Anorexia nervosa
| Anorexia nervosa | |
|---|---|
| Specialty | Psychiatry, clinical psychology |
Anorexia nervosa is an illness characterized by extremely low body weight and body image distortion with an obsessive fear of gaining weight. Individuals with anorexia nervosa are known to control body weight commonly through the means of voluntary starvation, excessive exercise, or other weight control measures such as diet pills or diuretic drugs. Although the condition primarily affects adolescent females, approximately 10% of people with the diagnosis are male.[1] Anorexia nervosa, involving neurobiological, psychological, and sociological components[2], is a complex condition that can lead to death in the most severe cases.
The term anorexia is of Greek origin: a (α, prefix of negation), n (ν, link between two vowels) and orexis (ορεξις, appetite), thus meaning a lack of desire to eat.[3]
"Anorexia nervosa" is frequently shortened to "anorexia" in the popular media. This is technically incorrect, as the term "anorexia" used separately refers to the medical symptom of reduced appetite (which therefore is distinguishable from anorexia nervosa in being non-psychiatric).
Definition
A definition of anorexia nervosa was established by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) and the World Health Organization's International Statistical Classification of Diseases and Related Health Problems (ICD).
DSM-IV-TR criteria are:
- Refusal to maintain body weight at or above a minimally normal weight for age and height (e.g. weight loss leading to maintenance of body weight less than 85% of that expected; or failure to make expected weight gain during period of growth, leading to body weight less than 85% of that expected).
- Intense fear of gaining weight or becoming fat, even though underweight.
- Disturbance in the way in which one's body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight.
- In postmenarcheal females, amenorrhea, i.e., the absence of at least three consecutive menstrual cycles. (A woman is considered to have amenorrhea if her periods occur only following hormone, e.g., estrogen, administration.)
Furthermore, the DSM-IV-TR specifies two subtypes:
- Restricting Type: during the current episode of anorexia nervosa, the person has not regularly engaged in binge-eating or purging behavior (that is, self-induced vomiting, or the misuse of laxatives, diuretics, or enemas). Weight loss is accomplished primarily through dieting, fasting, or excessive exercise.
- Binge-Eating Type or Purging Type: during the current episode of anorexia nervosa, the person has regularly engaged in binge-eating OR purging behavior (that is, self-induced vomiting, or the misuse of laxatives, diuretics, or enemas).
The ICD-10 criteria are similar, but in addition, specifically mention
- The ways that individuals might induce weight-loss or maintain low body weight (avoiding fattening foods, self-induced vomiting, self-induced purging, excessive exercise, excessive use of appetite suppressants or diuretics).
- Certain physiological features, including "widespread endocrine disorder involving hypothalamic-pituitary-gonadal axis is manifest in women as amenorrhoea and in men as loss of sexual interest and potency. There may also be elevated levels of growth hormones, raised cortisol levels, changes in the peripheral metabolism of thyroid hormone and abnormalities of insulin secretion".
- If onset is before puberty, that development is delayed or arrested.
There are a number of features that, although not necessarily diagnostic of anorexia, have been found to be commonly (but not exclusively) present in those with this eating disorder.[2][4][5]
Changes in brain structure and function are early signs often to be associated with starvation, and is partially reversed when normal weight is regained.[6] Anorexia is also linked to reduced blood flow in the temporal lobes, although since this finding does not correlate with current weight, it is possible that it is a risk trait rather than an effect of starvation.[7]
Diagnostic issues and controversies
The distinction between the diagnoses of anorexia nervosa, bulimia nervosa and eating disorder not otherwise specified (EDNOS) is often difficult to make in practice and there is considerable overlap between patients diagnosed with these conditions. Furthermore, seemingly minor changes in a patient's overall behavior or attitude (such as reported feeling of "control" over any binging behavior) can change a diagnosis from "anorexia: binge-eating type" to bulimia nervosa. It is not unusual for a person with an eating disorder to "move through" various diagnoses as his or her behavior and beliefs change over time.[4]
A person need not meet all diagnostic criteria for anorexia nervosa for their health and/or life to be in jeopardy; those with only some symptoms can still face permanent damage to their bodies, and even death.
Feminist writers such as Susie Orbach and Naomi Wolf have criticized the medicalization of extreme dieting and weight-loss as locating the problem within the affected women, rather than in a society that imposes concepts of unreasonable and unhealthy thinness as a measure of female beauty and gaining weight. Other writers have suggested that the disorder relates to issues of self-perception that are deeper than concerns with beauty and public perception.[8]
A vigorous debate exists on the topic of whether eating disorders are a choice or a biological illness.[citation needed] In 2006, Dr. Thomas Insel, director of the US National Institute of Mental Health, wrote an open letter to the National Eating Disorder Association stating "eating disorders are brain disorders."
Causes and contributory factors
It is clear that there is no single cause for anorexia and that it stems from a mixture of biological, social, and psychological factors. Current research is commonly focused on explaining existing factors and uncovering new causes. However, there is considerable debate over how much each of the known causes contributes to the development of anorexia. In particular, the contribution of perceived media pressure on women to be thin has been especially contentious.[9]
Genetic factors
Family and twin studies have suggested that genetic and environmental factors account for 74% and 26% of the variance in anorexia nervosa, respectively.[10] This evidence suggests that genes influencing both eating regulation, and personality and emotion, may be important contributing factors. In one study, variations in the norepinephrine transporter gene promoter were associated with restrictive anorexia nervosa, but not binge-purge anorexia (though the latter may have been due to small sample size).[11]
Several rodent models of anorexia have been developed which largely involve subjecting the animals to various environmental stressors or using gene knockout mice to test hypotheses about the effects of certain genes.[12] These models have suggested that the hypothalamic-pituitary-adrenal axis may be a contributory factor. However, these models have been criticised as food is being limited by the experimenter and not the animal and cannot take into account the complex cultural factors known to affect the development of anorexia nervosa.
Neurobiological factors
There are strong correlations between the neurotransmitter serotonin and various psychological symptoms such as mood, sleep, emesis (vomiting), sexuality and appetite. A recent review of the scientific literature has suggested that anorexia is linked to a disturbed serotonin system,[13] particularly to high levels at areas in the brain with the 5HT1A receptor - a system particularly linked to anxiety, mood and impulse control. Starvation has been hypothesised to be a response to these effects, as it is known to lower tryptophan and steroid hormone metabolism, which, in turn, might reduce serotonin levels at these critical sites and, hence, ward off anxiety. In contrast, studies of the 5HT2A serotonin receptor (linked to regulation of feeding, mood, and anxiety), suggest that serotonin activity is decreased at these sites. One difficulty with this work is that it is sometimes difficult to separate cause and effect, in that these disturbances to brain neurochemistry may be as much the result of starvation, than continuously existing traits that might predispose someone to develop anorexia. However, there is evidence that both personality characteristics (such as anxiety and perfectionism) and disturbances to the serotonin system are still apparent after patients have recovered from anorexia.[14] This suggests that these disturbances are likely to be causal risk factors.
Recent studies also suggest anorexia may be linked to an autoimmune response to melanocortin peptides which influence appetite and stress responses. [15] Brain-derived neurotrophic factor (BDNF) is also under investigation as a possible cause.[16]
Nutritional factors
Zinc deficiency may play a role in Anorexia. It is not thought responsible for causation of the initial illness but there is evidence that it may be an accelerating factor that deepens the pathology of the anorexia. A 1994 randomized, double-blind, placebo-controlled trial showed that zinc (14 mg per day) doubled the rate of body mass increase compared to patients receiving the placebo.[17]
Psychological factors
There has been a significant amount of study on psychological factors that suggests how biases in thinking and perception help maintain or contribute to the risk of developing anorexia.
Anorexic eating behavior is thought to originate from an obsessive fear of gaining weight due to a distorted self image[18] and is maintained by various cognitive biases that alter how the affected individual evaluates and thinks about their body, food and eating. This is not a perceptual problem, but one of how the perceptual information is evaluated by the affected person.[19] People with anorexia nervosa seem to more accurately judge their own body image while lacking a self-esteem boosting bias.[20]
It is often the case that people with anorexia nervosa also have other psychological difficulties and mental illness. Clinical depression, obsessive compulsive disorder, substance abuse and one or more personality disorders are the most likely conditions to be comorbid with anorexia, and high-levels of anxiety and depression are likely to be present regardless of whether they fulfill diagnostic criteria for a specific syndrome.[21]
Research into the neuropsychology of anorexia has indicated that many of the findings are inconsistent across studies and that it is hard to differentiate the effects of starvation on the brain from any long-standing characteristics. Nevertheless, one reasonably reliable finding is that those with anorexia have poor cognitive flexibility[22] (the ability to change past patterns of thinking, particularly linked to the function of the frontal lobes and executive system).
Other studies have suggested that there are some attention and memory biases that may maintain anorexia.[23] Attentional biases seem to focus particularly on body and body-shape related concepts, making them more salient for those affected by the condition, and some limited studies have found that those with anorexia may be more likely to recall related material than unrelated material.
Although there has been quite a lot of research into psychological factors, there are relatively few hypotheses which attempt to explain the condition as a whole.
Professor Chris Fairburn, of the University of Oxford and his colleagues have created a "transdiagnostic" model,[24] in which they aim to explain how anorexia, as well as related disorders such as bulimia nervosa and ED-NOS, are maintained. Their model is developed with psychological therapies, particularly cognitive behavioral therapy, in mind, and so suggests areas where clinicians could provide psychological treatment.
Their model is based on the idea that all major eating disorders (with the exception of obesity) share some core types of psychopathology which help maintain the eating disorder behavior. This includes clinical perfectionism, chronic low self-esteem, mood intolerance (inability to cope appropriately with certain emotional states) and interpersonal difficulties.
Social and environmental factors
Sociocultural studies have highlighted the role of cultural factors, such as the promotion of thinness as the ideal female form in Western industrialised nations, particularly through the media. A recent epidemiological study of 989,871 Swedish residents indicated that gender, ethnicity and socio-economic status were large influences on the chance of developing anorexia, with those with non-European parents among the least likely to be diagnosed with the condition, and those in wealthy, white families being most at risk.[25] A study by Garner and Garfinkel demonstrated that those in professions where there is a particular social pressure to be thin (such as models and dancers) were much more likely to develop anorexia during the course of their career,[26] and further research has suggested that those with anorexia have much higher contact with cultural sources that promote weight-loss.[27]
Although anorexia nervosa is usually associated with Western cultures, exposure to Western media is thought to have led to an increase in cases in non-Western countries. However, it is notable that other cultures may not display the same "fat phobic" worries about becoming fat as those with the condition in the West, and instead may present with low appetite with the other common features.[28]
There is a high rate of reported child sexual abuse experiences in clinical groups of who have been diagnosed with anorexia (up to 50% in those admitted to inpatient wards, with a lesser prevalence among people treated in the community). Although prior sexual abuse is not thought to be a specific risk factor for anorexia, those who have experienced such abuse are more likely to have more serious and chronic symptoms.[29]
The Internet has enabled anorexics and bulimics to contact and communicate with each other outside of a treatment environment, with much lower risks of rejection by mainstream society. A variety of websites exist, some run by people with anorexia, some by people in recovery, and some by professionals. The majority of such sites support a medical view of anorexia as a disorder to be cured, although some people affected by anorexia have formed online pro-ana communities that reject the medical view and argue that anorexia is a "lifestyle choice", using the internet for mutual support, and to swap weight-loss tips.[30] Such websites were the subject of significant media interest, largely focusing on concerns that these communities could encourage young women to develop or maintain eating disorders, and many were taken offline as a result.[31]
Relationship to autism
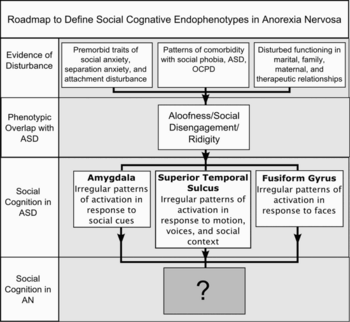
Since Gillberg's (1985) and others initial suggestion of relationship between anorexia nervosa and autism,[32][33][34] a large scale longitudinal study into teenage onset anorexia nervosa conducted in Sweden found that 23% of people with a long-standing eating disorder were on the autism spectrum.[35][36][37][38][39][40][41] Those on autism spectrum tend to have a worse outcome,[42] but may benefit from the combined use of behavioural and pharmacological therapies tailored to ameliorate autism rather than anorexia nervosa per se.[43][44] Other studies, most notably research conducted at the Maudsley Hospital UK, furthermore suggest that autistic traits are common in people with anorexia nervosa, shared traits include e.g. executive function, autism quotient score, central coherence, theory of mind, cognitive-behavioural flexibility, emotion regulation and understanding facial expressions.[45][46][47][48][49][50] Studies of identical twins indicate that genetics accounts for about three-quarters of the variance in anorexia nervosa;[10] the high degree of heritability, similar to that for autism, attests to a strong neurobiological component i.e. an atypical development of the brain.
Zucker et al. (2007) proposed that conditions on the autism spectrum make up the cognitive endophenotype underlying anorexia nervosa and appealed for increased interdisciplinary collaboration (see figure to right).[5] These research findings have been reported in the media and have included the claim that women not identified as being on the autism spectrum (e.g. those with undiagnosed Asperger syndrome), maybe identified via a co-morbid eating disorder.[51][52][53] A pilot study into the effectiveness Cognitive Behaviour Therapy, which based its treatment protocol on the hypothesised relationship between anorexia nervosa and an underlying autistic like condition, reduced perfectionism and rigidity in 17 out of 19 participants.[54]
Prognosis
Anorexia is thought to have the highest mortality rate of any psychiatric disorder, with anywhere from 6-20% of those who are diagnosed with the disorder eventually dying due to related causes.[55] The suicide rate of people with anorexia is also higher than that of the general population. [56]
Incidence, prevalence and demographics
The majority of research into the incidence and prevalence of anorexia has been done in Western industrialized countries, so results are generally not applicable outside these areas. However, recent reviews[57][58] of studies on the epidemiology of anorexia have suggested an incidence of between 8 and 13 cases per 100,000 persons per year and an average prevalence of 0.3% using strict criteria for diagnosis. These studies also confirm the view that the condition largely affects young adolescent females, with females between 15 and 19 years old making up 40% of all cases. Furthermore, the majority of cases are unlikely to be in contact with mental health services. As a whole, about 10% of people with anorexia are male and about 90% of people with anorexia are female.[2] Anorexia, however, is not exclusively limited to any age or demographic. In March 2008, a British senior university lecturer with PhD in psychology and a professional background in health, Rosemary Pope, died from anorexia.[59] Anorexia has been reported occurring throughout a patient's life extending into the seventies and eighties.[60] In addition, onset can occur in one's sixties or later.[61] The Italian character actor, Giovanni Rovini, died of onset of symptoms commencing in his early nineties. [62]
Treatment
The first line treatment for anorexia is usually focused on immediate weight gain, especially with those who have particularly serious conditions that require hospitalization. In particularly serious cases, this may be done as an involuntary hospital treatment under mental health law, where such legislation exists. In the majority of cases, however, people with anorexia are treated as outpatients, with input from physicians, psychiatrists, clinical psychologists and other mental health professionals.
The use of medication in anorexia is not all that well established. Many medications have been tried with mixed but mostly discouraging results. Drug treatments, such as SSRI or other antidepressant medication, have not been found to be generally effective for either treating anorexia,[63] or preventing relapse[64] although it has also been noted that there is a lack of adequate research in this area.
Family based treatment has also been found to be an effective treatment for adolescents with short term anorexia.[65] In particular, a method developed at the Maudsley Hospital is widely used and found to maintain improvement over time.[66] A 2008 paper published in the Journal of Clinical Child & Adolescent Psychology states that the evidence base is strongest for the Maudsley model for the treatment of anorexia nervosa.[67] At 4 to 5 year follow up one study shows full recovery rate of 60 - 90% with 10-15% remaining seriously ill. This compares favourable to other treatments such as inpatient care where full recovery rates vary between 33-55%.[68]
See also
- History of anorexia nervosa
- Adi Barkan (photographer who has campaigned against the use of anorexic models)
- Anorexia (symptom)
- Anorexia mirabilis
- Body dysmorphic disorder
- Body image
- Bulimia nervosa
- Binge eating disorder
- Cachexia
- Calorie restriction
- Defensive vomiting
- Eating disorder
- Eating disorder not otherwise specified
- Empress Elisabeth of Austria
- Fasting girls for a historical perspective on anorexia nervosa
- Female athlete triad
- Female body shape
- Hungry: A Mother and Daughter Fight Anorexia (book)
- Karen Carpenter
- Malnutrition
- Muscle dysmorphia (a reversed mental disorder of anorexia)
- National Association of Anorexia Nervosa and Associated Disorders
- Orthorexia nervosa
- Pro-ana
- Purging disorder
- Refeeding syndrome
- Wannarexia
References
- ^ "The Numbers Count: Mental Disorders in America". The National Institute of Mental Health. Retrieved 2008-10-09.
- ^ a b c Lask B, and Bryant-Waugh, R (eds) (2000) Anorexia Nervosa and Related Eating Disorders in Childhood and Adolescence. Hove: Psychology Press. ISBN 0-86377-804-6.
- ^ Costin, Carolyn.~ (1999) The Eating Disorder Sourcebook. Linconwood: Lowell House. 6.
- ^ a b Gowers S, Bryant-Waugh R. (2004) Management of child and adolescent eating disorders: the current evidence base and future directions. J Child Psychol Psychiatry, 45 (1), 63-83. PMID 14959803
- ^ a b c Zucker, N. L (2007). "Anorexia nervosa and autism spectrum disorders: Guided investigation of social cognitive endophenotypes" (PDF). Psychological Bulletin. 133 (6): 976–1006.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) Cite error: The named reference "Zucker1" was defined multiple times with different content (see the help page). - ^ Palazidou E, Robinson P, Lishman WA. (1990) Neuroradiological and neuropsychological assessment in anorexia nervosa. Psychol Med, 20 (3), 521-7. PMID 2236361.
- ^ Lask B, Gordon I, Christie D, Frampton I, Chowdhury U, Watkins B. (2005) Functional neuroimaging in early-onset anorexia nervosa. Int J Eat Disord, 37 Suppl, S49-51. PMID 15852320.
- ^ Jacobson, K. (2006) The Interpersonal Experience of Human Spatiality: A Phenomenological Interpretation of Anorexia Nervosa. Chiasmi International 8, 157-74
- ^ Tiggemann M and Pickering AS. (1996) Role of television in adolescent women's body dissatisfaction and drive for thinness Int J Eat Disord, Sep;20(2):199-203.
- ^ a b Klump, K. L. (2001). "Genetic and Environmental Influences on Anorexia Nervosa Syndromes in a Population–based Twin Sample". Psychological Medicine. 31 (04): 737–740. doi:10.1017/S0033291701003725. Retrieved 2009-09-29.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Urwin, R.E., Bennetts, B., Wilcken, B. et al. (2002). "Anorexia nervosa (restrictive subtype) is associated with a polymorphism in the novel norepinephrine transporter gene promoter polymorphic region," Molecular Psychiatry, 7(6), 652–657.
- ^ Siegfried Z, Berry EM, Hao S, Avraham Y. (2003) Animal models in the investigation of anorexia. Physiol Behav, 79 (1), 39-45. PMID 12818708.
- ^ Kaye WH, Frank GK, Bailer UF, Henry SE, Meltzer CC, Price JC, Mathis CA, Wagner A. (2005) Serotonin alterations in anorexia and bulimia nervosa: new insights from imaging studies. Physiol Behav, 85 (1), 73-81. PMID 15869768.
- ^ Kaye WH, Bailer UF, Frank GK, Wagner A, Henry SE. (2005) Brain imaging of serotonin after recovery from anorexia and bulimia nervosa. Physiol Behav, 86(1-2), 15-7. PMID 16102788.
- ^ Fetissov SO, Harro J, Jaanisk M, Jarv A, Podar I, Allik J, Nilsson I, Sakthivel P, Lefvert AK, Hokfelt T. (2005) Autoantibodies against neuropeptides are associated with psychological traits in eating disorders. Proc Natl Acad Sci U S A, 102 (41), 14865-70. PMID 16195379.
- ^ Attention: This template ({{cite doi}}) is deprecated. To cite the publication identified by doi:10.1093/hmg/ddh137, please use {{cite journal}} (if it was published in a bona fide academic journal, otherwise {{cite report}} with
|doi=10.1093/hmg/ddh137instead. - ^ Shay NF, Mangian HF (2000). "Neurobiology of zinc-influenced eating behavior". The Journal of nutrition. 130 (5S Suppl): 1493S–9S. PMID 10801965.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Rosen JC, Reiter J, Orosan P. (1995) Assessment of body image in eating disorders with the body dysmorphic disorder examination. Behav Res Ther, 1, 77-84. PMID 7872941.
- ^ Skrzypek S, Wehmeier PM, Remschmidt H. (2001) Body image assessment using body size estimation in recent studies on anorexia nervosa. A brief review. Eur Child Adolesc Psychiatry, 10 (4), 215-21. PMID 11794546.
- ^ Jansen A, Smeets T, Martijn C, Nederkoorn C. (2006) I see what you see: the lack of a self-serving body-image bias in eating disorders. Br J Clin Psychol, 45 (1), 123-35. PMID 16480571.
- ^ O'Brien KM, Vincent NK. (2003) Psychiatric comorbidity in anorexia and bulimia nervosa: nature, prevalence, and causal relationships. Clin Psychol Rev, 23 (1), 57-74. PMID 12559994
- ^ Tchanturia K, Campbell IC, Morris R, Treasure J. (2005) Neuropsychological studies in anorexia nervosa. Int J Eat Disord, 37 Suppl, S72-6. PMID 15852325.
- ^ Cooper MJ (2005) Cognitive theory in anorexia nervosa and bulimia nervosa: progress, development and future directions. Clin Psychol Rev, 25 (4), 511-31. PMID 15914267.
- ^ Fairburn CG, Cooper Z, Shafran R. (2003) Cognitive behavior therapy for eating disorders: a "transdiagnostic" theory and treatment. Behav Res Ther, 41 (5), 509-28. PMID 12711261.
- ^ Lindberg L, Hjern A. (2003) Risk factors for anorexia nervosa: a national cohort study. International Journal of Eating Disorders, 34 (4), 397-408. PMID 14566927
- ^ Garner DM, Garfinkel PE. (1980) Socio-cultural factors in the development of anorexia nervosa. Psychol Med, 10 (4), 647-56. PMID 7208724.
- ^ Toro J, Salamero M, Martinez E. (1994) Assessment of sociocultural influences on the aesthetic body shape model in anorexia nervosa. Acta Psychiatrica Scandinavica, 89 (3), 147-51. PMID 8178671.
- ^ Simpson KJ. (2002) Anorexia Nervosa and culture. J Psychiatr Ment Health Nurs, 9 (1), 65-71. PMID 11896858.
- ^ Carter JC, Bewell C, Blackmore E, Woodside DB. (2006) The impact of childhood sexual abuse in anorexia nervosa. Child Abuse Negl, 30 (3), 257-69. PMID 16524628.
- ^ Norris ML, Boydell KM, Pinhas L, Katzman DK. (2006) Ana and the internet: A review of pro-anorexia websites. International Journal of Eating Disorders, 39(6):443-7. PMID 16721839.
- ^ Reaves, J. (2001). Anorexia goes high tech. Time (July). Retrieved on April 16, 2007.
- ^ Gillberg, C. (1985). "Autism and anorexia nervosa: Related conditions". Nordisk Psykiatrisk Tidskrift. 39 (4): 307–312.
- ^ Rothery, D.J. (1988-01-11). "Anorexia nervosa and infantile autism" (5). Retrieved 2009-09-28.
{{cite journal}}: Cite journal requires|journal=(help); Unknown parameter|coauthor=ignored (|author=suggested) (help); Unknown parameter|vol=ignored (|volume=suggested) (help) - ^ Gillberg, C. (1992). "Do some cases of anorexia nervosa reflect underlying autistic-like conditions?". Behavioural neurology. 5 (1): 27–32.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Gillberg, I. Carina (1995-02). "Anorexia nervosa 6 years after onset: Part I. Personality disorders". Comprehensive Psychiatry. 36 (1): 61–69. doi:10.1016/0010-440X(95)90100-A. Retrieved 2009-09-23.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Gillberg, I. Carina (1996-02). "The cognitive profile of anorexia nervosa: A comparative study including a community-based sample". Comprehensive Psychiatry. 37 (1): 23–30. doi:10.1016/S0010-440X(96)90046-2. Retrieved 2009-09-23.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Råstam, M. (1996). "A six-year follow-up study of anorexia nervosa subjects with teenage onset". Journal of Youth and Adolescence. 25 (4): 439–453. doi:10.1007/BF01537541. Retrieved 2009-09-23.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Nilsson, E. W (1999-11). "Ten-year follow-up of adolescent-onset anorexia nervosa: personality disorders". Journal of the American Academy of Child and Adolescent Psychiatry. 38 (11): 1389–95. Retrieved 2009-09-23.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Wentz, Elisabet (2001). "Ten-Year Follow-up of Adolescent-Onset Anorexia Nervosa: Psychiatric Disorders and Overall Functioning Scales". The Journal of Child Psychology and Psychiatry and Allied Disciplines. 42 (05): 613–622. doi:10.1017/S0021963001007284. Retrieved 2009-09-23.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Råstam, Maria (2003-01-01). "Outcome of teenage-onset anorexia nervosa in a Swedish community-based sample". European Child & Adolescent Psychiatry. 12 (1). doi:10.1007/s00787-003-1111-y. Retrieved 2009-09-23.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Wentz, Elisabet (2005-12-01). "Childhood onset neuropsychiatric disorders in adult eating disorder patients". European Child & Adolescent Psychiatry. 14 (8): 431–437. doi:10.1007/s00787-005-0494-3. Retrieved 2009-09-23.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Wentz, Elisabet (2009-02-01). "Adolescent-onset anorexia nervosa: 18-year outcome". The British Journal of Psychiatry. 194 (2): 168–174. doi:10.1192/bjp.bp.107.048686. Retrieved 2009-09-25.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Fisman, S (1996-07). "Case study: anorexia nervosa and autistic disorder in an adolescent girl". Journal of the American Academy of Child and Adolescent Psychiatry. 35 (7): 937–940. ISSN 0890-8567. Retrieved 2009-09-26.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Kerbeshian, Jacob (2008). "Is anorexia nervosa a neuropsychiatric developmental disorder? An illustrative case report". World Journal of Biological Psychiatry. doi:10.1080/15622970802043117. ISSN 1562-2975. Retrieved 2009-09-27.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Gillberg, I. C (2007). "Cognitive and executive functions in anorexia nervosa ten years after onset of eating disorder". Journal of Clinical and Experimental Neuropsychology. 29 (2): 170–178.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Hambrook, D. (2008). "Empathy, systemizing, and autistic traits in anorexia nervosa: a pilot study". The British journal of clinical psychology/the British Psychological Society. 47 (Pt 3): 335. doi:http://dx.doi.org/10.1348/014466507X272475.
{{cite journal}}: Check|doi=value (help); External link in|doi=|coauthors=ignored (|author=suggested) (help) - ^ Lopez, C. (2008). "An examination of the concept of central coherence in women with anorexia nervosa". International Journal of Eating Disorders. 41 (2): 143–152. doi:10.1002/eat.20478.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Russell, Tamara Anne (2009). "Aspects of social cognition in anorexia nervosa: Affective and cognitive theory of mind". Psychiatry Research. 168 (3): 181–185. doi:10.1016/j.psychres.2008.10.028. ISSN 0165-1781. Retrieved 2009-09-26.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Zastrow, Arne (2009-05-01). "Neural Correlates of Impaired Cognitive-Behavioral Flexibility in Anorexia Nervosa". Am J Psychiatry. 166 (5): 608–616. doi:10.1176/appi.ajp.2008.08050775. Retrieved 2009-09-28.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Harrison, Amy (2009). "Emotion recognition and regulation in anorexia nervosa". Clinical Psychology & Psychotherapy. 16 (4): 348–356. doi:10.1002/cpp.628. Retrieved 2009-09-27.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Campbell, Katy (2007-08-17). "Is anorexia the female Asperger's?". The Times (London). ISSN 0951-9467. Retrieved 2009-09-28.
- ^ Szalavitz, Maia (2009-06-19). "A Genetic Link Between Anorexia and Autism?". Time. ISSN 0040-718X. Retrieved 2009-09-23.
{{cite news}}: Check|issn=value (help) - ^ "Girls' autism 'under-diagnosed'". BBC. 2005-06-28. Retrieved 2009-09-25.
- ^ Whitney, Jenna (2008). "Service users' feedback on cognitive training in the treatment of anorexia nervosa: A qualitative study". International Journal of Eating Disorders. 41 (6): 542–550. doi:10.1002/eat.20536. Retrieved 2009-09-29.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Herzog, David B; Greenwood, Dara N; Dorer, David J; Flores, Andrea T; Ekeblad, Elizabeth R; Richards, Ana; Blais, Mark A; Keller, Martin B (2000), "Mortality in eating disorders: A descriptive study", International Journal of Eating Disorders, 28 (1): 20–26, doi:10.1002/(SICI)1098-108X(200007)28:1<20::AID-EAT3>3.0.CO;2-X
- ^ Pompili, M; Mancinelli, I; Girardi, P; Ruberto, A; Tatarelli, R (2004), "Suicide in anorexia nervosa: A meta-analysis", International Journal of Eating Disorders, 36 (1), John Wiley: 99–103, doi:10.1002/eat.20011
- ^ Bulik CM, Reba L, Siega-Riz AM, Reichborn-Kjennerud T. (2005) Anorexia nervosa: definition, epidemiology, and cycle of risk. Int J Eat Disord, 37 Suppl, S2-9. PMID 15852310.
- ^ Hoek HW. (2006) Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Curr Opin Psychiatry., 19 (4), 389-94. PMID 16721169.
- ^ "Professor, 49, died from anorexia". BBC. 2008-04-22. Retrieved 2008-04-23.
- ^ AJ Giannini, N Telew. Anorexia nervosa in geriatric patienys. Geriatric Medicine Today. 6:75-78, 1987.
- ^ AJ Giannini. Drug abuse and depression:possible models for geriatric anorexia. Neurobiology of Aging. 9:26-27, 1988.
- ^ AJ Giannini, AE Slaby. The Eating Disorders. NY, Springer-Verlag,1993. ISBN 3-540-94002-2
- ^ Claudino AM, Hay P, Lima MS, Bacaltchuk J, Schmidt U, Treasure J. (2006) Antidepressants for anorexia nervosa. Cochrane Database Syst Rev, 1, CD004365. PMID 16437485.
- ^ Walsh BT, Kaplan AS, Attia E, Olmsted M, Parides M, Carter JC, Pike KM, Devlin MJ, Woodside B, Roberto CA, Rockert W. (2006) Fluoxetine after weight restoration in anorexia nervosa: a randomized controlled trial. JAMA, 295(22), 2605-12. PMID 16772623.
- ^ Lock J, Le Grange D. (2005) Family-based treatment of eating disorders. Int J Eat Disord, 37 Suppl, S64-7. PMID 15852323.
- ^ Le Grange D. (2005) The Maudsley family-based treatment for adolescent anorexia nervosa. World Psychiatry, 4 (3), 142-6. PMID 16633532.
- ^ Keel, Pamela K. and Haedt, Alissa. Journal of Clinical Child & Adolescent Psychology, Volume 37, Issue 1 January 2008 , pages 39 - 61
- ^ Le Grange, Daniel and Eisler, Ivan. Family Interventions in Adolescent Anorexia Nervosa. "Child Adolesc Psychiatric Clin N Am". 18 (2008): 159-173
External links
Informational resources
- MayoClinic eating disorders information
- BBC Mental Health on eating disorders
- Anorexia nervosa NHS Direct
Media stories and reports
- Anorexia goes high-tech - Time magazine on pro-ana websites.
- Fighting Anorexia: No One to Blame - Newsweek on the increasing prevalence of anorexia in young people.
- More 4 News report on how eating disorders are increasingly affecting men as well as women.
- Resources on Anorexia Nervosa and other Eating Disorders including an hour long program on the subject.
