Ventilator
It has been suggested that this article be merged into Mechanical ventilation. (Discuss) Proposed since April 2020. |
| Ventilator | |
|---|---|
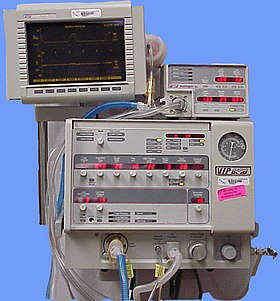 The Bird VIP Infant ventilator | |
| Specialty | Pulmonology |
A ventilator is a machine that provides mechanical ventilation by moving breathable air into and out of the lungs, to deliver breaths to a patient who is physically unable to breathe, or breathing insufficiently. Modern ventilators are computerized microprocessor-controlled machines, but patients can also be ventilated with a simple, hand-operated bag valve mask. Ventilators are chiefly used in intensive-care medicine, home care, and emergency medicine (as standalone units) and in anesthesiology (as a component of an anesthesia machine).
Ventilators are sometimes called "respirators", a term commonly used for them in the 1950s (particularly the "Bird respirator"). However, contemporary hospital and medical terminology uses the word "respirator" to refer to a protective face-mask.[1]
Function
In its simplest form, a modern positive pressure ventilator consists of a compressible air reservoir or turbine, air and oxygen supplies, a set of valves and tubes, and a disposable or reusable "patient circuit". The air reservoir is pneumatically compressed several times a minute to deliver room-air, or in most cases, an air/oxygen mixture to the patient. If a turbine is used, the turbine pushes air through the ventilator, with a flow valve adjusting pressure to meet patient-specific parameters. When over pressure is released, the patient will exhale passively due to the lungs' elasticity, the exhaled air being released usually through a one-way valve within the patient circuit called the patient manifold.
Ventilators may also be equipped with monitoring and alarm systems for patient-related parameters (e.g. pressure, volume, and flow) and ventilator function (e.g. air leakage, power failure, mechanical failure), backup batteries, oxygen tanks, and remote control. The pneumatic system is nowadays often replaced by a computer-controlled turbopump.
Modern ventilators are electronically controlled by a small embedded system to allow exact adaptation of pressure and flow characteristics to an individual patient's needs. Fine-tuned ventilator settings also serve to make ventilation more tolerable and comfortable for the patient. In Canada and the United States, respiratory therapists are responsible for tuning these settings, while biomedical technologists are responsible for the maintenance. In the United Kingdom and Europe the management of the patient's interaction with the ventilator is done by critical care nurses.
The patient circuit usually consists of a set of three durable, yet lightweight plastic tubes, separated by function (e.g. inhaled air, patient pressure, exhaled air). Determined by the type of ventilation needed, the patient-end of the circuit may be either noninvasive or invasive.
Noninvasive methods, such as continuous positive airway pressure (CPAP) and non-invasive ventilation, which are adequate for patients who require a ventilator only while sleeping and resting, mainly employ a nasal mask. Invasive methods require intubation, which for long-term ventilator dependence will normally be a tracheotomy cannula, as this is much more comfortable and practical for long-term care than is larynx or nasal intubation.
Life-critical system
Because failure may result in death, mechanical ventilation systems are classified as life-critical systems, and precautions must be taken to ensure that they are highly reliable, including their power supply. Mechanical ventilators are therefore carefully designed so that no single point of failure can endanger the patient. They may have manual backup mechanisms to enable hand-driven respiration in the absence of power (such as the mechanical ventilator integrated into an anaesthetic machine). They may also have safety valves, which open to atmosphere in the absence of power to act as an anti-suffocation valve for spontaneous breathing of the patient. Some systems are also equipped with compressed-gas tanks, air compressors or backup batteries to provide ventilation in case of power failure or defective gas supplies, and methods to operate or call for help if their mechanisms or software fail.[2]
Major manufacturers
| Manufacturer | Country | Market share (2019) |
|---|---|---|
| Getinge | Sweden | 22% |
| Hamilton Medical | USA, Switzerland | 22% |
| Dräger | Germany | 16 % |
| Mindray | China | 10% |
| Medtronic | Ireland, USA | 5% |
| Löwenstein Medical | Germany | 3% |
| Vyaire Medical | USA | 3% |
| GE Healthcare | USA | 3% |
| Philips Respironics | Netherlands | 3% |
| Others | 15% |
| Manufacturer | Country | Market share (2019) |
|---|---|---|
| Dräger | Germany | 24 % |
| Weinmann Medical | Germany | 21 % |
| Hamilton Medical | USA, Switzerland | 18 % |
| Vyaire Medical | USA | 5 % |
| Customs | Japan | 4 % |
| O Two | Canada | 4 % |
| Smiths Medical | USA | 4 % |
| Medtronic | Ireland, USA | 4 % |
| Air Liquide Healthcare | France | 3 % |
| (and 13 other vendors contributing for 13 %) |
| Manufacturer | Country | City |
|---|---|---|
| Airon Corporation | USA | Melbourne, Florida |
| Avasarala Technologies Limited | India | Bengaluru |
| A B INDUSTRIES (MAX MEDITECH PVT LTD)[citation needed] | India | Vadodara |
| AgVa Healthcare[6] | India | |
| AEONMED CO., LTD. | China | Beijing |
| ACUTRONIC Medical Systems AG | Switzerland | Hirzel |
| aXcent medical | Germany | Koblenz |
| Becton Dickinson and Company | USA | Franklin Lakes, NJ |
| Biosys Medikal | Turkey | Ankara |
| Bio-Med Devices, Inc. | USA | Guilford, CT |
| Bunnell Incorporated | USA | Salt Lake City, UT |
| Cardinal Health | USA | Dublin, OH |
| Concern Radio-Electronic Technologies[7] | Russia | Moscow |
| Dima Italia | Italy | Bologna |
| Fisher & Paykel | New Zealand | Auckland |
| Getinge AB | Sweden | Göteborg |
| Hartwell Medical Corp. | USA | Carlsbad, CA |
| Hillrom | USA | Chicago, IL |
| Oceanic Medical Products, Inc. | USA | Atchison, KS |
| ResMed Corp. | USA | San Diego, CA |
| Smiths Group | UK | London |
| Triton Electronics Systems, Ltd. | Russia | Yekaterinburg |
| United Hayek Industries, Inc. | USA | San Diego, CA |
| Ventec Life Systems | USA | Bothell, WA |
History
This section needs additional citations for verification. (April 2020) |
The history of mechanical ventilation begins with various versions of what was eventually called the iron lung, a form of noninvasive negative-pressure ventilator widely used during the polio epidemics of the twentieth century after the introduction of the "Drinker respirator" in 1928, improvements introduced by John Haven Emerson in 1931,[8] and the Both respirator in 1937. Other forms of noninvasive ventilators, also used widely for polio patients, include Biphasic Cuirass Ventilation, the rocking bed, and rather primitive positive pressure machines.[8]
In 1949, John Haven Emerson developed a mechanical assister for anaesthesia with the cooperation of the anaesthesia department at Harvard University. Mechanical ventilators began to be used increasingly in anaesthesia and intensive care during the 1950s. Their development was stimulated both by the need to treat polio patients and the increasing use of muscle relaxants during anaesthesia. Relaxant drugs paralyse the patient and improve operating conditions for the surgeon but also paralyse the respiratory muscles.

In the United Kingdom, the East Radcliffe and Beaver models were early examples. The former used a Sturmey-Archer bicycle hub gear to provide a range of speeds, and the latter an automotive windscreen wiper motor to drive the bellows used to inflate the lungs.[9] Electric motors were, however, a problem in the operating theatres of that time, as their use caused an explosion hazard in the presence of flammable anaesthetics such as ether and cyclopropane. In 1952, Roger Manley of the Westminster Hospital, London, developed a ventilator which was entirely gas-driven and became the most popular model used in Europe. It was an elegant design, and became a great favourite with European anaesthetists for four decades, prior to the introduction of models controlled by electronics. It was independent of electrical power and caused no explosion hazard. The original Mark I unit was developed to become the Manley Mark II in collaboration with the Blease company, which manufactured many thousands of these units. Its principle of operation was very simple, an incoming gas flow was used to lift a weighted bellows unit, which fell intermittently under gravity, forcing breathing gases into the patient's lungs. The inflation pressure could be varied by sliding the movable weight on top of the bellows. The volume of gas delivered was adjustable using a curved slider, which restricted bellows excursion. Residual pressure after the completion of expiration was also configurable, using a small weighted arm visible to the lower right of the front panel. This was a robust unit and its availability encouraged the introduction of positive pressure ventilation techniques into mainstream European anesthetic practice.
The 1955 release of Forrest Bird's "Bird Universal Medical Respirator" in the United States changed the way mechanical ventilation was performed, with the small green box becoming a familiar piece of medical equipment.[10] The unit was sold as the Bird Mark 7 Respirator and informally called the "Bird". It was a pneumatic device and therefore required no electrical power source to operate.
In 1965, the Army Emergency Respirator was developed in collaboration with the Harry Diamond Laboratories (now part of the U.S. Army Research Laboratory) and Walter Reed Army Institute of Research. Its design incorporated the principle of fluid amplification in order to govern pneumatic functions. Fluid amplification allowed the respirator to be manufactured entirely without moving parts, yet capable of complex resuscitative functions.[11] Elimination of moving parts increased performance reliability and minimized maintenance.[12] The mask is composed of a poly(methyl methacrylate) (commercially known as Lucite) block, about the size of a pack of cards, with machined channels and a cemented or screwed-in cover plate.[13] The reduction of moving parts cut manufacturing costs and increased durability.[12]
The bistable fluid amplifier design allowed the respirator to function as both a respiratory assistor and controller. It could functionally transition between assistor and controller automatically, based on the patient's needs.[13][12] The dynamic pressure and turbulent jet flow of gas from inhalation to exhalation allowed the respirator to synchronize with the breathing of the patient.[14]
Intensive care environments around the world revolutionized in 1971 by the introduction of the first SERVO 900 ventilator (Elema-Schönander), constructed by Björn Jonson. It was a small, silent and effective electronic ventilator, with the famous SERVO feedback system controlling what had been set and regulating delivery. For the first time, the machine could deliver the set volume in volume control ventilation.
Ventilators used under increased pressure (hyperbaric) require special precautions, and few ventilators can operate under these conditions.[15] In 1979, Sechrist Industries introduced their Model 500A ventilator, which was specifically designed for use with hyperbaric chambers.[16]
Microprocessor ventilators
Microprocessor control led to the third generation of intensive care unit (ICU) ventilators, starting with the Dräger EV-A[17] in 1982 in Germany which allowed monitoring the patient's breathing curve on an LCD monitor. One year later followed Puritan Bennett 7200 and Bear 1000, SERVO 300 and Hamilton Veolar over the next decade. Microprocessors enable customized gas delivery and monitoring, and mechanisms for gas delivery that are much more responsive to patient needs than previous generations of mechanical ventilators.[18]
Open-source ventilators
An open-source ventilator is a disaster-situation ventilator made using a freely-licensed design, and ideally, freely-available components and parts. Designs, components, and parts may be anywhere from completely reverse-engineered to completely new creations, components may be adaptations of various inexpensive existing products, and special hard-to-find and/or expensive parts may be 3D printed instead of sourced.[19][20]
During the 2019-2020 COVID-19 pandemic, various kinds of ventilators have been considered. Deaths caused by COVID-19 have occurred when the most severely infected experience acute respiratory distress syndrome, a widespread inflammation in the lungs that impairs the lungs' ability to absorb oxygen and expel carbon dioxide. These patients require a capable ventilator to continue breathing.
Among ventilators that might be brought into the COVID-19 fight, there have been many concerns. These include current availability,[21][22] the challenge of making more and lower cost ventilators,[23] effectiveness,[24] functional design, safety,[25][26] portability,[27] suitability for infants,[28] assignment to treat other illnesses,[29] and operator training.[30] Deploying the best possible mix of ventilators can save the most lives.
Although not formally open-sourced, the Ventec V+ Pro ventilator was developed in April 2020 as a shared effort between Ventec Life Systems and General Motors, to provide a rapid supply of 30,000 ventilators capable of treating COVID-19 patients[31][32].
A major worldwide design effort began during the 2019-2020 coronavirus pandemic after a Hackaday project was started,[33][non-primary source needed] in order to respond to expected ventilator shortages causing higher mortality rate among severe patients.
On March 20, 2020, the Irish Health Service[34] began reviewing designs.[35] A prototype is being designed and tested in Colombia.[36].
The Polish company Urbicum reports successful testing[37] of a 3D-printed open-source prototype device called VentilAid. The makers describe it as a last resort device when professional equipment is missing. The design is publicly available.[38] The first Ventilaid prototype requires compressed air to run.
On March 21, 2020 the New England Complex Systems Institute (NECSI) began maintaining a strategic list of open source designs being worked on.[39][40] The NECSI project considers manufacturing capability, medical safety and need for treating patients in various conditions, speed dealing with legal and political issues, logistics and supply.[41] NECSI is staffed with scientists from Harvard and MIT and others who have an understanding of pandemics, medicine, systems, risk, and data collection.[41]
The University of Minnesota Bakken Medical Device Center initiated a collaboration with various companies to bring a ventilator alternative to the market that works as a one-armed robot and replaces the need for manual ventilation in emergency situations. The Coventor device was developed in a very short time and approved on April 15, 2020 by the FDA, only 30 days after conception. The mechanical ventilator is designed for use by trained medical professionals in intensive care units and easy to operate. It has a compact design and is relatively inexpensive to manufacture and distribute. The cost is only about 4% of a normal ventilator. In addition, this device does not require pressurized oxygen or air supply, as is normally the case. A first series is manufactured by Boston Scientific. The plans are to be freely available online to the general public without royalties.[42][43]
COVID-19 pandemic
The COVID-19 pandemic has led to shortages of essential goods and services - from hand sanitizers to masks to beds to ventilators. Several countries have already experienced a shortage of ventilators.[44]
In 2006 (under President George W. Bush), the Biomedical Advanced Research and Development Authority (BARDA) of the United States realized that the country was likely to have an epidemic of respiratory disease and would need more ventilators, so it awarded a $6 million contract to Newport Medical Instruments, a small company in California, to make 40,000 ventilators for under $3,000 apiece. In 2011, Newport sent three prototypes to the Centers for Disease Control. In 2012, Covidien, a $12 billion/year medical device manufacturer, which manufactured more expensive competing ventilators, bought Newport for $100 million. Covidien delayed and in 2014 cancelled the contract.
BARDA started over again with a new company, Philips, and in July 2019, the FDA approved the Philips ventilator, and the government ordered 10,000 ventilators for delivery in mid-2020.[45]
On April 23, 2020, NASA reported building, in 37 days, a successful COVID-19 ventilator, named VITAL ("Ventilator Intervention Technology Accessible Locally"). On April 30, NASA reported receiving fast-track approval for emergency use by the United States Food and Drug Administration for the new ventilator.[46][47][48] On May 29, NASA reported that eight manufacturers were selected to manufacture the new ventilator.[49]
Fifty-four governments, including many in Europe and Asia, imposed restrictions on medical supply exports in response to the coronavirus pandemic.[50]
See also
- Artificial ventilation
- Joseph Stoddart
- Open-source hardware
- Respiratory therapy
- Robert Martensen
- Two-balloon experiment
References
- ^ Center for Devices and Radiological Health (2019-02-08). "Personal Protective Equipment for Infection Control - Masks and N95 Respirators". FDA. Retrieved 2017-03-08.
- ^ Johnson, Carolyn Y.; reporterEmailEmailBioBioFollowFollow, closeCarolyn Y. JohnsonScience reporterEmailEmailBioBioFollowFollowAriana Eunjung Cha closeAriana Eunjung ChaNational. "The dark side of ventilators: Those hooked up for long periods face difficult recoveries". Washington Post. Retrieved 8 April 2020.
- ^ Giorgio V. Müller (2020-03-30). "Hersteller von Beatmungsgeräten produzieren massiv mehr, aber können die Nachfrage trotzdem nicht decken". Neue Zürcher Zeitung (in German). Retrieved 2020-03-30.
{{cite news}}: CS1 maint: url-status (link) With reference to: IPG Research. - ^ Müller, Giorgio V. (2020-03-30). "Hersteller von Beatmungsgeräten produzieren massiv mehr, aber können die Nachfrage trotzdem nicht decken". Neue Zürcher Zeitung (in German). Retrieved 2020-03-30.
{{cite news}}: CS1 maint: url-status (link) With reference to: IPG Research. - ^ "Medical Ventilator Manufacturers and Companies". Retrieved 17 April 2020.
- ^ "Battle against coronavirus: Maruti ties up with AgVA Healthcare to produce 10,000 ventilators per month". Retrieved 20 April 2020.
- ^ "Rostec will increase by 18% the supply of the ventilator for the Russian health care". Retrieved 20 April 2020.
- ^ a b Geddes, LA (2007). "The history of artificial respiration". IEEE Engineering in Medicine and Biology Magazine. 26 (6): 38–41. doi:10.1109/EMB.2007.907081. PMID 18189086.
- ^ Russell WR, Schuster E, Smith AC, Spalding JM (April 1956). "Radcliffe respiration pumps". The Lancet. 270 (6922): 539–41. doi:10.1016/s0140-6736(56)90597-9. PMID 13320798.
- ^ Bellis, Mary. "Forrest Bird invented a fluid control device, respirator & pediatric ventilator". About.com. Retrieved 2009-06-04.
- ^ Army R, D & A. Development and Engineering Directorate, HQ, U.S. Army Materiel Development and Readiness Command. 1965.
- ^ a b c Mon, George; Woodward, Kenneth E.; Straub, Henrik; Joyce, James; Meyer, James (1966). "Fluid Amplifier-Controlled Medical Devices". SAE Transactions. 74: 217–222. ISSN 0096-736X. JSTOR 44554326.
- ^ a b "Army Research and Development Monthly Magazine" (PDF).
- ^ "Fluid Amplification Symposium" (PDF). October 1965.
- ^ Skinner, M (1998). "Ventilator function under hyperbaric conditions". South Pacific Underwater Medicine Society Journal. 28 (2). Retrieved 2009-06-04.
- ^ Weaver LK, Greenway L, Elliot CG (1988). "Performance of the Seachrist 500A Hyperbaric Ventilator in a Monoplace Hyperbaric Chamber". Journal of Hyperbaric Medicine. 3 (4): 215–225. Retrieved 2009-06-04.
- ^ "Dräger - die Geschichte des Unternehmens" (PDF). Dräger. Dräger. Retrieved March 22, 2020.
- ^ Kacmarek, Robert M. (August 2011). "The Mechanical Ventilator: Past, Present, and Future". Respiratory Care. 56 (8): 1170–1180. doi:10.4187/respcare.01420. ISSN 0020-1324. PMID 21801579.
- ^ Bender, Maddie (2020-03-17). "People Are Trying to Make DIY Ventilators to Meet Coronavirus Demand". Vice. Retrieved 2020-03-21.
- ^ Toussaint, Kristin (2020-03-16). "These Good Samaritans with a 3D printer are saving lives by making new respirator valves for free". Fast Company. Retrieved 2020-03-17.
- ^ NEIGHMOND, PATTI (March 14, 2020). "As The Pandemic Spreads, Will There Be Enough Ventilators?". NPR. Retrieved April 6, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ Parker, Thomas (March 25, 2020). "880,000 more ventilators needed to cope with coronavirus outbreak, says analyst". NS Medical Devices. Retrieved April 6, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "A Guide To Designing Low-Cost Ventilators for COVID-19". YouTube. Real Engineering. April 4, 2020. Retrieved April 6, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "Mortality rate of COVID-19 patients on ventilators". Physician's Weekly. March 30, 2020. Retrieved April 6, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "SAFE INITIATION AND MANAGEMENT OF MECHANICAL VENTILATION" (PDF). American Association for Respiratory Care. 2016. Retrieved April 6, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "Mechanical Ventilation of SARS Patients: Lessons from the 2003 SARS Outbreak". ECRI. February 18, 2020. Retrieved April 6, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ Etherington, Darrell (March 30, 2020). "Medtronic is sharing its portable ventilator design specifications and code for free to all". TechCrunch. Retrieved April 6, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "Bird V.I.P Standard Infant and Pediatric Ventilator". BemesOnline. Retrieved April 6, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ Iftikhar, Noreen (September 23, 2019). "When a ventilator is used". Healthline. Retrieved April 6, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ Williams, LM (January 30, 2020). "Ventilator Safety" (Document). StatPearls Publishing.
{{cite document}}: Unknown parameter|pmid=ignored (help) - ^ Welch, David (April 8, 2020). "GM Lands U.S. Ventilator Contract Worth Almost $500 Million". Bloomberg.
{{cite web}}: CS1 maint: url-status (link) - ^ "60 Minutes". CBS. April 26, 2020. On the Line, Outbreak Science, The Unseen Enemy, S52 E30, At 7 minutes 10 seconds.
{{cite web}}: CS1 maint: url-status (link) - ^ Coetzee, Gerrit (2020-03-12). "Ultimate Medical Hackathon: How Fast Can We Design And Deploy An Open Source Ventilator?". Hackaday. Retrieved 2020-03-17.
- ^ Sternlicht, Alexandra. "There's A Shortage Of Ventilators For Coronavirus Patients, So This International Group Invented An Open Source Alternative That's Being Tested Next Week". Forbes. Retrieved 2020-03-21.
- ^ Rodrigo, Chris Mills (2020-03-20). "Irish health officials to review 3D-printed ventilator". TheHill. Retrieved 2020-03-21.
- ^ colombiareports (2020-03-21). "Colombia close to having world's first open source and low-cost ventilator to 'beat Covid-19'". Colombia News | Colombia Reports. Retrieved 2020-03-21.
- ^ urbicum (2020-03-23). "VentilAid -open-source ventilator, that can be made anywhere locally". VentilAid. Retrieved 2020-03-23.
- ^ urbicum (2020-03-23). "GitLab - VentilAid / VentilAid". VentilAid. Retrieved 2020-03-23.
- ^ Fenton, Bruce (March 21, 2020). "Ventilator Project Update: March 21th, 2020". Medium. Retrieved March 27, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ "A list projects to make emergency ventilators in response to COVID-19, focusing on free-libre open source". GitHub. Retrieved March 27, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ a b Fenton, Bruce (March 14, 2020). "We need Ventilators - We Need You to Help Get Them Built". Medium. Retrieved March 27, 2020.
{{cite web}}: CS1 maint: url-status (link) - ^ Joe Carlson (2020-04-16). "FDA approves production of device designed at University of Minnesota to help COVID-19 patients breathe". startribune.com. Star Tribune.
- ^ Darrell Etherington (2020-04-16). "FDA authorizes production of a new ventilator that costs up to 25x less than existing devices". techcrunch.com. Verizon Media.
- ^ "Allocating Ventilators in a Pandemic". healthmanagement.org. 2020-03-24. Retrieved 2020-03-25.
- ^ Nicholas Kulish, Sarah Kliff and Jessica Silver-Greenberg (March 29, 2020). "The U.S. Tried to Build a New Fleet of Ventilators. The Mission Failed. As the coronavirus spreads, the collapse of the project helps explain America's acute shortage". New York Times.
- ^ Inclán, Bettina; Rydin, Matthew; Northon, Karen; Good, Andrew (30 April 2020). "NASA-Developed Ventilator Authorized by FDA for Emergency Use". NASA. Retrieved 1 May 2020.
- ^ Good, Andrew; Greicius, Tony (April 23, 2020). "NASA Develops COVID-19 Prototype Ventilator in 37 Days". NASA. Retrieved April 24, 2020.
- ^ Wall, Mike (April 24, 2020). "NASA engineers build new COVID-19 ventilator in 37 days". Space.com. Retrieved April 24, 2020.
- ^ Inclán, Bettina; Rydin, Matthew; Northon, Karen; Good, Andrew (May 29, 2020). "Eight US Manufacturers Selected to Make NASA COVID-19 Ventilator". NASA. Retrieved May 29, 2020.
- ^ "Export restrictions threaten ventilator availability". politico.com. 2020-03-24. Retrieved 2020-03-25.



