Dissociative identity disorder: Difference between revisions
Rescuing orphaned refs ("Rind 2000 1–62" from Rind et al. controversy) |
→History: removing, I really think this is irrelevant here |
||
| Line 152: | Line 152: | ||
In 1994, the fourth edition of the DSM replaced the criteria again and changed the name of the condition from "multiple personality disorder" to the current "dissociative identity disorder" to emphasize the importance of changes to consciousness and identity rather than personality. The inclusion of interpersonality amnesia helped to distinguish DID from [[dissociative disorder not otherwise specified]], but the condition retains an inherent subjectivity due to difficulty in defining terms such as personality, identity, ego-state and even [[amnesia]].<ref name = Kihlstrom>{{cite pmid | 17716088}}</ref> The [[ICD-10]] still classifies DID as a "Dissociative [conversion] disorder" and retains the name "multiple personality disorder" with the classification number of F44.8.81.<ref name = ICD10>{{cite web | url = http://www.who.int/classifications/icd/en/GRNBOOK.pdf | format = pdf | publisher = [[World Health Organization]] | title = The ICD-10 Classification of Mental and Behavioural Disorders }}</ref> |
In 1994, the fourth edition of the DSM replaced the criteria again and changed the name of the condition from "multiple personality disorder" to the current "dissociative identity disorder" to emphasize the importance of changes to consciousness and identity rather than personality. The inclusion of interpersonality amnesia helped to distinguish DID from [[dissociative disorder not otherwise specified]], but the condition retains an inherent subjectivity due to difficulty in defining terms such as personality, identity, ego-state and even [[amnesia]].<ref name = Kihlstrom>{{cite pmid | 17716088}}</ref> The [[ICD-10]] still classifies DID as a "Dissociative [conversion] disorder" and retains the name "multiple personality disorder" with the classification number of F44.8.81.<ref name = ICD10>{{cite web | url = http://www.who.int/classifications/icd/en/GRNBOOK.pdf | format = pdf | publisher = [[World Health Organization]] | title = The ICD-10 Classification of Mental and Behavioural Disorders }}</ref> |
||
In 1998 the publication of [[peer review]]ed [[meta-analysis]] of the self-reported harm caused by [[child sexual abuse]] (CSA) by two researchers caused a public debate, ''[[Rind et al. controversy]]''.<ref name = Rindetal>{{cite journal | title = A Meta-Analytic Examination of Assumed Properties of Child Sexual Abuse Using College Samples | url = http://digilib.bc.edu/reserves/sc563/mcgu/sc56310.pdf | journal = [[Psychological Bulletin]] | last = Rind| first = B | coauthors = Tromovitch P Bauserman R | volume = 124 | issue = 1 | pages = 22–53 | year = 1998 | pmid = 9670820 | doi = 10.1037/0033-2909.124.1.22 }}</ref> The paper was a follow-up and expansion of a 1997 meta-analysis by two of the paper's three authors caused debate unprecedented in the scientific community.<ref name = RindTromovitch>{{cite journal | last = Rind | first = B | coauthors = Tromovitch P | year = 1997 | title = A meta-analytic review of findings from national samples on psychological correlates of child sexual abuse | url = http://www.findarticles.com/p/articles/mi_m2372/is_n3_v34/ai_20444907 | journal = [[The Journal of Sex Research]] | volume = 34 | pages = 237–255 |jstor=3813384 | doi = 10.1080/00224499709551891 | issue = 3 }}</ref> The debate played out in the [[scientific literature]], public media, and government legislatures in the [[United States]]. Based on the results, those against the paper's findings concluded that the general consensus associating CSA with intense, pervasive harm and long-term [[mental disorder|maladjustment]] was incorrect.<ref name = RindTromovitch>{{cite journal | last = Rind | first = B | coauthors = Tromovitch P | year = 1997 | title = A meta-analytic review of findings from national samples on psychological correlates of child sexual abuse | url = http://www.findarticles.com/p/articles/mi_m2372/is_n3_v34/ai_20444907 | journal = [[The Journal of Sex Research]] | volume = 34 | pages = 237–255 |jstor=3813384 | doi = 10.1080/00224499709551891 | issue = 3 }}</ref> The debate resulted in the unprecedented condemnation of the paper by both Houses of the [[United States Congress]]. In September 1999 the [[American Association for the Advancement of Science]] (AAAS), upon a request by the APA to independently review the article, stated that it saw no reason to second-guess the peer review process that approved it initially and that it saw no evidence of improper methodology or questionable practices by the authors. The AAAS also expressed concern that the materials reviewed demonstrated a grave lack of understanding of the study on the part of the media and politicians and were also concerned about the misrepresentation of its findings.<ref name="Rind 2000 1–62">{{cite journal | url = http://www.springerlink.com/content/q771v3lq3x036122/ | last = Rind | first = B | coauthors = Tromovitch P; Bauserman R | year = 2000 | title = Condemnation of a scientific article: A chronology and refutation of the attacks and a discussion of threats to the integrity of science | journal = Sexuality and Culture | volume = 4 | issue = 2 | pages = 1–62 | doi = 10.1007/s12119-000-1025-5 }}</ref> The AAAS stated that the responsibility for discovering problems with the article lay with the initial peer reviewers, and declined to evaluate the article and concluded with a statement that the decision not to review the article was neither an endorsement, nor a criticism of it.<ref name = Lilienfeld2002>{{cite journal | last = Lilienfeld | first = SO | year = 2002 | url = http://www.haverford.edu/psych/ble/SciSoc/lilienfeld02.pdf | title = When Worlds Collide: Social Science, Politics and the Rind et al. (1998) Child Abuse Meta-Analysis | format = PDF | journal = [[The American Psychologist]] | volume = 57 | issue = 3 | pages = 177–187 |archiveurl = http://web.archive.org/web/20030429000006/http://www.haverford.edu/psych/ble/SciSoc/lilienfeld02.pdf |archivedate = 2003-04-29 | pmid=11905116}}</ref> |
|||
In August 2000, the APA drafted and adopted a position statement in response to the Rind et al. controversy which opposed any efforts to [[censorship|censor]] controversial or surprising research findings and asserting researchers must be free to investigate and report findings so long as the research has been conducted within appropriate ethical and research standards.<ref name = Lilienfeld2002/> |
|||
A 2006 study compared scholarly research and publications on DID and [[dissociative amnesia]] to other mental health conditions, such as [[anorexia nervosa]], [[alcohol abuse]] and [[schizophrenia]] from 1984 to 2003. The results were found to be unusually distributed, with a very low level of publications in the 1980s followed by a significant rise that peaked in the mid-1990s and subsequently rapidly declined in the decade following. Compared to 25 other diagnosis, the mid-90's "bubble" of publications regarding DID was unique. In the opinion of the authors of the review, the publication results suggest a period of "fashion" that waned, and that the two diagnoses "[did] not command widespread scientific acceptance".<ref name = Pope>{{cite pmid|16361871}}</ref> |
A 2006 study compared scholarly research and publications on DID and [[dissociative amnesia]] to other mental health conditions, such as [[anorexia nervosa]], [[alcohol abuse]] and [[schizophrenia]] from 1984 to 2003. The results were found to be unusually distributed, with a very low level of publications in the 1980s followed by a significant rise that peaked in the mid-1990s and subsequently rapidly declined in the decade following. Compared to 25 other diagnosis, the mid-90's "bubble" of publications regarding DID was unique. In the opinion of the authors of the review, the publication results suggest a period of "fashion" that waned, and that the two diagnoses "[did] not command widespread scientific acceptance".<ref name = Pope>{{cite pmid|16361871}}</ref> |
||
Revision as of 17:31, 9 August 2012
| Dissociative identity disorder | |
|---|---|
| Specialty | Psychiatry, psychology |
| Frequency | 1.5% (United States of America) |
Dissociative identity disorder (DID), also known as multiple personality disorder,[1] is a mental disorder characterized by at least two distinct and relatively enduring identities or dissociated personality states that alternately control a person's behavior, and is accompanied by memory impairment for important information not explained by ordinary forgetfulness. These symptoms are not accounted for by substance abuse, seizures, other medical condition or fantasy behavior in children.[2] Diagnosis is often difficult as there is considerable comorbidity with other mental disorders. Malingering should be ruled out if there is possible financial or forensic gain, as well as factitious disorder if help-seeking behavior is prominent.[2]
DID is one of the most controversial psychiatric disorders with no clear consensus regarding its diagnosis or treatment.[3] Research on treatment effectiveness still focuses mainly on clinical approaches and case studies. Dissociative symptoms range from common lapses in attention, becoming distracted by something else, and daydreaming, to pathological dissociative disorders.[4] No systematic, empirically-supported definition of "dissociation" exists.
Although neither epidemiological surveys nor longitudinal studies have been done, it is thought DID rarely resolves spontaneously. Symptoms are said to vary over time.[4] In general, the prognosis is poor, especially for those with co-morbid disorders.
There is little systematic data on the prevalence of DID.[5] Some evidence indicates a rate of between 1 and 3% in the general population, and between 1 and 5% in inpatient groups in Europe and North America.[6] DID is diagnosed more frequently in North America than in the rest of the world, and is 5 to 9 times more common in females than males.[7][8][5]
Traditionally dissociative disorders such as DID were attributed to trauma and other forms of stress that caused memory to separate or dissociate, but research on this hypothesis has been characterized by poor methodology. So far, experimental studies, usually focusing on memory, have been few and the research has been inconclusive.[9] It became a popular diagnosis in the 1970s but it is unclear if the actual incidence of the disorder increased or only its popularity. An alternative hypotheses for its etiology is that DID is a product of techniques employed by some therapists, especially those using hypnosis, and disagreement between the two positions is characterized by intense debate.[10][3] The unusual number of diagnoses after 1980, clustered around a small number of clinicians and the suggestibility characteristic of those with DID, support the hypothesis that DID is therapist-induced.[11] The unusual clustering of diagnoses has also been explained as due to a lack of awareness and training among clinicians to recognize cases of DID.[12]
Signs and symptoms
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM), DID includes "the presence of two or more distinct identities or personality states" that alternate control of the individual's behavior, accompanied by the inability to recall personal information beyond what is expected through normal forgetfulness. The diagnosis excludes symptoms caused by alcohol, drugs or medications and other medical conditions such as complex partial seizures and normal fantasy play in children.[2] In each individual, the clinical presentation, degree of symptom severity and level of daily functioning varies widely from severely impaired to normal to "highly effective".[12][13] The symptoms of dissociative amnesia, dissociative fugue and depersonalization disorder are subsumed under DID diagnosis and are not diagnosed separately. Individuals with DID may experience distress from the consequences of DID rather than from the symptoms themselves. [verification needed][14] The majority of patients with DID report a history of severe physical and sexual abuse during their childhood, though the accuracy of these reports is controversial.[4] Identities may be unaware of each other and compartmentalize knowledge and memories, resulting in chaotic personal lives.[13] Individuals with DID may be reluctant to share symptoms due to associations with abuse, shame and fear.[4]
The number of alters varies wildly, with most patients identifying fewer than ten, though as many as 4,500 have been reported. The primary personality, which often has the patients given name, tends to be "passive, dependent, guilty and depressed" with other personalities or "alters" being more active, aggressive or hostile, and often containing more complete memories. Most identities are of ordinary people, though fictional, mythical, celebrity and animal alters have also been reported.[15]
Co-morbid disorders
Most dissociative disorder cases have co-morbid mental disorders, with an average of 8 Axis I and 4.5 Axis II DSM diagnoses.[15] The psychiatric history frequently contains multiple previous diagnoses of various disorders and treatment failures.[16] Common Axis I co-morbidities include anxiety disorders such as posttraumatic stress disorder (PTSD) (up to 80%), social anxiety disorder (up to 75%), panic disorder (54-70%) and obsessive-compulsive disorder (up to 64%); mood disorders such as major depressive disorder (88-97%); substance-related disorders (50-65%); eating disorders such as bulimia nervosa (19-23%); and somatoform disorders (23–45%).[17] In addition, a majority of those diagnosed with DID meet the criteria for DSM axis II personality disorders such as borderline personality disorder;[18] a significant minority meet the criteria for avoidant personality disorder and other personality disorders.[19] Further, data supports a high level of psychotic symptoms in DID, and that both schizophrenia and DID have histories of trauma.[20] Individuals diagnosed with DID also demonstrate the highest hypnotizability of any clinical population.[14]
Borderline personality disorder
Between 50 and 66% of patients also meet the criteria for borderline personality disorder (BPD), and nearly 75% of patients with BPD also meet the criteria for DID with considerable overlap between the two conditions in terms of personality traits, cognitive and day-to-day functioning and ratings by clinicians. Both groups also report higher than general population rates of physical and sexual abuse, and patients with BPD also score highly on measures of dissociation.[15]
Causes
The cause of DID is controversial, with debate occurring between the developmental trauma model (which hypothesizes that DID develops over time as a result of trauma), the iatrogenic–sociocognitive (the hypotheses that DID is caused by therapeutic techinques in combination with societal factors) and newer hypotheses involving the neural processing of memory and the possibility that the trauma causing dissociation can occur after childhood in DID as it does posttraumatic stress disorder (PTSD). It has been suggested that all the trauma-based and stress-related disorders be placed in one category that would include both DID and PTSD.[21] Research is needed to determine the prevalence of the disorder in those who have never been in therapy, and the prevalence rates across cultures. These issues remain largely unaddressed.[22]
Developmental trauma
People diagnosed with DID often report that they have experienced severe physical and sexual abuse, especially during early to mid-childhood,[23] (although the accuracy of these reports has been disputed.[2]) and others report an early loss, serious medical illness or other traumatic events.[13] They also report more historical psychological trauma than those diagnosed with any other mental illness.[failed verification][24] Severe sexual, physical, or psychological trauma in childhood has been proposed as an explanation for its development; awareness, memories and emotions of harmful actions or events caused by the trauma are removed from consciousness, and alternate personalities or subpersonalities form with differing memories, emotions and behavior.[25] DID is attributed to extremes of stress or disorders of attachment. What may be expressed as posttraumatic stress disorder in adults may become DID when occurring in children, possibly due to their greater use of imagination as a form of coping.[14][18] Possibly due to developmental changes and a more coherent sense of self past the age of six, the experience of extreme trauma may result in different, though also complex dissociative symptoms and identity disturbances.[14] A specific relationship between childhood abuse, disorganized attachment and lack of social support are thought to be a necessary component of DID.[18] Other suggested explanations include insufficient childhood nurturing combined with the innate ability of children in general to dissociate memories or experiences from consciousness.[13]
Delinking early trauma from the etiology of dissociation has been explicitly rejected by those supporting the early trauma model. However, a 2012 review article supports the hypothesis that current or recent trauma may affect an individual's assessment of the more distant past, changing the experience of the past and resulting in dissociative states.[26] Giesbrecht et al. have suggested there is no actual empirical evidence linking early trauma to dissociation, and instead suggest that problems with neuropsychological functioning, such as increased distractibility in response to certain emotions and contexts, account for dissociative features.[27] A middle position hypothesizes that trauma, in some situations, alters neuronal mechanisms related to memory. Evidence is increasing that dissociative disorders are related both to a trauma history and to "specific neural mechanisms".[14] It has also been suggested that there may be a genuine but more modest link between trauma and DID, with early trauma causing increased fantasy-proneness, which may in turn render individuals more vulnerable to sociocognitive influences surrounding the development of DID.[28]
Therapist induced
It has been suggested that symptoms of DID may be created by therapists using techniques to "recover" memories with people who are suggestible (such as the use of hypnosis to "access" alter identities, facilitate age regression or retrieve memories).[29][10][12][11][22] Referred to as the "sociocognitive model" (SCM), it suggests that DID is due to a person consciously or unconsciously enacting social roles expected of people with their diagnosis,[22] with cues from behavior coming from unwitting therapists, improper therapeutic techniques, media portrayals of DID and sociocultural expectations of patients with DID.[28] The characteristics of people diagnosed with DID (hypnotizability, suggestibility, frequent fantasization and mental absorption) contributed to these concerns and concerns regarding the validity of recovered memories.[30] Skeptics note that a small subset of doctors are responsible for diagnosing the majority of individuals with DID.[10][11] Psychologist Nicholas Spanos and others skeptical of the condition have suggested that in addition to iatrogenesis, DID may be the result of role-playing rather than separate personalities, though others disagree, pointing to a lack of incentive to manufacture or maintain separate personalities and point to the claimed histories of abuse.[31] Proponents of the iatrogenic or sociocognitive position list a variety of arguments for the iatrogenic position, including the lack of children diagnosed with DID, the sudden spike in incidence after 1980 (although DID was not a diagnosis until DSM-IV published in 1994) in the absence of evidence of greater rates of child abuse, the appearance of the disorder almost exclusively in individuals undergoing psychotherapy (particularly involving hypnosis), the presences of bizarre alternate identities (such as those claiming to be animals or mythological creatures) and an increase in the number of alternate identities over time[11][28] (as well as an initial increase in their number as psychotherapy begins in DID-oriented therapy[28]). Proponents of the iatrogenic position see these various cultural and therapeutic causes as occurring within a context of pre-existing psychopathology, notably borderline personality disorder, which is commonly comorbid with DID.[28] In addition, presentations can vary across cultures, such as Indian patients who only switch alters after a period of sleep - which is commonly how DID is presented by the media within that country.[28]
The iatrogenic position is strongly linked to the False memory syndrome, coined by the False Memory Syndrome Foundation in reaction to memories recovered by a range of controversial therapies whose effectiveness is unproven. Such a memory could be used to make a false allegation of child sexual abuse. There is little consensus between the iatrogenic and traumagenic positions regarding DID.[3] Proponents of the iatrogenic position suggest a small number of clinicians diagnosing a disproportionate number of cases would provide evidence for their position[22] though it has also been claimed that higher rates of diagnosis in specific countries like the United States, may be due to greater awareness of DID. Lower rates in other countries may be due to an artificially low recognition of the diagnosis.[12]
In children
DID is rarely diagnosed in children. This fact is cited as a reason to doubt the validity of DID, and proponents of both etiologies believe that the discovery of DID in a child that had never undergone treatment would critically undermine the SCM. Conversely the development of DID only after undergoing treatment would challenge the traumagenic model.[22] To date approximately 250 cases of DID in children have been identified, though the data does not offer unequivocal support for either theory. While children have been diagnosed with DID before therapy, several were presented to clinicians by parents with the diagnosis; others were influenced by the appearance of DID in popular culture or due to a diagnosis of psychosis due to hearing voices - a symptom also found in DID. No studies have looked for children with DID in the general population, and the single study that attempted to look for children with DID not already in therapy did so by examining siblings of those already in therapy for DID. An analysis of diagnosis of children reported in scientific publications, 44 case studies of single patients were found to be evenly distributed (i.e. each case study was reported by a different author) but in articles regarding groups of patients, four researchers were responsible for the majority of the reports.[22]
Diagnosis
The American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM) diagnoses DID according to the diagnostic criteria found in in section 300.14 (dissociative disorders). The criteria require that an adult, for non-physiological reasons, be recurrently controlled by two or more discrete identities or personality states, accompanied by memory lapses for important information.[2] While otherwise similar, the diagnostic criteria for children also rules out fantasy. Diagnosis is normally performed by a clinically trained mental health professional such as a psychiatrist or psychologist through clinical evaluation, interviews with family and friends, and consideration of other ancillary material. Specially designed interviews (such as the SCID-D) and personality assessment tools may be used in the evaluation as well.[16] Since most of the symptoms depend on self report and are not concrete and observable, the result is a degree of subjectivity in making the diagnosis.[32] People are often disinclined to seek treatment, especially since their symptoms may not be taken seriously; thus dissociative disorders have been referred to as "diseases of hiddenness".[30][33]
The diagnosis has been criticized as proponents of the iatrogenic or sociocognitive hypothesis believe it as a culture-bound and often iatrogenic condition which they believe is in decline.[29][11][22] Other researchers disagree and argue that the condition is real and supported by convergent evidence and its inclusion in the DSM is supported by reliable and convergent evidence, with diagnostic criteria allowing it to be clearly discriminated from conditions it is often mistaken for (schizophrenia, borderline personality disorder and seizure disorder).[12] Since a large proportion of cases are diagnosed by specific clinicians, suggests to some that either those clinicians are indeed responsible for the iatrogenic creation of alters or there is a high rate of false positives due to subjective diagnostic criteria, though proponents of the traumagenic hypothesis believe there are valid and objective diagnostic criteria to identify individuals with DID.[22]
Screening
Perhaps due to their perceived rarity, the dissociative disorders (including DID) were not initially included in the Structured Clinical Interview for DSM-IV (SCID), which is designed to make psychiatric diagnoses more rigorous and reliable.[32] Instead, shortly after the publication of the initial SCID a freestanding protocol for dissociative disorders (SCID-D)[34] was published.[32] This interview takes about 30 to 90 minutes depending on the subject's experiences.[35] An alternative diagnostic instrument, the Dissociative Disorders Interview Schedule, also exists but the SCID-D is generally considered superior.[32] The Dissociative Disorders Interview Schedule (DDIS) is a highly structured interview that discriminates among various DSM-IV diagnoses. The DDIS can usually be administered in 30–45 minutes.[36]
Other questionnaires include the Dissociative Experiences Scale (DES), Perceptual Alterations Scale, Questionnaire on Experiences of Dissociation, Dissociation Questionnaire and the Mini-SCIDD. All are strongly intercorrelated and except the Mini-SCIDD, all incorporate absorption, a normal part of personality involving narrowing or broadening of attention.[32] The DES[37] is a simple, quick, and validated[38] questionnaire that has been widely used to screen for dissociative symptoms, with variations for children and adolescents. Tests such as the DES provide a quick method of screening subjects so that the more time-consuming structured clinical interview can be used in the group with high DES scores. Depending on where the cutoff is set, people who would subsequently be diagnosed can be missed. An early recommended cutoff was 15-20.[39] The reliability of the DES in non-clinical samples has been questioned.[40]
Differential diagnoses
People with DID are diagnosed with five to seven co-morbid disorders on average - much higher than other mental illnesses.[18] Due to overlap between symptoms, differential diagnosis between DID and a variety of other conditions (including schizophrenia, psychosis, normal and rapid-cycling bipolar disorder, anxiety disorders, somatization and personality disorders) can be complicated as delusions or auditory hallucinations can be mistaken for speech by other personalities and vice-versa (individuals with DID may also conceal these symptoms and avoid disclosing them during interviews to avoid being considered "crazy" or out of feelings of shame[14]), or sudden behavior changes being attributed to sudden mood fluctuations. Persistence and consistency of identities and behavior, amnesia, measures of dissociation or hypnotizability and reports from family members or other associates indicating a history of such changes can help distinguish DID from other conditions. A diagnosis of DID takes precedence over any other dissociative disorders. Distinguishing true DID from malingering is a concern when financial or legal gains are an issue, and factitious disorder may also be considered if there patient has a history or pattern help or attention seeking. Individuals who state that their symptoms are due to external spirits or entities entering their bodies are generally diagnosed with dissociative disorder not otherwise specified rather than DID due to the lack of internal personalities or alter states.[2] Most individuals who enter an emergency department and are unaware of their names are generally in a psychotic state rather dissociative. Auditory hallucinations are common, but complex visual hallucinations may also occur.[18] Though hallucinations can be experienced in any sensory system (visual, auditory, tactile, gustatory or olfactory),[14] patients generally have adequate reality testing to distinguish between reality and hallucinations, and lack the negative symptoms of schizophrenia.[12] In addition, individuals with psychosis are much less susceptible to hypnosis than those with DID.[14] Difficulties in differential diagnosis are increased in children.[22]
DID must be distinguished from, or determined if comorbid with, a variety of disorders including mood disorders, psychosis, anxiety disorders, posttraumatic stress disorder, personality disorders, cognitive disorders, neurological disorders, epilepsy, somatoform disorder, factitious disorder, malingering, other dissociative disorders and trance states.[5] Individuals faking or mimicking DID due to factitious disorder will exaggerate symptoms (particularly when observed), lie, blame bad behavior on symptoms and often show little distress regarding their apparent diagnosis. In contrast, genuine DID patients exhibit confusion, distress and shame regarding their symptoms and history.[5] The condition may be under-diagnosed due to skepticism and lack of awareness from mental health professionals, made difficult due to the lack of specific and reliable criteria for diagnosing DID as well as a lack of prevalence rates due to the failure to examine systematically selected and representative populations.[10][41] A specific relationship between DID and borderline personality disorder has been posited several times, with various clinicians noting significant overlap between symptoms and patient behaviors and it has been suggested that DID may arise "from a substrate of borderline traits." Reviews of DID patients and their medical records concluded that the majority of those diagnosed with DID would also meet the criteria for either borderline personality disorder or more generally borderline personality.[18]
History of the DSM diagnosis
The DSM-II used the term Hysterical Neurosis, Dissociative Type. It described the possible occurrence of alterations in the patient's state of consciousness or identity, and included the symptoms of "amnesia, somnambulism, fugue, and multiple personality."[42] The DSM-III grouped the diagnosis with the other four major dissociative disorders using the term "multiple personality disorder". The DSM-IV made more changes to DID than any other dissociative disorder,[12] and renamed it DID.[2] The name was changed for two reasons. First, to emphasize the main problem was not a multitude of personalities, but rather a lack of a single, unified identity[12] and an emphasis on "the identies as centers of information processing".[14] Second, the term "personality" is used to refer to "characteristic patterns of thoughts, feelings, moods and behaviors of the whole individual", while for a patient with DID, the switches between identities and behavior patterns is the personality.[12] It is for this reason the DSM-IV-TR referred to "distinct identities or personality states" instead of personalities. The diagnostic criteria also changed to indicate that while the patient may name and personalize alters, they lack an independent, objective existence.[12] The changes also included the addition of amnesia as a symptom, which was not included in the DSM-III-R because despite being a core symptom of the condition, patients may experience "amnesia for the amnesia" and fail to report it.[14] Amnesia was replaced when it became clear that the risk of false negative diagnoses was low because amnesia was central to DID.[12]
The ICD-10 places the diagnosis in the category of "dissociative disorders", within the subcategory of "other dissociative (conversion) disorders", but continues to list the condition as multiple personality disorder.[1]
The DSM-IV-TR criteria for DID have been criticized for failing to capture the clinical complexity of DID, lacking usefulness in diagnosing individuals with DID (for instance, by focusing on the two least frequent and most subtle symptoms of DID) producing a high rate of false negatives and an excessive number of DDNOS diagnoses, for excluding possession (seen as a cross-cultural form of DID), and for including only two "core" symptoms of DID (amnesia and self-alteration) while failing to discuss hallucinations, trance-like states, somatoform, depersonalization and derealization symptoms. Arguments have been made for allowing diagnosis through the presence of some, but not all of the characteristics of DID rather than the current exclusive focus on the two least common and noticeable features.[14] The DSM-V-TR criteria has also been criticized for being tautological, using imprecise and undefined language and for the use of instruments that give a false sense of validity and empirical certainty to the diagnosis.
Controversy
DID is a controversial diagnosis.[15] The primary dispute is between those who believe DID is caused by traumatic stresses forcing the mind to split into multiple identities, each with a separate set of memories,[32][9] and the belief that the symptoms of DID are produced artificially by certain psychotherapeutic practices or patients playing a role they believe appropriate for a patient suffering from from DID.[29][43][10][31][30][12] The debate between the two positions is characterized by intense disagreement.[29][10][31][12][3][11]
The initial theoretical description of DID was that dissociative symptoms were a means of coping with extreme stress (particularly childhood sexual and physical abuse), but this belief has been challenged by the data of multiple research studies.[28] Scholars have noted a lack of objective corroboration for abuse, with many studies using only self-reported trauma in cross-sectional studies, which may be worsened by selection and referral bias. In addition, the numerous other conditions comorbid with DID as well as family maladjustment are rarely controlled for.[28] The popular association of DID with childhood abuse is relatively recent, occurring only after the publication of Sybil in 1973. Most previous examples of "multiples" such as Chris Costner Sizemore, whose life was depicted in the book and film The Three Faces of Eve, disclosed no history of child abuse.[44] Psychiatrists August Piper and Harold Merskey have challenged the trauma hypothesis, arguing that correlation does not imply causation - the fact that people with DID report childhood trauma does not mean trauma causes DID - and point to the rareness of the diagnosis before 1980 as well as a failure to find DID as an outcome in longitudinal studies of traumatized children. They assert that DID cannot be accurately diagnosed because of vague and unclear diagnostic criteria in the DSM and undefined concepts such as "personality state" and "identities", and question the evidence for childhood abuse beyond self-reports, the lack of definition of what would indicate a threshold of abuse sufficient to induce DID and the extremely small number of cases of children diagnosed with DID despite an average age of appearance of the first alter of three years.[11] Psychiatrist Colin Ross disagrees with Piper and Merskey's conclusion that DID cannot be accurately diagnosed, pointing to internal consistency between different structured dissociative disorder interviews (including the Dissociative Experiences Scale, Dissociative Disorders Interview Schedule and Structured Clinical Interview for Dissociative Disorders)[32] that are in the internal validity range of widely accepted mental illnesses such as schizophrenia and major depressive disorder. In his opinion, Piper and Merskey are setting the standard of proof higher than they are for other diagnoses. He also asserts that Piper and Merskey have cherry-picked data and not incorporated all relevant scientific literature available, such as independent corroborating evidence of trauma.[45]
Richard J. McNally has explained in his 2005 book how he sees child abuse being politicized.[46]
Pathophysiology
Despite research on DID including structural and functional magnetic resonance imaging, positron emission tomography, single-photon emission computed tomography, event-related potential and electroencephalography, no convergent neuroimaging findings have been identified regarding DID, making it difficult to hypothesize a biological basis for DID. In addition, many of the studies that do exist were performed from an explicitly trauma-based position, and did not consider the possibility of iatrogenic induction of DID. There is no research to date regarding the neuroimaging and introduction of false memories in DID patients,[3] though there is evidence of changes in visual parameters[47] and support for amnesia between alters.[32][3] DID patients also appear to show deficiencies in tests of conscious control of attention and memorization (which also showed signs of compartmentalization for implicit memory between alters but no such compartmentalization for verbal memory) and increased and persistent vigilance and startle responses to sound. DID patients may also demonstrate altered neuroanatomy.[18] Experimental tests of memory suggest that patients with DID may have improved memory for certain tasks, which has been used to criticize the hypothesis that DID is a means of forgetting or suppressing memory. Patients also show experimental evidence of being more fantasy-prone, which in turn is related to a tendency to over-report false memories of painful events.[28]
Several of the terms used to diagnose DID (personality, ego state, identity and even amnesia) are undefined,[32] and the overall concept of dissociation itself is substantially undefined, with multiple competing models that incorporate some nondissociative symptoms while excluding dissociative ones. The most widely used model of dissociation is conceptualizes DID as one extreme end of a continuum of dissociation, with flow at the other end, though this model is being challeneged.[48] Psychiatrist Paulette Gillig draws distinction between an "ego state" (behaviors and experiences united by a common principle but possessing permeable boundaries with other such states) and the commonly used term "alters" (which have a separate autobiographical memory, independent initiative and sense of ownership over their own actions) described in DID.[18] Ellert Nijenhuis and colleagues suggest a distinction between personalities responsible for day-to-day functioning (associated with blunted physiological responses and reduced emotions, referred to as the "apparently normal part of the personality") and those emerging in survival situations (involving Fight or Flight reflexes, vivid traumatic memories and strong, painful emotions, the "emotional part of the personality").[49] Disturbed and altered sleep has also been suggested as having a role in dissociative disorders in general and DID in specific.[50]
Treatment
There is a general lack of consensus in the diagnosis and treatment of DID[3] and research on treatment effectiveness focuses mainly on clinical approaches described in case studies. General treatment guidelines exist that suggest a phased, eclectic approach with more concrete guidance and agreement on early stages but no systematic, empirically-supported approach exists and later stages of treatment are not well described and have no consensus. Even highly experienced therapists have few patients that achieve a unified identity.[51] Common treatment methods include an eclectic mix of psychotherapy techniques, including cognitive behavioral (CBT),[18] insight-oriented therapies,[32] dialectical behavioral therapy (DBT), hypnotherapy and eye movement desensitization and reprocessing (EMDR). Medications can be used for co-morbid disorders and/or targeted symptom relief.[6][30] Some behavior therapists initially use behavioral treatments such as only responding to a single identity, and then use more traditional therapy once a consistent response is established.[52] Brief treatment due to managed care may be difficult, as individuals diagnosed with DID may have unusual difficulties in trusting a therapist and take a prolonged period to form a comfortable therapeutic alliance.[6] Regular contact (weekly or biweekly) is more common, and treatment generally lasts years - not weeks or months.[6][18] Sleep hygiene has been suggested as a treatment option, but has not been tested. In general there are very few clinical trials on the treatment of DID, none of which were randomized controlled trials.[28]
Therapy for DID is generally phase oriented. Different alters may appear based on their greater ability to deal with specific situational stresses or threats. While some patients may initially present with a large number of alters, this number may reduce during treatment - though it is considered important for the therapist to become familiar with at least the more prominent personality states as the "host" personality may not be the "true" identity of the patient. Specific alters may react negatively to therapy, fearing the therapists goal is to eliminate the alter (particularly those associated with illegal or violent activities). A more realistic and appropriate goal of treatment is to integrate adaptive responses to abuse, injury or other threats into the overall personality structure.[18] There is debate over issues such as whether exposure therapy (reliving traumatic memories, also known as abrecation), engagement with alters and physical contact during therapy is appropriate and there are clinical opinions both for and against each option with little high-quality evidence for any position.
Brandt et al., noting the lack of empirical studies of treatment effectiveness, conducted a survey of 36 clinicians expert in treating dissociative disorder (DD) who recommended a three-stage treatment. They agreed that skill building in the first stage is important so the patient can learn to handle high risk, potentially dangerous behavior, as well as emotional regulation, interpersonal effectiveness and other practical behaviors. In addition, they recommended "trauma-based cognitive therapy" to reduce cognitive distortions related to trauma; they also recommended that the therapist deal with the dissociated identities early in treatment. In the middle stage, they recommended graded exposure techniques, along with appropriate interventions as needed. The treatment in the last stage was more individualized; few with DD [sic] became integrated into one identity.[51]
The International Society for the Study of Trauma and Dissociation has published guidelines to phase-oriented treatment in adults as well as children and adolescents that are widely used in the field of DID treatment.[non-primary source needed][6] The first phase of therapy focuses on symptoms and relieving the distressing aspects of the condition, ensuring the safety of the individual, improving the patient's capacity to form and maintain healthy relationships, and improving general daily life functioning. Co-morbid disorders such as substance abuse and eating disorders are addressed in this phase of treatment.[6] The second phase focuses on stepwise exposure to traumatic memories and prevention of re-dissociation. The final phase focuses on reconnecting the identities of disparate alters into a single functioning identity with all its memories and experiences intact.[6]
A study was conducted with the goal of developing an "expertise-based prognostic model for the treatment of complex posttraumatic stress disorder (PTSD) and dissociative identity disorder (DID)." Researchers constructed a two-stage survey and factor analyses performed on the survey elements found 51 factors common to complex PTSD and DID. The authors concluded from their findings: "The model is supportive of the current phase-oriented treatment model, emphasizing the strengthening of the therapeutic relationship and the patient's resources in the initial stabilization phase. Further research is needed to test the model's statistical and clinical validity."[53]
Prognosis
The prognosis of untreated DID is not well known.[5] It rarely if ever goes away without treatment[4][13] but symptoms may resolve from time to time[4] or wax and wane spontaneously.[13] Patients with mainly dissociative and posttraumatic symptoms face a better prognosis than those with comorbid disorders or those still in contact with abusers, and the latter groups often face lengthier and more difficult treatment. Suicidal ideation, failed suicide attempts and self-harm also occur.[13] Duration of treatment can vary depending on patient goals, which can extend from elimination of all alters to merely reducing inter-alter amnesia, but generally takes years.[13]
Epidemiology
There is little systematic data on the prevalence of DID.[54] It occurs more commonly in young adults[54] and declines with age.[55] Reported rates in the community vary from 1% to 3% with higher rates among psychiatric patients.[12][6] It is 5 to 9 times more common in females than males during young adulthood.[5] In children rates among females and males are neither the same (5:4).[4]
Though the condition has been described in non-English speaking nations and non-Western cultures, these reports all occur in English-language journals authored by international researchers who cite Western scientific literature and are therefore not isolated from Western influences.[22]
DID diagnoses are extremely rare in children; much of the research on childhood DID occurred in the 1980s and 1990s and does not address ongoing controversies surrounding the diagnosis.[22]
Changing prevalence
Rates of diagnosed DID have been increasing.[4] Initially DID along with the rest of the dissociative disorders were considered the rarest of psychological conditions, numbering less than 100 by 1944, with only one further case added in the next two decades.[32] In the late 1970s and 80s, the number of diagnoses rose sharply.[32] Estimate from the 1980s where 0.01%.[4] Accompanying this rise was an increase in the number of alters, rising from only the primary and one alter personality in most cases, to an average of 13 in the mid-1980s (the increase in both number of cases and number of alters within each case are both factors in professional skepticism regarding the diagnosis).[32] Others explain the increase as being due to the use of inappropriate therapeutic techniques in highly suggestible individuals, though this is itself controversial.[10][31] Figures from psychiatric populations (inpatients and outpatients) show a wide diversity from different countries:[56]
North America
The DSM does not provide an estimate of incidence for DID and dissociative disorders were excluded from the Epidemiological Catchment Area Project. As a result, there are no national statistics for incidence and prevalence of DID in the United States.[32]
DID is a controversial diagnosis and condition, with much of the literature on DID still being generated and published in North America, to the extent that it was once regarded as a phenomenon confined to that continent[8][29] though research has appeared discussing the appearance of DID in other countries and cultures.[57] A 1996 review offered three possible causes for the sudden increase in people diagnosed with DID:[7]
- The result of therapist suggestions to suggestible people, much as Charcot's hysterics acted in accordance with his expectations.
- Psychiatrists' past failure to recognize dissociation being redressed by new training and knowledge.
- Dissociative phenomena are actually increasing, but this increase only represents a new form of an old and protean entity: "hysteria".
Paris believes that the first possible cause is the most likely. Etzel Cardena and David Gleaves believe the over-representation of DID in North America is the result of increased awareness and training about the condition which had formerly been missing.[12]
History


Before the 19th century, people exhibiting symptoms similar to those were believed to be possessed.[5] The first case of DID was thought to be described by Paracelsus in 1646.[58] In the 19th century "dédoublement" or double consciousness, the historical precursor to DID, was frequently described as a state of sleepwalking, with scholars hypothesizing that the patients were switching between a normal consciousness and a "sonambulistic state".[50]
An intense interest in spiritualism, parapsychology, and hypnosis continued throughout the 19th and early 20th centuries,[8] running in parallel with John Locke's views that there was an association of ideas requiring the coexistence of feelings with awareness of the feelings.[59] Hypnosis, which was pioneered in the late 18th century by Franz Mesmer and Armand-Marie Jacques de Chastenet, Marques de Puységur, challenged Locke's association of ideas. Hypnotists reported what they thought were second personalities emerging during hypnosis and wondered how two minds could coexist.[8]
The 19th century saw a number of reported cases of multiple personalities which Rieber[59] estimated would be close to 100. Epilepsy was seen as a factor in some cases,[59] and discussion of this connection continues into the present era.[60][61]
By the late 19th century there was a general acceptance that emotionally traumatic experiences could cause long-term disorders which might display a variety of symptoms.[62] These conversion disorders were found to occur in even the most resilient individuals, but with profound effect in someone with emotional instability like Louis Vivé (1863-?) who suffered a traumatic experience as a 13-year-old when he encountered a viper. Vivé was the subject of countless medical papers and became the most studied case of dissociation in the 19th century.
Between 1880 and 1920, many great international medical conferences devoted a lot of time to sessions on dissociation.[63] It was in this climate that Jean-Martin Charcot introduced his ideas of the impact of nervous shocks as a cause for a variety of neurological conditions. One of Charcot's students, Pierre Janet, took these ideas and went on to develop his own theories of dissociation.[64] One of the first individuals diagnosed with multiple personalities to be scientifically studied was Clara Norton Fowler, under the pseudonym Christine Beauchamp; American neurologist Morton Prince studied Fowler between 1898 and 1904, describing her case study in his 1906 monograph, Dissociation of a Personality.[64]
In the early 20th century interest in dissociation and multiple personalities waned for a number of reasons. After Charcot's death in 1893, many of his so-called hysterical patients were exposed as frauds, and Janet's association with Charcot tarnished his theories of dissociation.[8] Sigmund Freud recanted his earlier emphasis on dissociation and childhood trauma.[8]
In 1910, Eugen Bleuler introduced the term schizophrenia to replace dementia praecox. A review of the Index medicus from 1903 through 1978 showed a dramatic decline in the number of reports of multiple personality after the diagnosis of schizophrenia became popular, especially in the United States.[65] A number of factors helped create a large climate of skepticism and disbelief; paralleling the increased suspicion of DID was the decline of interest in dissociation as a laboratory and clinical phenomenon.[63]
Starting in about 1927, there was a large increase in the number of reported cases of schizophrenia, which was matched by an equally large decrease in the number of multiple personality reports.[63] Bleuler also included multiple personality in his category of schizophrenia. It was concluded in the 1980s that DID patients are often misdiagnosed as suffering from schizophrenia.[63]
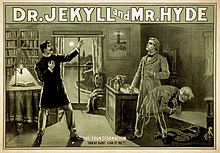
The public, however, was exposed to psychological ideas which took their interest. Mary Shelley's Frankenstein, Robert Louis Stevenson's Strange Case of Dr Jekyll and Mr Hyde, and many short stories by Edgar Allan Poe had a formidable impact.[59] In 1957, with the publication of the book The Three Faces of Eve and the popular movie which followed it, the American public's interest in multiple personality was revived. During the 1970s an initially small number of clinicians campaigned to have it considered a legitimate diagnosis.[63]
Between 1968 and 1980 the term that was used for dissocative identity disorder was "Hysterical neurosis, dissociative type". The APA wrote in the second edition of the DSM: "In the dissociative type, alterations may occur in the patient's state of consciousness or in his identity, to produce such symptoms as amnesia, somnambulism, fugue, and multiple personality."[42] The number of cases sharply increased in the late 1970s and throughout the 80s, and the first scholarly monographs on the topic appeared in 1986.[32]
In 1974 the highly influential book Sybil was published, and later made into a miniseries in 1976 and again in 2007. Describing what Robert Rieber called “the third most famous of multiple personality cases”,[66] it presented a detailed discussion of the problems of treatment of “Sybil”, a pseudonym for Shirley Ardell Mason. Though the book and subsequent films helped popularize the diagnosis, later analysis of the case suggested different interpretations, ranging from Mason’s problems being iatrogenically induced through therapeutic methods used by her psychiatrist, Cornelia B. Wilbur or an inadvertent hoax due in part to the lucrative publishing rights,[66][67] though this conclusions has itself been challenged.[68] As media attention on DID increased, so too did the controversy surrounding the diagnosis.[58]
With the publication of the DSM-III, which omitted the terms "hysteria" and "neurosis" (and thus the former categories for dissociative disorders), dissociative diagnoses became "orphans" with their own categories[69] with dissociative identity disorder appearing as "multiple personality disorder".[32] In the opinion of McGill University psychiatrist Joel Paris, this inadvertently legitimized them by forcing textbooks, which mimicked the structure of the DSM, to include a separate chapter on them and resulted in an increase in diagnosis of dissociative conditions. Once a rarely occurring spontaneous phenomena (research in 1944 showed only 76 cases),[70] became "an artifact of bad (or naïve) psychotherapy" as patients capable of dissociating were accidentally encouraged to express their symptoms by "overly fascinated" therapists.[69]
"Interpersonality amnesia" was removed as a diagnostic feature from the DSM III in 1987, which may have contributed to the increasing frequency of the diagnosis.[32] There were 200 reported cases of DID as of 1980, and 20,000 from 1980 to 1990.[71] Joan Acocella reports that 40,000 cases were diagnosed from 1985 to 1995.[72] Scientific publications regarding DID peaked in the mid-1990s then rapidly declined.[73]
In 1994, the fourth edition of the DSM replaced the criteria again and changed the name of the condition from "multiple personality disorder" to the current "dissociative identity disorder" to emphasize the importance of changes to consciousness and identity rather than personality. The inclusion of interpersonality amnesia helped to distinguish DID from dissociative disorder not otherwise specified, but the condition retains an inherent subjectivity due to difficulty in defining terms such as personality, identity, ego-state and even amnesia.[32] The ICD-10 still classifies DID as a "Dissociative [conversion] disorder" and retains the name "multiple personality disorder" with the classification number of F44.8.81.[1]
A 2006 study compared scholarly research and publications on DID and dissociative amnesia to other mental health conditions, such as anorexia nervosa, alcohol abuse and schizophrenia from 1984 to 2003. The results were found to be unusually distributed, with a very low level of publications in the 1980s followed by a significant rise that peaked in the mid-1990s and subsequently rapidly declined in the decade following. Compared to 25 other diagnosis, the mid-90's "bubble" of publications regarding DID was unique. In the opinion of the authors of the review, the publication results suggest a period of "fashion" that waned, and that the two diagnoses "[did] not command widespread scientific acceptance".[73]
Society and culture
Despite its rareness, DID is portrayed with remarkable frequency in popular culture, producing or appearing in numerous books, films and television shows.[31]
Psychiatrist Colin A. Ross has stated that based on documents obtained through freedom of information legislation, psychiatrists linked to Project MKULTRA claimed to be able to deliberately induce dissociative identity disorder using a variety of aversive techniques.[75]
Surveys of the attitudes of Canadian and American psychiatrists' attitudes towards dissociative disorders completed in 1999[43] and 2001[76] found considerable skepticism and disagreement regarding the research base of dissociative disorders in general and DID in specific, as well as whether the inclusion DID in the DSM was appropriate.
Legal issues
Within legal circles, DID has been described as one of the most disputed psychiatric diagnoses and forensic assessments.[3] The number of court cases involving DID has increased substantially since the 1990s[77] and the diagnosis presents a variety of challenges for legal systems. Courts must distinguish individuals who mimic symptoms of DID for legal or social reasons. Within jurisprudence there are three significant problems:[3]
- Individuals diagnosed with DID may accuse others of abuse but lack objective evidence and base their accusations solely on regular or recovered memories.
- There are questions regarding the civil and political rights of alters, particularly which alter can legally represent the person, sign a contract or vote.
- Finally, individuals diagnosed with DID who are accused of crimes may deny culpability due to the crime being committed by a different identity state.
In cases where not guilty by reason of insanity (NGRI) is used as a defence in a court, it is normally accompanied by one of three legal approaches - claiming a specific alter was in control when the crime was committed (and if that alter is considered insane), deciding whether all (or which) alters may be insane, or whether only the dominant personality meets the insanity standard.[58] NGRI is rarely successful for individuals with DID accused of committing crimes while in a dissociated states.[78]
There is no agreement within the legal and mental health fields whether an individual can be acquitted due to a diagnosis of DID. It has been argued that any individual with DID is a single person with a serious mental illness and therefore exhibits diminished responsibility and this was first recognized in an American court in 1978 (State v. Milligan). However, public reaction to the result of the case was strongly negative and since that time the few cases claiming insanity have found that the altered consciousness found in DID is either irrelevant or the diagnosis was not admissible evidence.[58] The self-reported nature of the symptoms used to reach a diagnosis makes it difficult to determine their credibility, although objective measuring of brain activation and structural patterns are a promising direction for future scientific research into distinguishing malingered from genuine DID in forensic settings.[3] Forensic experts called on to conduct forensic examinations for DID must use a multidisciplinary approach including multiple screening instruments.[58]
See also
Footnotes
- ^ a b c "The ICD-10 Classification of Mental and Behavioural Disorders" (pdf). World Health Organization.
- ^ a b c d e f g American Psychiatric Association (2000-06). Diagnostic and Statistical Manual of Mental Disorders-IV (Text Revision). Arlington, VA, USA: American Psychiatric Publishing, Inc. pp. 526–529. doi:10.1176/appi.books.9780890423349. ISBN 978-0-89042-024-9.
{{cite book}}: Check date values in:|date=(help) - ^ a b c d e f g h i j Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18569730 , please use {{cite journal}} with
|pmid= 18569730instead. - ^ a b c d e f g h i Maldonado, JR (2008). "Dissociative disorders - Dissociative identity disorder (Multiple personality disorder)". The American Psychiatric Publishing textbook of psychiatry (5th ed.). Washington, DC: American Psychiatric Pub. pp. 681-710. ISBN 9781585622573.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|editors=ignored (|editor=suggested) (help) - ^ a b c d e f g Sadock, BJ (2007). "Dissociative disorders — Dissociative identity disorder". Kaplan & Sadock's synopsis of psychiatry: behavioral sciences/clinical psychiatry (10th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 671–6. ISBN 9780781773270.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c d e f g h Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1080/15299732.2011.537248, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1080/15299732.2011.537248instead. - ^ a b Paris J (1996). "Review-Essay : Dissociative Symptoms, Dissociative Disorders, and Cultural Psychiatry". Transcult Psychiatry. 33 (1): 55–68. doi:10.1177/136346159603300104.
- ^ a b c d e f Atchison M, McFarlane AC (1994). "A review of dissociation and dissociative disorders". The Australian and New Zealand journal of psychiatry. 28 (4): 591–9. doi:10.3109/00048679409080782. PMID 7794202.
- ^ a b Howell, E (2010). "Dissociation and dissociative disorders: commentary and context". Knowing, not-knowing and sort-of-knowing: psychoanalysis and the experience of uncertainty. Karnac Books. pp. 83–98. ISBN 1-85575-657-9.
{{cite book}}: Unknown parameter|editors=ignored (|editor=suggested) (help) Cite error: The named reference "Howell" was defined multiple times with different content (see the help page). - ^ a b c d e f g Rubin, EH (2005). Adult psychiatry: Blackwell's neurology and psychiatry access series (2nd ed.). John Wiley & Sons. pp. 280. ISBN 1-4051-1769-9.
{{cite book}}: Unknown parameter|editors=ignored (|editor=suggested) (help) - ^ a b c d e f g Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15560314 , please use {{cite journal}} with
|pmid= 15560314instead. - ^ a b c d e f g h i j k l m n o Cardena E; Gleaves DH (2007). "Dissociative Disorders". In Hersen M; Turner SM; Beidel DC (ed.). Adult Psychopathology and Diagnosis. John Wiley & Sons. pp. 473–503. ISBN 978-0-471-74584-6.
{{cite book}}: CS1 maint: multiple names: authors list (link) Cite error: The named reference "Cardena" was defined multiple times with different content (see the help page). - ^ a b c d e f g h Simeon, D (2008). "Dissociative Identity Disorder". Merck & Co. Retrieved 2012-07-31.
- ^ a b c d e f g h i j k Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1002/da.20874 , please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1002/da.20874instead. - ^ a b c d Lynn, SJ (2012). "14 - Dissociative disorders". Adult Psychopathology and Diagnosis. John Wiley & Sons. pp. 497-538. ISBN 1118138821.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|editors=ignored (|editor=suggested) (help) - ^ a b Johnson, K (2012-05-26). "Dissociative Identity Disorder (Multiple Personality Disorder): Signs, Symptoms, Treatment". WebMD. Retrieved 2012-08-03.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15912905 , please use {{cite journal}} with
|pmid= 15912905instead. - ^ a b c d e f g h i j k Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19724751, please use {{cite journal}} with
|pmid= 19724751instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 8912944, please use {{cite journal}} with
|pmid=8912944instead. - ^ Foote B, Park J (2008). "Dissociative identity disorder and schizophrenia: differential diagnosis and theoretical issues". Current Psychiatry Reports. 10 (3): 217–22. PMID 18652789.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1080/15299731003780788 , please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1080/15299731003780788instead. - ^ a b c d e f g h i j k Boysen, GA (2011). "The scientific status of childhood dissociative identity disorder: a review of published research". Psychotherapy and psychosomatics. 80 (6): 329–34. doi:10.1159/000323403. PMID 21829044.
- ^ "Dissociative Identity Disorder, patient's reference". Merck.com. 2003-02-01. Retrieved 2007-12-07.
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1155/2011/404538, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1155/2011/404538instead. - ^ Carson VB (2006). Foundations of Psychiatric Mental Health Nursing: A Clinical Approach (5 ed.). St. Louis: Saunders Elsevier. pp. 266–267. ISBN 1-4160-0088-7.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 22423434 , please use {{cite journal}} with
|pmid= 22423434instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 18729565 , please use {{cite journal}} with
|pmid=18729565instead. - ^ a b c d e f g h i j Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1177/0963721411429457 , please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1177/0963721411429457instead. - ^ a b c d e Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 15503730 , please use {{cite journal}} with
|pmid= 15503730instead. - ^ a b c d MacDonald, K (2008). "Dissociative disorders unclear? Think 'rainbows from pain blows'" (pdf). Current Psychiatry. 7 (5): 73–85.
- ^ a b c d e Weiten, W (2010). Psychology: Themes and Variations (8 ed.). Cengage Learning. pp. 461. ISBN 0-495-81310-9.
- ^ a b c d e f g h i j k l m n o p q r Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17716088, please use {{cite journal}} with
|pmid= 17716088instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16585425 , please use {{cite journal}} with
|pmid= 16585425instead. - ^ Steinberg M, Rounsaville B, Cicchetti DV (1990). "The Structured Clinical Interview for DSM-III-R Dissociative Disorders: preliminary report on a new diagnostic instrument". The American Journal of Psychiatry. 147 (1): 76–82. PMID 2293792.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Steinberg, Marlene (1993). Structured clinical interview for DSM-IV dissociative disorders / Marlene Steinberg. Washington, DC: American Psychiatric Press. ISBN 0-88048-562-0.
- ^ Ross CA, Helier S, Norton R, Anderson D, Anderson G, Barchet P (1989). "The Dissociative Disorders Interview Schedule: A Structured Interview" (PDF). Dissociation. 2 (3): 171.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Bernstein EM, Putnam FW (1986). "Development, reliability, and validity of a dissociation scale". J. Nerv. Ment. Dis. 174 (12): 727–35. doi:10.1097/00005053-198612000-00004. PMID 3783140.
- ^ Carlson EB; Putnam FW; Ross CA; et al. (1993). "Validity of the Dissociative Experiences Scale in screening for multiple personality disorder: a multicenter study". The American Journal of Psychiatry. 150 (7): 1030–6. PMID 8317572.
{{cite journal}}: Unknown parameter|author-separator=ignored (help) - ^ Steinberg M, Rounsaville B, Cicchetti D (1991). "Detection of dissociative disorders in psychiatric patients by a screening instrument and a structured diagnostic interview". The American Journal of Psychiatry. 148 (8): 1050–4. PMID 1853955.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wright DB, Loftus EF (1999). "Measuring dissociation: comparison of alternative forms of the dissociative experiences scale". The American journal of psychology. 112 (4). The American Journal of Psychology, Vol. 112, No. 4: 497–519. doi:10.2307/1423648. JSTOR 1423648. PMID 10696264. Page 1
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19893342 , please use {{cite journal}} with
|pmid= 19893342instead. - ^ a b American Psychiatric Association (1968). "Hysterical Neurosis". Diagnostic and statistical manual of mental disorders second edition (PDF). Washington, D.C. p. 40.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 9989574, please use {{cite journal}} with
|pmid= 9989574instead. - ^ McNally 2005, p. 11.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19306208, please use {{cite journal}} with
|pmid= 19306208instead. - ^ McNally 2005, p. 420.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 8888853 , please use {{cite journal}} with
|pmid=8888853instead. - ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1017/S1754470X11000031, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1017/S1754470X11000031instead. - ^ Nijenhuis, E (2010). "Trauma-related structural dissociation of the personality" (pdf). Activitas Nervosa Superior. 52 (1): 1–23.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1177/1745691612437597 , please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1177/1745691612437597instead. - ^ a b Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi: 10.1037/a0026487, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi= 10.1037/a0026487instead. - ^ Kohlenberg, R.J. (1991). Functional Analytic Psychotherapy: Creating Intense and Curative Therapeutic Relationships. Springer. ISBN 0-306-43857-7.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21240739, please use {{cite journal}} with
|pmid= 21240739instead. - ^ a b Sadock, BJ (2008). "Dissociative disorders - Dissociative identity disorder". Kaplan & Sadock's concise textbook of clinical psychiatry (3rd ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 299–300. ISBN 9780781787468.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Thornhill, JT (2011-05-10). Psychiatry (6 ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 169. ISBN 9781608315741.
- ^ Boon S, Draijer N (1991). "Diagnosing dissociative disorders in The Netherlands: a pilot study with the Structured Clinical Interview for DSM-III-R Dissociative Disorders". The American Journal of Psychiatry. 148 (4): 458–62. PMID 2006691.
- ^ Trauma And Dissociation in a Cross-cultural Perspective: Not Just a North American Phenomenon. Routledge. 2006. ISBN 978-0-7890-3407-6.
{{cite book}}: Unknown parameter|editors=ignored (|editor=suggested) (help) - ^ a b c d e Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21908758 , please use {{cite journal}} with
|pmid= 21908758instead. - ^ a b c d Rieber RW (2002). "The duality of the brain and the multiplicity of minds: can you have it both ways?". History of Psychiatry. 13 (49 Pt 1): 3–17. doi:10.1177/0957154X0201304901. PMID 12094818.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 6427406, please use {{cite journal}} with
|pmid= 6427406instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 2725878, please use {{cite journal}} with
|pmid= 2725878instead. - ^ Borch-Jacobsen M, Brick D (2000). "How to predict the past: from trauma to repression". History of Psychiatry. 11 (41 Pt 1): 15–35. doi:10.1177/0957154X0001104102. PMID 11624606.
- ^ a b c d e Putnam, Frank W. (1989). Diagnosis and Treatment of Multiple Personality Disorder. New York: The Guilford Press. p. 351. ISBN 0-89862-177-1.
- ^ a b van der Kolk BA, van der Hart O (1989). "Pierre Janet and the breakdown of adaptation in psychological trauma". Am J Psychiatry. 146 (12): 1530–40. PMID 2686473.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Rosenbaum M (1980). "The role of the term schizophrenia in the decline of diagnoses of multiple personality". Arch. Gen. Psychiatry. 37 (12): 1383–5. doi:10.1001/archpsyc.1980.01780250069008. PMID 7004385.
- ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11623821, please use {{cite journal}} with
|pmid= 11623821instead. - ^ Nathan, D (2011). Sybil Exposed. Free Press. ISBN 978-1-4391-6827-1.
- ^ Lawrence, M (2008). "Review of Bifurcation of the Self: The history and theory of dissociation and its disorders". American Journal of Clinical Hypnosis. 50 (3): 273–283.
- ^ a b Paris, J (2008). Prescriptions for the mind: a critical view of contemporary psychiatry. Oxford University Press. pp. 92. ISBN 0-19-531383-6.
- ^ "Creating Hysteria by Joan Acocella". The New York Times. 1999.
- ^ PMID 7788115
- ^ Acocella, JR (1999). Creating hysteria: Women and multiple personality disorder. San Francisco: Jossey-Bass Publishers. ISBN 0-7879-4794-6.
- ^ a b Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16361871, please use {{cite journal}} with
|pmid=16361871instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19742237, please use {{cite journal}} with
|pmid= 19742237instead. - ^ Ross, C (2000). Bluebird: Deliberate Creation of Multiple Personality Disorder by Psychiatrists. Manitou Communications. ISBN 978-0-9704525-1-1.
- ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 11441778, please use {{cite journal}} with
|pmid= 11441778instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 16530592, please use {{cite journal}} with
|pmid= 16530592instead. - ^ Farrell, HM (2011). "Dissociative identity disorder: No excuse for criminal activity" (pdf). Current Psychiatry. 10 (6): 33–40.
