Asperger syndrome and neuroscience
This article has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these template messages)
|
Asperger syndrome (AS) is a neurodevelopmental condition. Asperger syndrome, along with other autism spectrum disorders (ASD), is an active field of research. From a biological perspective, it is unclear whether "autism and Asperger's disorder (AD) exist on a symptom continuum or are separate disorders with discrete neurobiological underpinnings."[1]
Early research
Behavioral and cognitive descriptions
- Cognition
- Early onset language, high language skills
- Normal or above average VIQ, PIQ < VIQ
- Intense narrow interest
- "little professors"
Hans Asperger coined the phrase "little professors" because of their ability to talk about their favorite subject in great detail. Asperger noticed that many of the children he identified as being autistic used their special talents in adulthood and had successful careers. One of them became a professor of astronomy and solved an error in Newton’s work he had originally noticed as a student.[2] Another one of Asperger's patients was the Austrian writer and Nobel Prize in Literature laureate, Elfriede Jelinek.[3]
- Learning, memory, and savantism
- Social
- Social criteria
- Eye contact / gaze avoidance
- Face processing
- Subjects with AS take longer to respond to face processing in a stroop test.
- "The prevalence for face recognition difficulties was 46.6% in AS group (compared with 10.7% in the control group)".[4]
- Repetition
- Repetitive behavior
- Resistance to change
- Other
- Motor coordination and motor planning
Clinical descriptions
Hans Asperger
Asperger was the director of the University Children's Clinic in Vienna. In 1944, Asperger described in the paper "'Autistic psychopathy' in childhood"[5] four children in his practice[6] who had difficulty in integrating themselves socially. Although their intelligence appeared normal, the children lacked nonverbal communication skills, failed to demonstrate empathy with their peers, and were physically clumsy. Their speaking was either disjointed or overly formal, and their all-absorbing interest in a single topic dominated their conversations. Asperger called the condition "autistic psychopathy" and described it as primarily marked by social isolation.[7] Asperger called his young patients "little professors".[5][6]
Popularization
Lorna Wing is the author of many books and academic papers, including Asperger's Syndrome: a Clinical Account, a 1981 academic paper that popularised the research of Hans Asperger and introduced the term "Asperger's syndrome".
The diagnosis of AS is complicated by the use of several different screening instruments.[8][9] In addition to the DSM-IV and the ICD-10 criteria, other sets of diagnostic criteria for AS are the Szatmari et al. criteria[10] and the Gillberg and Gillberg criteria.[11]
Gillberg
Gillberg's criteria
- Severe impairment in reciprocal social interaction (at least two of the following)
- inability to interact with peers
- lack of desire to interact with peers
- lack of appreciation of social cues
- socially and emotionally inappropriate behavior
- All-absorbing narrow interest (at least one of the following)
- exclusion of other activities
- repetitive adherence
- more rote than meaning
- Imposition of routines and interests (at least one of the following)
- on self, in aspects of life
- on others
- Speech and language problems (at least three of the following)
- delayed development
- superficially perfect expressive language
- formal, pedantic language
- odd prosody, peculiar voice characteristics
- impairment of comprehension including misinterpretations of literal/implied meanings
- Non-verbal communication problems (at least one of the following)
- limited use of gestures
- clumsy/gauche body language
- limited facial expression
- inappropriate expression
- peculiar, stiff gaze
- Motor clumsiness: poor performance on neurodevelopmental examination
Szatmari
Szatmari Critera
- Social isolation (at least two of the following):
- no close friends
- avoids others
- no interest in making friends
- a loner
- Impaired social interaction (at least one of the following):
- approaches others only to have own needs met
- clumsy social approach
- one-sided responses to peers
- difficulty sensing feelings of others
- indifference to the feelings of others
- Impaired non-verbal communication (at least one of the following):
- limited facial expressions
- impossible to read emotions through facial expression of the child
- inability to convey message with eyes
- avoids looking at others
- does not use hands to aid expression
- large and clumsy gestures
- infringes on other people’s physical space
- Speech and language peculiarities (at least two of the following):
- abnormalities of inflection
- over-talkative
- non-communicative
- lack of cohesion to conversation
- idiosyncratic use of words ( uses words in a different way than what they would normally mean)
- repetitive patters of speech
DSM-IV-TR
DSM-IV-TR Criteria (2000)
- Qualitative impairment in social interaction, as manifested by at least two of the following:
- marked impairment in the use of multiple nonverbal behaviors such as eye-to-eye gaze, facial expression, body postures, and gestures to regulate social interaction
- failure to develop peer relationships appropriate to developmental level
- a lack of spontaneous seeking to share enjoyment, interests, or achievements with other people (e.g., by a lack of showing, bringing, or pointing out objects of interest to other people)
- lack of social or emotional reciprocity
- Restricted repetitive and stereotyped patterns of behavior, interests, and activities, as manifested by at least one of the following:
- encompassing preoccupation with one or more stereotyped and restricted patterns of interest that is abnormal either in intensity or focus
- apparently inflexible adherence to specific, nonfunctional routines or rituals
- stereotyped and repetitive motor mannerisms (e.g., hand or finger flapping or twisting, or complex whole-body movements)
- persistent preoccupation with parts of objects
- The disturbance causes clinically significant impairment in social, occupational, or other important areas of functioning.
- There is no clinically significant general delay in language (e.g., single words used by age 2 years, communicative phrases used by age 3 years).
- There is no clinically significant delay in cognitive development or in the development of age-appropriate self-help skills, adaptive behavior (other than in social interaction), and curiosity about the environment in childhood.
- Criteria are not met for another specific Pervasive Developmental Disorder or Schizophrenia.
ICD-10
ICD-10
- A lack of any clinically significant general delay in spoken or receptive language or cognitive development. Diagnosis requires that single words should have developed by two years of age or earlier and that communicative phrases be used by three years of age or earlier. Self-help skills, adaptive behaviour and curiosity about the environment during the first three years should be at a level consistent with intellectual development. However, motor milestones may be somewhat delayed and motor clumsiness is usual (although not a necessary diagnostic feature). Isolated special skills, often related to abnormal preoccupations, are common, but are not required for diagnosis.
- Qualitative abnormalities in reciprocal social interaction (criteria as for autism).
- An unusually intense circumscribed interest or restrictive, repetitive, and stereotyped patterns of behaviour, interests and activities (criteria as for autism; however, it would be less usual for these to include either motor mannerisms or preoccupations with part-objects or non-functional elements of play materials).
- The disorder is not attributable to other varieties of pervasive developmental disorder; schizotypal disorder (F21); simple schizophrenia (F20.6); reactive and disinhibited attachment disorder of childhood (F94.1 and .2); obsessional personality disorder (F60.5); obsessive-compulsive disorder (F42).
Neuroanatomical
Neuroimaging

MRI Comparison of Asperger and High Functioning Autism revealed the HFA group had the atypical pattern of decreasing Performance IQ linked to increasing gray matter. In contrast, subjects with Asperger showed the typical pattern of increasing PIQ associated with increasing gray matter volume. The study also observed a correlation between PIQ and cerebral white tissue volume in the Aspergers that was significantly different from the HFA and control groups.[12]
A 2011 meta-analysis[13] compared the grey matter volume of AS subjects to HFA subjects. Autism showed lower volumes in the cerebellum, right uncus, dorsal hippocampus and middle temporal gyrus compared with controls; grey matter volumes were greater in the bilateral caudate, prefrontal lobe and ventral temporal lobe.
Asperger syndrome showed "lower grey matter volumes in the bilateral amygdala/hippocampal gyrus and prefrontal lobe, left occipital gyrus, right cerebellum, putamen and precuneus compared with controls; grey matter volumes were greater in more limited regions, including the bilateral inferior parietal lobule and the left fusiform gyrus." Aspergers and autism both showed increases in the ventral temporal lobe of the left hemisphere.
Austism Spectrum Disorders "showed robust reductions of gray matter volume in the amygdala-hippocampus complex (particularly on the right side) and medial parietal regions (precuneus, BA7). A small increase in gray matter volume was found in the left middle and inferior frontal gyri (BA46 and BA10)."[14]
Amygdala
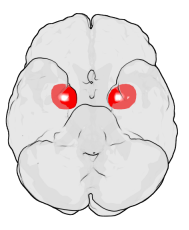
The amygdala perform a primary role in the processing of memory and emotional reactions, the amygdalae are considered part of the limbic system.[15] The amygdala is associated with fear processing and social interaction.
A MRI study found subjects with Asperger syndrome had significant differences in both the size and the aging of the amygdala.[16]
A study found abnormal fear acquisition in subjects with Asperger syndrome.[17]
Other
Neurological systems
- Facial image processing[4]
Sleep
- Multiple studies have confirmed a high prevalence of sleep disorders in subjects with Asperger syndrome.[4] Insomnia is a frequent finding in that population. The studies[18] have shown subjects with Asperger syndrome exhibit an increased prevalence of disorders in initiating and maintaining sleep (both in children and adults).[19][20][21]
- Subjects with autism have significantly lower levels of melatonin and ASMT.[22]
Stress response
- Heart-rate and EEG measures show children with Asperger Syndrome react more strongly to stressful stimuli.[23]
Gaze and eye movements
- Inhibition of return is an effect where reaction time is increased in previously-attended locations. Subjects with Asperger's showed normal IOR response to some stimuli, but abnormal responses when shown "eye gaze" stimuli.[24]
EEG
- A study reported subjects with Aspergers showed more theta rhythms, "and they were not localized in the AS group". The authors reported "The buildup of slow waves in response to hyperventilation tended to appear earlier in the AS group and a big buildup appeared in only the AS group." According to the authors, the "findings regarding slow wave buildup suggested hypersensitivity to hypocapnea induced by hyperventilation".[25]
Biochemical systems
- Sex hormone systems
- Neuronal growth systems
- Neurotrophins like BDNF are elevated in blood of children with autism and "may be associated with early brain overgrowth".[26]
- Social-emotional systems
- ACTH
- Subjects with AS had significantly higher plasma-ACTH values[27]
- Cortisol
- Absence of cortisol awakening response in subjects with Asperger syndrome (HPA dysregulation).[28]
- Genes involved in cortisol synthesis implicated in Asperger syndrome. "CYP1A1, CYP1B1, CYP3A, CYP7A1, CYP11A, CYP11B1, CYP17A1, CYP19A1, CYP21A2, POR; Synthesis of sex hormones such as progesterone, estrogen, cortisol, aldosterone and testosterone."[29]
- Inflammation
- Atopy increased in subjects with AS.[30]
Biomarkers implicated in Asperger syndrome
- Cytokines are small proteins that can influence the behavior of white blood cells.
- Interleukins are a group of cytokines secreted by white blood cells (leukocytes).[31]
- Tissue factor (TF) is related to a protein family known as the cytokine receptor class II family. The members of this receptor family are activated by cytokines.
- Tenascin-C is the founding member of the Tenascin gene family. In the embryo it is made by migrating cells like the neural crest; it is also abundant in developing tendons, bone and cartilage.
Genes implicated in Asperger syndrome
Single nucleotide polymorphism (SNP) analysis, genetic screens, and other methods have implicated several specific genes:
Neural development
- HOXA1 (Homeobox protein Hox-A1) is a Hox gene, involved in neural development. A common polymorphism in the HOXA1 gene is associated with a susceptibility to autism spectrum disorder.[32]
- NTRK1 (Neurotrophic tyrosine kinase receptor type 1) encodes a receptor that binds to neurotrophins. The presence of this kinase leads to cell differentiation and may play a role in specifying sensory neuron subtypes. Mutations in the NTRK1 gene have been associated with congenital insensitivity to pain with anhidrosis and self-mutilating behavior. Mice without NTKR1 showed "severe sensory and sympathetic neuropathy, especially for nociceptive neurons".[33]
- NLGN3 and NLGN4X.[34] Neuroligins are believed to be involved in synapse formation.
- NRXN1, CNTNAP2, and SHANK3. SHANK3 "regulates the structural organization of dendritic spines". SHANK3 binds with neuroligins. Mutations SHANK3 are associated are associated with ASD.[35]
- BDNF (Brain-derived neurotrophic factor) is associated with neuroplasticity. Various studies have shown possible links between BDNF and conditions such as depression,[36][37] schizophrenia,[38] obsessive-compulsive disorder,[39] Alzheimer's disease,[40] Huntington's disease,[41] Rett syndrome,[42] and dementia,[43] as well as anorexia nervosa[44] and bulimia nervosa.[45] BDNF has been associated with Asperger syndrome and autism.[46][47]
Sex steroids
- ESR1 and ESR2 (Estrogen Receptors α and β) encode estrogen receptor proteins.
- CYP11B1 encodes Steroid 11-beta-hydroxylase, which is involved in the biosynthesis of both cortisol and corticosterone. (see also Congenital adrenal hyperplasia due to 11β-hydroxylase deficiency )
Emotional/Social
- MAOB (Monoamine Oxidase B) associated with mood and anxiety.
- AVPR1B encodes a vasopressin receptor located in the anterior pituitary, where it stimulates ACTH release.[48] Subsequent studies have shown that it is also present in the brain.[49][50]
- GABRB3 encodes a GABA receptor subunit. Deletion has been associated with Angelman Syndrome (hyper-socialization). A specific polymorphism in the gene is reported to distinguish Asperger Syndrome from High Functioning Autism.[34]GABA is the primary inhibitory neurotransmitter of the human brain. Ma et al. (2005) concluded that GABRA4 is involved in the etiology of autism, and that it potentially increases autism risk through interaction with GABRB1.[51] The GABRB3 gene has been associated with savant skills.[52] The GABRB3 gene deficient mouse has been proposed as a model of ASD.[53]
- WFS1 encodes the protein wolframin. Mutations in WFS1 are associated with the neurodegenerative Wolfram syndrome. WFS1 polymorphisms have been associated with affective disorders. WFS1 has been implicated in anxiety.[54]
- OXT encodes Oxytocin. OXTR encodes an Oxytocin receptor. Oxytocin infusion reduced repetitive behaviors in subjects with Asperger syndrome.[55][56] Oxytocin nasal spray trial[57]
- PRL (Prolactin), PRLR (Prolactin receptor) implicated in ASD.[58]
- DISC1 (Disrupted in schizophrenia 1) is a gene that has been linked to various psychiatric conditions, including clinical depression, bipolar disorder, Autism and Asperger Syndrome.[59]
Asperger syndrome versus High Functioning Autism
The precise relationship between Asperger syndrome and autism is unclear.[13]
- Subjects with HFA displayed deficits in attentional set-shifting, i.e. the ability to display flexibility in the face of changing schedules of reinforcement. Subjects with AS did not display the set-shifting deficits.[60]<
- Relatives of subjects with AS were significantly more likely to have depression, schizophrenia, or the broader autistic phenotype (compared to relatives of subjects with HFA).[61]
- Examination of mothers of children with Asperger or autism, mothers with a history of mood disorders are more likely to have a child with Asperger syndrome phenotype than the Autism phenotype.[62]
- A meta-analysis found that autism is characterized by increased gray matter volume in both hemispheres of the brain, but in contrast, Asperger syndrome showed decreased gray matter volume in the right hemisphere and increased in the left hemisphere.[13]
- On an inspection time test, mean inspection time was shorter for the autistic subgroup (but not the Asperger subgroup).[63]
- A study was able to discriminate between individuals with Asperger’s syndrome and those with autism by their ability to solve Theory of mind tasks.[64]
- Subjects with AS showed the typical pattern of increased gray matter being associated with increased Performance IQ. In contrast, subjects with HFA have the opposite pattern—increased gray matter being associated with decreased PIQ.[12]
Theoretical frameworks
Asperger syndrome as an autistic spectrum disorder
Increasing consensus has classed Asperger syndrome as a subtype of autism spectrum disorders. In this framework, Asperger syndrome is distinguished from "classic" high functioning autism primarily by a lack of language or cognitive deficits.
Intense World Theory
The Intense World Theory seeks to explain autism's "core cognitive consequences of hyper-perception, hyper-attention, hyper-memory and hyper-emotionality."[65] According to the Intense World Theory, individuals with autism-spectrum disorders are "hypersensitive" to the world around them.[65] According to the theory, the pathology in autism may be hyper-functioning of local neural microcircuits. It's argued that local neural microcircuits in individuals with autism possess both "hyper-reactivity" and "hyper-plasticity".[65]
- NTRK1, KO mice
- Sensory processing disorder
Epigenetic models
This section needs expansion. You can help by adding to it. (October 2012) |
Deficit in empathy / theory of mind
- "Children with AS did not refer to cognitive states as often as the other groups" in narrative testing.[66]
"Extreme Male Brain"
Researcher Simon Baron-Cohen has proposed that the Aspergers/Autism represents an "extreme male brain". The hypothesis is supported by the increased prevalence of the conditions in males relative to females. Additional evidence comes from studies of gender dysphoria—a study found female-to-male (FTM) transgender people have higher rates of autistic traits copared to male-to-female (MTF) transgender people or non-transsexuals.[67]
Sex differences
This section is empty. You can help by adding to it. (February 2013) |
Sex-specific serum biomarker patterns in adults with Asperger’s syndrome
E Schwarz1, PC Guest1, H Rahmoune1, L Wang1, Y Levin1, E Ingudomnukul2, L Ruta2,3, L Kent 2,4, M Spain5, S Baron-Cohen2 and S Bahn1,6 1Institute of Biotechnology, University of Cambridge, Cambridge, UK; 2Department of Psychiatry, Autism Research Centre, University of Cambridge, Cambridge, UK; 3Division of Child Neurology and Psychiatry, Department of Pediatrics, University of Catania, Catania, Italy; Bute Medical School, University of St Andrews, Scotland, UK; Rule Based Medicine, Austin, TX, USA and Department of Neuroscience, Erasmus MC, Rotterdam, The Netherlands
Autism spectrum conditions have been hypothesized to be an exaggeration of normal male low-empathizing and high-systemizing behaviors. We tested this hypothesis at the molecular level by performing comprehensive multi-analyte profiling of blood serum from adult subjects with Asperger’s syndrome (AS) compared with controls. This led to identification of distinct sex-specific biomarker fingerprints for male and female subjects. Males with AS showed altered levels of 24 biomarkers including increased levels of cytokines and other inflammatory molecules. Multivariate statistical classification of males using this panel of 24 biomarkers revealed a marked separation between AS and controls with a sensitivity of 0.86 and specificity of 0.88.
Testing this same panel in females did not result in a separation between the AS and control groups. In contrast, AS females showed altered levels of 17 biomarkers including growth factors and hormones such as androgens, growth hormone and insulin-related molecules. Classification of females using this biomarker panel resulted in a separation between AS and controls with sensitivities and specificities of 0.96 and 0.83, respectively, and testing this same panel in the male group did not result in a separation between the AS and control groups. The finding of elevated testosterone in AS females confirmed predictions from the ‘extreme male brain’ and androgen theories of autism spectrum conditions. We conclude that to understand the etiology and development of autism spectrum conditions, stratification by sex is essential. Molecular Psychiatry advance online publication, 28 September 2010; doi:10.1038/mp.2010.102
Rejected frameworks
Refrigerator mother refers to a rejected hypothesis that autism was caused by maternal emotional frigidity. A modern understanding of genetics has led to a rejection of this theory of causation. Similarly, a hypothetical causal connection between MMR vaccine and autism has been rejected.
References
- ^ Stanley-Cary, C; Rinehart, N; Tonge, B; White, O; Fielding, J (2011). "Greater disruption to control of voluntary saccades in autistic disorder than Asperger's disorder: Evidence for greater cerebellar involvement in autism?". Cerebellum (London, England). 10 (1): 70–80. doi:10.1007/s12311-010-0229-y. PMID 21072692.
- ^ Asperger H (1944). "Die "Autistischen Psychopathen" im Kindesalter". Archiv für Psychiatrie und Nervenkrankheiten. 117: 132–135. doi:10.1007/bf01837709.
- ^ Mayer, Verena; Koberg, Roland (2006). Elfriede Jelinek. Rowohlt Verlag GmbH. p. 32. ISBN 3-498-03529-0. OCLC 63127455.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ a b c Nieminen-von Wendt T, Paavonen JE, Ylisaukko-Oja T; et al. (2005). "Subjective face recognition difficulties, aberrant sensibility, sleeping disturbances and aberrant eating habits in families with Asperger syndrome". BMC Psychiatry. 5: 20. doi:10.1186/1471-244X-5-20. PMC 1097741. PMID 15826308.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ a b Frith, Uta (1991). 'Autistic psychopathy' in childhood. Cambridge, UK: Cambridge University Press. ISBN 0-521-38608-X. OCLC 23731537.
{{cite book}}:|work=ignored (help) - ^ a b Baskin JH, Sperber M, Price BH (2006). "Asperger syndrome revisited". Rev Neurol Dis. 3 (1): 1–7. PMID 16596080.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ National Institute of Neurological Disorders and Stroke (NINDS) (July 31, 2007). Asperger Syndrome Fact Sheet. Retrieved 24 August 2007.
- ^ "Asperger Syndrome Fact Sheet". http://www.ninds.nih.gov.
{{cite web}}: External link in|work= - ^ Ehlers S, Gillberg C (November 1993). "The epidemiology of Asperger syndrome. A total population study". J Child Psychol Psychiatry. 34 (8): 1327–50. doi:10.1111/j.1469-7610.1993.tb02094.x. PMID 8294522.
- ^ Szatmari P, Bremner R, Nagy J (1989). "Asperger's syndrome: a review of clinical features". Canadian Journal of Psychiatry. 34 (6): 554–60. PMID 2766209.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Gillberg IC, Gillberg C (Jul 1989). "Asperger syndrome-some epidemiological considerations: A research note". J Child Psychol Psychiatry. 30 (4): 631–38. doi:10.1111/j.1469-7610.1989.tb00275.x. PMID 2670981.
- ^ a b Lotspeich LJ, Kwon H, Schumann CM; et al. (March 2004). "Investigation of neuroanatomical differences between autism and Asperger syndrome" (PDF). Arch. Gen. Psychiatry. 61 (3): 291–8. doi:10.1001/archpsyc.61.3.291. PMID 14993117.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ a b c Yu KK, Cheung C, Chua SE, McAlonan GM (November 2011). "Can Asperger syndrome be distinguished from autism? An anatomic likelihood meta-analysis of MRI studies". J Psychiatry Neurosci. 36 (6): 412–21. doi:10.1503/jpn.100138. PMC 3201995. PMID 21406158.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Via E, Radua J, Cardoner N, Happé F, Mataix-Cols D (April 2011). "Meta-analysis of gray matter abnormalities in autism spectrum disorder: should Asperger disorder be subsumed under a broader umbrella of autistic spectrum disorder?". Arch. Gen. Psychiatry. 68 (4): 409–18. doi:10.1001/archgenpsychiatry.2011.27. PMID 21464365.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Amunts, K.; Kedo, O.; Kindler, M.; Pieperhoff, P.; Mohlberg, H.; Shah, N.J.; Habel, U.; et al. (2005). "Cytoarchitectonic mapping of the human amygdala, hippocampal region and entorhinal cortex: Intersubject variability and probability maps". Anatomy and Embryology. 210 (5–6): 343–52. doi:10.1007/s00429-005-0025-5. PMID 16208455.
{{cite journal}}: Explicit use of et al. in:|last8=(help) - ^ Murphy CM, Deeley Q, Daly EM; et al. (February 2012). "Anatomy and aging of the amygdala and hippocampus in autism spectrum disorder: an in vivo magnetic resonance imaging study of Asperger syndrome". Autism Res. 5 (1): 3–12. doi:10.1002/aur.227. PMID 21948742.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Gaigg, SB; Bowler, DM (2007). "Differential fear conditioning in Asperger's syndrome: Implications for an amygdala theory of autism". Neuropsychologia. 45 (9): 2125–34. doi:10.1016/j.neuropsychologia.2007.01.012. PMID 17321555.
- ^ Paavonen et al. and Tani et al.
- ^ "It is not known why persons with AS have insomnia or sleeping problems, but the reports by Godbout et al. [32,33] suggest that AS subjects may present the same difficulties in initiating and maintaining sleep as those previously described in autism. It has also been hypothesized that individuals with AS have a defective sleep control system which may be associated with the clinical picture of AS [33]. From a clinical point of view, sleep disturbances are typical among people with AS and should be taken into account when a person is referred for a diagnosis, especially as the problem can be alleviated by melatonin [17]".
- ^ Godbout, Roger; Bergeron, Cybèle; Limoges, Élyse; Stip, Emmanuel; Mottron, Laurent (2000). "A laboratory study of sleep in Aspergerʼs syndrome". NeuroReport. 11 (1): 127–30. doi:10.1097/00001756-200001170-00025. PMID 10683843.
- ^ Limoges, E. (2005). "Atypical sleep architecture and the autism phenotype". Brain. 128 (5): 1049. doi:10.1093/brain/awh425.
- ^ Melke J, Goubran Botros H, Chaste P; et al. (January 2008). "Abnormal melatonin synthesis in autism spectrum disorders". Mol. Psychiatry. 13 (1): 90–8. doi:10.1038/sj.mp.4002016. PMC 2199264. PMID 17505466.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Tiinanen, S; Määttä, A; Silfverhuth, M; Suominen, K; Jansson-Verkasalo, E; Seppänen, T (2011). "HRV and EEG based indicators of stress in children with Asperger syndrome in audio-visual stimulus test". Conference proceedings : ... Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference. 2011: 2021–4. doi:10.1109/IEMBS.2011.6090371. ISBN 978-1-4577-1589-1. PMID 22254732.
- ^ Marotta A, Pasini A, Ruggiero S; et al. (April 2013). "Inhibition of return in response to eye gaze and peripheral cues in young people with Asperger's syndrome". J Autism Dev Disord. 43 (4): 917–23. doi:10.1007/s10803-012-1636-3. PMID 22932768.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ NAKATANI HIDEO. "Conventional EEG findings of patients with Asperger's disorder". Science Links Japan. Retrieved 7 September 2013.
- ^ Schwarz E, Guest PC, Rahmoune H; et al. (December 2011). "Sex-specific serum biomarker patterns in adults with Asperger's syndrome". Mol. Psychiatry. 16 (12): 1213–20. doi:10.1038/mp.2010.102. PMID 20877284.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Tani P, Lindberg N, Matto V; et al. (June 2005). "Higher plasma ACTH levels in adults with Asperger syndrome". J Psychosom Res. 58 (6): 533–6. doi:10.1016/j.jpsychores.2004.12.004. PMID 16125520.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Brosnan, M; Turner-Cobb, J; Munro-Naan, Z; Jessop, D (2009). "Absence of a normal cortisol awakening response (CAR) in adolescent males with Asperger syndrome (AS)". Psychoneuroendocrinology. 34 (7): 1095–100. doi:10.1016/j.psyneuen.2009.02.011. PMID 19304400.
- ^ Chakrabarti B, Dudbridge F, Kent L; et al. (June 2009). "Genes related to sex steroids, neural growth, and social-emotional behavior are associated with autistic traits, empathy, and Asperger syndrome". Autism Res. 2 (3): 157–77. doi:10.1002/aur.80. PMID 19598235.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Magalhães ES, Pinto-Mariz F, Bastos-Pinto S, Pontes AT, Prado EA, deAzevedo LC (November 2009). "Immune allergic response in Asperger syndrome". J. Neuroimmunol. 216 (1–2): 108–12. doi:10.1016/j.jneuroim.2009.09.015. PMID 19840888.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Brocker, C; Thompson, D; Matsumoto, A; Nebert, DW; Vasiliou, V (Oct 2010). "Evolutionary divergence and functions of the human interleukin (IL) gene family". Human Genomics. 5 (1): 30–55. doi:10.1186/1479-7364-5-1-30. PMC 3390169. PMID 21106488.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Ingram, Jennifer L.; Stodgell, Christopher J.; Hyman, Susan L.; Figlewicz, Denise A.; Weitkamp, Lowell R.; Rodier, Patricia M. (2000). "Discovery of allelic variants ofHOXA1 andHOXB1: Genetic susceptibility to autism spectrum disorders". Teratology. 62 (6): 393–405. doi:10.1002/1096-9926(200012)62:6<393::AID-TERA6>3.0.CO;2-V. PMID 11091361.
- ^ Chakrabarti, B.; Dudbridge, F.; Kent, L.; Wheelwright, S.; Hill-Cawthorne, G.; Allison, C.; Banerjee-Basu, S.; Baron-Cohen, S. (2009). "Genes related to sex steroids, neural growth, and social-emotional behavior are associated with autistic traits, empathy, and Asperger syndrome". Autism Research. 2 (3): 157–77. doi:10.1002/aur.80. PMID 19598235.
- ^ a b Jamain, Stéphane; Quach, Hélène; Betancur, Catalina; Råstam, Maria; Colineaux, Catherine; Gillberg, I. Carina; Soderstrom, Henrik; et al. (2003). "Mutations of the X-linked genes encoding neuroligins NLGN3 and NLGN4 are associated with autism". Nature Genetics. 34 (1): 27–9. doi:10.1038/ng1136. PMC 1925054. PMID 12669065.
{{cite journal}}: Explicit use of et al. in:|last8=(help) - ^ Durand, Christelle M; Betancur, Catalina; Boeckers, Tobias M; Bockmann, Juergen; Chaste, Pauline; Fauchereau, Fabien; Nygren, Gudrun; et al. Carina (2006). "Mutations in the gene encoding the synaptic scaffolding protein SHANK3 are associated with autism spectrum disorders". Nature Genetics. 39 (1): 25–7. doi:10.1038/ng1933. PMC 2082049. PMID 17173049.
- ^ Dwivedi, Yogesh (2009). "Brain-derived neurotrophic factor: Role in depression and suicide". Neuropsychiatric Disease and Treatment. 5: 433–49. doi:10.2147/NDT.S5700. PMC 2732010. PMID 19721723.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Brunoni, André Russowsky; Lopes, Mariana; Fregni, Felipe (2008). "A systematic review and meta-analysis of clinical studies on major depression and BDNF levels: Implications for the role of neuroplasticity in depression". The International Journal of Neuropsychopharmacology. 11 (8): 1169–80. doi:10.1017/S1461145708009309. PMID 18752720.
- ^ Xiu, Mei Hong; Hui, Li; Dang, Yu Feng; De Hou, Tian; Zhang, Chong Xi; Zheng, You Lan; Chen, Da Chun; et al. (2009). "Decreased serum BDNF levels in chronic institutionalized schizophrenia on long-term treatment with typical and atypical antipsychotics". Progress in Neuro-Psychopharmacology and Biological Psychiatry. 33 (8): 1508–12. doi:10.1016/j.pnpbp.2009.08.011. PMID 19720106.
{{cite journal}}: Explicit use of et al. in:|last8=(help) - ^ Maina, Giuseppe; Rosso, Gianluca; Zanardini, Roberta; Bogetto, Filippo; Gennarelli, Massimo; Bocchio-Chiavetto, Luisella (2010). "Serum levels of brain-derived neurotrophic factor in drug-naïve obsessive–compulsive patients: A case–control study". Journal of Affective Disorders. 122 (1–2): 174–8. doi:10.1016/j.jad.2009.07.009. PMID 19664825.
- ^ Zuccato, Chiara; Cattaneo, Elena (2009). "Brain-derived neurotrophic factor in neurodegenerative diseases". Nature Reviews Neurology. 5 (6): 311–22. doi:10.1038/nrneurol.2009.54. PMID 19498435.
- ^ Zajac, M.S.; Pang, T.Y.C.; Wong, N.; Weinrich, B.; Leang, L.S.K.; Craig, J.M.; Saffery, R.; Hannan, A.J. (2009). "Wheel running and environmental enrichment differentially modify exon-specific BDNF expression in the hippocampus of wild-type and pre-motor symptomatic male and female Huntington's disease mice". Hippocampus. 20 (5): NA. doi:10.1002/hipo.20658. PMID 19499586.
- ^ Zeev, B. B.; Bebbington, A.; Ho, G.; Leonard, H.; De Klerk, N.; Gak, E.; Vecksler, M.; Christodoulou, J. (2009). "The common BDNF polymorphism may be a modifier of disease severity in Rett syndrome". Neurology. 72 (14): 1242–7. doi:10.1212/01.wnl.0000345664.72220.6a. PMC 2677489. PMID 19349604.
- ^ Arancio, Ottavio; Chao, Moses V (2007). "Neurotrophins, synaptic plasticity and dementia". Current Opinion in Neurobiology. 17 (3): 325–30. doi:10.1016/j.conb.2007.03.013. PMID 17419049.
- ^ Mercader, Josep M.; FernÁNdez-Aranda, Fernando; GratacÒs, MÒNica; RibasÉs, Marta; BadÍa, Anna; Villarejo, Cynthia; Solano, Raquel; et al. (2007). "Blood Levels of Brain-Derived Neurotrophic Factor Correlate with Several Psychopathological Symptoms in Anorexia Nervosa Patients". Neuropsychobiology. 56 (4): 185–90. doi:10.1159/000120623. PMID 18337636.
{{cite journal}}: Explicit use of et al. in:|last8=(help)CS1 maint: multiple names: authors list (link) - ^ Kaplan, Allan S.; Levitan, Robert D.; Yilmaz, Zeynep; Davis, Caroline; Tharmalingam, Subi; Kennedy, James L. (2008). "A DRD4/BDNF gene–gene interaction associated with maximum BMI in women with bulimia nervosa". International Journal of Eating Disorders. 41 (1): 22–8. doi:10.1002/eat.20474. PMID 17922530.
- ^ Schwarz, E; Guest, P C; Rahmoune, H; Wang, L; Levin, Y; Ingudomnukul, E; Ruta, L; et al. (2010). "Sex-specific serum biomarker patterns in adults with Asperger's syndrome". Molecular Psychiatry. 16 (12): 1213–20. doi:10.1038/mp.2010.102. PMID 20877284.
{{cite journal}}: Explicit use of et al. in:|last8=(help) - ^ Nishimura, Katsuhiko; Nakamura, Kazuhiko; Anitha, A.; Yamada, Kazuo; Tsujii, Masatsugu; Iwayama, Yoshimi; Hattori, Eiji; et al. (2007). "Genetic analyses of the brain-derived neurotrophic factor (BDNF) gene in autism". Biochemical and Biophysical Research Communications. 356 (1): 200–6. doi:10.1016/j.bbrc.2007.02.135. PMID 17349978.
{{cite journal}}: Explicit use of et al. in:|last8=(help) - ^ Antoni, Ferenc A.; Holmes, Megan C.; Makara, Gábor B.; Kárteszi, Mihály; László, Ferenc A. (1984). "Evidence that the effects of arginine-8-vasopressin (AVP) on pituitary corticotropin (ACTH) release are mediated by a novel type of receptor". Peptides. 5 (3): 519–22. doi:10.1016/0196-9781(84)90080-9. PMID 6089144.
- ^ Hernando, F.; Schoots, O; Lolait, SJ; Burbach, JP (2001). "Immunohistochemical Localization of the Vasopressin V1b Receptor in the Rat Brain and Pituitary Gland: Anatomical Support for Its Involvement in the Central Effects of Vasopressin". Endocrinology. 142 (4): 1659–68. doi:10.1210/en.142.4.1659. PMID 11250948.
- ^ Young, W.S.; Li, J.; Wersinger, S.R.; Palkovits, M. (2006). "The vasopressin 1b receptor is prominent in the hippocampal area CA2 where it is unaffected by restraint stress or adrenalectomy". Neuroscience. 143 (4): 1031–9. doi:10.1016/j.neuroscience.2006.08.040. PMC 1748954. PMID 17027167.
- ^ Ma, D.Q.; Whitehead, P.L.; Menold, M.M.; Martin, E.R.; Ashley-Koch, A.E.; Mei, H.; Ritchie, M.D.; et al. (2005). "Identification of Significant Association and Gene-Gene Interaction of GABA Receptor Subunit Genes in Autism". The American Journal of Human Genetics. 77 (3): 377–88. doi:10.1086/433195. PMC 1226204. PMID 16080114.
{{cite journal}}: Explicit use of et al. in:|last8=(help) - ^ Nurmi, Erika L.; Dowd, Michael; Tadevosyan-Leyfer, Ovsanna; Haines, Jonathan L.; Folstein, Susan E.; Sutcliffe, James S. (2003). "Exploratory Subsetting of Autism Families Based on Savant Skills Improves Evidence of Genetic Linkage to 15q11-q13". Journal of the American Academy of Child & Adolescent Psychiatry. 42 (7): 856–63. doi:10.1097/01.CHI.0000046868.56865.0F. PMID 12819446.
- ^ Delorey, T; Sahbaie, P; Hashemi, E; Homanics, G; Clark, J (2008). "Gabrb3 gene deficient mice exhibit impaired social and exploratory behaviors, deficits in non-selective attention and hypoplasia of cerebellar vermal lobules: A potential model of autism spectrum disorder". Behavioural Brain Research. 187 (2): 207–20. doi:10.1016/j.bbr.2007.09.009. PMC 2684890. PMID 17983671.
- ^ Kõks, Sulev; Planken, Anu; Luuk, Hendrik; Vasar, Eero (2002). "Cat odour exposure increases the expression of wolframin gene in the amygdaloid area of rat". Neuroscience Letters. 322 (2): 116–20. doi:10.1016/S0304-3940(02)00110-6. PMID 11958857.
- ^ Andari, E.; Duhamel, J.-R.; Zalla, T.; Herbrecht, E.; Leboyer, M.; Sirigu, A. (2010). "Promoting social behavior with oxytocin in high-functioning autism spectrum disorders". Proceedings of the National Academy of Sciences. 107 (9): 4389–94. doi:10.1073/pnas.0910249107. PMC 2840168. PMID 20160081.
- ^ Hollander, Eric; Novotny, Sherie; Hanratty, Margaret; Yaffe, Rona; Decaria, Concetta M; Aronowitz, Bonnie R; Mosovich, Serge (2003). "Oxytocin Infusion Reduces Repetitive Behaviors in Adults with Autistic and Asperger's Disorders". Neuropsychopharmacology. 28 (1): 193–8. doi:10.1038/sj.npp.1300021. PMID 12496956.
- ^ Gever, John (February 15, 2010). "Oxytocin Shows Promise in Autism". ABC News. p. 2. Retrieved October 22, 2012.
- ^ Yrigollen, Carolyn M.; Han, Summer S.; Kochetkova, Anna; Babitz, Tammy; Chang, Joseph T.; Volkmar, Fred R.; Leckman, James F.; Grigorenko, Elena L. (2008). "Genes Controlling Affiliative Behavior as Candidate Genes for Autism". Biological Psychiatry. 63 (10): 911–6. doi:10.1016/j.biopsych.2007.11.015. PMC 2386897. PMID 18207134.
- ^ Kilpinen, H; Ylisaukko-Oja, T; Hennah, W; Palo, O M; Varilo, T; Vanhala, R; Nieminen-Von Wendt, T; et al. (2007). "Association of DISC1 with autism and Asperger syndrome". Molecular Psychiatry. 13 (2): 187–96. doi:10.1038/sj.mp.4002031. PMID 17579608.
{{cite journal}}: Explicit use of et al. in:|last8=(help) - ^ Rinehart NJ, Bradshaw JL, Moss SA, Brereton AV, Tonge BJ (March 2001). "A deficit in shifting attention present in high-functioning autism but not Asperger's disorder". Autism. 5 (1): 67–80. doi:10.1177/1362361301005001007. PMID 11708391.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ghaziuddin M (April 2005). "A family history study of Asperger syndrome". J Autism Dev Disord. 35 (2): 177–82. doi:10.1007/s10803-004-1996-4. PMID 15909404.
- ^ Vasa RA, Anderson C, Marvin AR; et al. (2012). "Mood disorders in mothers of children on the autism spectrum are associated with higher functioning autism". Autism Res Treat. 2012: 435646. doi:10.1155/2012/435646. PMC 3426171. PMID 22934172.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ^ Barbeau EB, Soulières I, Dawson M, Zeffiro TA, Mottron L (February 2013). "The level and nature of autistic intelligence III: Inspection time". J Abnorm Psychol. 122 (1): 295–301. doi:10.1037/a0029984. PMID 23088375.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ozonoff, S (1991). "Asperger's syndrome: Evidence for an empirical distinction from high-functioning autism". Journal of Child Psychology and Psychi. 32.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b c Markram, Henry; Markram, Kamila (2010). "The Intense World Theory – A Unifying Theory of the Neurobiology of Autism". Frontiers in Human Neuroscience. 4. doi:10.3389/fnhum.2010.00224.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Rumpf AL, Kamp-Becker I, Becker K, Kauschke C (2012). "Narrative competence and internal state language of children with Asperger Syndrome and ADHD". Res Dev Disabil. 33 (5): 1395–407. doi:10.1016/j.ridd.2012.03.007. PMID 22522198.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.huffingtonpost.com/kyle-simon/is-there-a-link-between-autism-and-gender-dysphoria_b_3896317.html
