352 (14): 1463–72. PMID 15814882.
{{cite journal}}: Unknown parameter|month=ignored (help) - Webster G (2002). "Acne vulgaris". BMJ. 325 (7362): 475–9. PMID 12202330.
{{cite journal}}: Unknown parameter|month=ignored (help)
Footnotes
- ^ a b Goodman G (2006). "Acne and acne scarring - the case for active and early intervention" (PDF). Aust Fam Physician. 35 (7): 503–4. PMID 16820822.
- ^ Purvis D, Robinson E, Merry S, Watson P (2006). "Acne, anxiety, depression and suicide in teenagers: a cross-sectional survey of New Zealand secondary school students". J Paediatr Child Health. 42 (12): 793–6. PMID 17096715.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
One study has estimated the incidence of suicidal ideation in patients with acne as 7.1% :
* Picardi A, Mazzotti E, Pasquini P (2006). "Prevalence and correlates of suicidal ideation among patients with skin disease". J Am Acad Dermatol. 54 (3): 420–6. PMID 16488292.{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ CHOICE - Citizens for Healthy Options In Children's Education (2003). "Acne Has Nothing to Do with Diet - Wrong!".
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Magin P, Pond D, Smith W, Watson A (2005). "A systematic review of the evidence for 'myths and misconceptions' in acne management: diet, face-washing and sunlight". Fam Pract. 22 (1): 62–70. PMID 15644386.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Adebamowo CA, Spiegelman D, Danby FW, Frazier AL, Willett WC, Holmes MD (2005). "High school dietary dairy intake and teenage acne". J Am Acad Dermatol. 52 (2): 207–14. PMID 15692464.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fries JH (1978). "Chocolate: a review of published reports of allergic and other deleterious effects, real or presumed". Ann Allergy. 41 (4): 195–207. PMID 152075.
- ^ Danby FW (2007). "Acne and iodine: Reply". J Am Acad Dermatol. 56 (1): 164–5. PMID 17190637.
- ^ Loren Cordain, et al. "Acne Vulgaris - A Disease of Western Civilization" Arch Dermatol. 2002;138:1584-1590. Observation
- ^ Smith R, Mann N, Makelainen H, Braue A, Varigos G (2004). "The effect of short-term altered macronutrient status on acne vulgaris and biochemical markers of insulin sensitivity". Asia Pac J Clin Nutr. 13 (Suppl): S67. PMID 15294556.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Anderson, Laurence. 2006. Looking Good, the Australian guide to skin care, cosmetic medicine and cosmetic surgery. AMPCo. Sydney. ISBN 0-85557-044-X.
- ^ Endocrine effects of masturbation in men.
- ^ "The iPLEDGE Program - Guide to Best Practices for Isotretinoin - "The resource to help the prescriber prepare, plan treatments, and prevent pregnancies during the course of isotretinoin therapy"" (PDF). 2005.
- ^ Bernadine Healy (2005-05-09). "Pledging for Accutane". US News Best Health.
{{cite news}}: Check date values in:|date=(help) - ^ Kawada A, Aragane Y, Kameyama H, Sangen Y, Tezuka T (2002). "Acne phototherapy with a high-intensity, enhanced, narrow-band, blue light source: an open study and in vitro investigation". J Dermatol Sci. 30 (2): 129–35. PMID 12413768.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Kjeldstad B (1984). "Photoinactivation of Propionibacterium acnes by near-ultraviolet light". Z Naturforsch [C]. 39 (3–4): 300–2. PMID 6730638.
- ^ Ashkenazi H, Malik Z, Harth Y, Nitzan Y (2003). "Eradication of Propionibacterium acnes by its endogenic porphyrins after illumination with high intensity blue light". FEMS Immunol Med Microbiol. 35 (1): 17–24. PMID 12589953.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "New Light Therapy for Acne" U.S. Food and Drug Administration, FDA Consumer magazine, November-December 2002 Notice
- ^ Papageorgiou P, Katsambas A, Chu A (2000). "Phototherapy with blue (415 nm) and red (660 nm) light in the treatment of acne vulgaris" (PDF). Br J Dermatol. 142 (5): 973–8. PMID 10809858.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ MedlinePlus (2001-07-24). "Azelaic Acid (Topical)".
- ^ Dreno B, Amblard P, Agache P, Sirot S, Litoux P (1989). "Low doses of zinc gluconate for inflammatory acne". Acta Derm Venereol. 69 (6): 541–3. PMID 2575335.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Dreno B, Moyse D, Alirezai M, Amblard P, Auffret N, Beylot C, Bodokh I, Chivot M, Daniel F, Humbert P, Meynadier J, Poli F (2001). "Multicenter randomized comparative double-blind controlled clinical trial of the safety and efficacy of zinc gluconate versus minocycline hydrochloride in the treatment of inflammatory acne vulgaris". Dermatology. 203 (2): 135–40. PMID 11586012.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Koh KJ; Pearce AL; Marshman G; Finlay-Jones JJ; Hart PH Department of Dermatology, Flinders Medical Centre, Bedford Park, South Australia, Australia (2002). "Tea tree oil reduces histamine-induced skin inflammation". Dermatology: 147. ISSN 0007-0963.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Shalita A, Smith J, Parish L, Sofman M, Chalker D (1995). "Topical nicotinamide compared with clindamycin gel in the treatment of inflammatory acne vulgaris". Int J Dermatol. 34 (6): 434–7. PMID 7657446.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ The star ledger- Germs that fight germs
- ^ Ayurveda Encyclopedia, "Acne Treatment"
- ^ Leeds, Cook's and Pillsbury scales obtained from here
External links
- Acne vulgaris: more than skin deep (on the psychological effects of acne)
- Story on Acne from the Better Health Channel (Quality assured by the Victorian government, Australia)
- "AcneNet". American Academy of Dermatology. - Dermatologist-reviewed information about acne.
- "Acne Questions and Answers". From the National Institute of Health.
- "Acne & Microdermabrasion".
{{cite web}}: Cite has empty unknown parameter:|1=(help) - Premium acne and microdermabrasion resource
