Dysautonomia
| Dysautonomia | |
|---|---|
| Other names | Autonomic dysfunction |
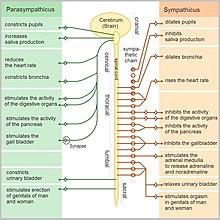 | |
| The autonomic nervous system | |
| Specialty | Neurology |
| Symptoms | Anxiety[1] |
| Causes | Inadequacy of sympathetic, or parasympathetic, components of autonomic nervous system[2] |
| Risk factors | Alcoholism and Diabetes[3] |
| Diagnostic method | Ambulatory Blood pressure, as well as EKG monitoring[4] |
| Treatment | Symptomatic and supportive[2] |
Dysautonomia or autonomic dysfunction is a condition in which the autonomic nervous system (ANS) does not work properly. This may affect the functioning of the heart, bladder, intestines, sweat glands, pupils, and blood vessels. Dysautonomia has many causes, not all of which may be classified as neuropathic.[5] A number of conditions can feature dysautonomia, such as Parkinson's disease, HIV/AIDS, multiple system atrophy, autonomic failure, postural orthostatic tachycardia syndrome, Ehlers-Danlos syndrome,[6] autoimmune autonomic ganglionopathy, and autonomic neuropathy.[citation needed]
The diagnosis is achieved through functional testing of the ANS, focusing on the affected organ system. Investigations may be performed to identify underlying disease processes that may have led to the development of symptoms or autonomic neuropathy. Symptomatic treatment is available for many symptoms associated with dysautonomia, and some disease processes can be directly treated.[7]
Signs and symptoms
The symptoms of dysautonomia, which are numerous and vary widely for each individual, are due to inefficient or unbalanced efferent signals sent via both systems. The primary symptoms in individuals with dysautonomia include
- Anhydrosis[1]
- Anxiety[4]
- Blurry or double vision[1]
- Bowel incontinence[1]
- Brain fog[1]
- Constipation[4]
- Dizziness[4]
- Difficulty swallowing[8]
- Exercise intolerance[1]
- Insomnia[4]
- Low blood pressure[4]
- Orthostatic hypotension[1]
- Syncope[4]
- Tachycardia[5]
- Tunnel vision[4]
- Urinary incontinence or urinary retention[1]
- Vertigo[4]
- Weakness[4]
Causes

Dysautonomia may be due to inherited or degenerative neurologic diseases (primary dysautonomia)[5] or it may occur due to injury of the autonomic nervous system from an acquired disorder (secondary dysautonomia).[1][9] The most common causes of dysautonomia include
- Alcoholism[8]
- Amyloidosis[4]
- Autoimmune disease, such as Sjögren's syndrome or systemic lupus erythematosus (lupus), and autoimmune autonomic ganglionopathy[citation needed]
- Craniocervical instability[8]
- Diabetes[8]
- Eaton-Lambert syndrome[4]
- Ehlers-Danlos syndrome[10]
- Guillain-Barré syndrome[8]
- HIV and AIDS[8]
- Lyme disease[4]
- Multiple sclerosis[8]
- Multiple system atrophy
- Paraneoplastic syndrome[11]
- Parkinson's disease[8]
- Spinal cord injury[8]
- Surgery or injury involving the nerves[8]
- Toxicity (vincristine)[4]
In the sympathetic nervous system (SNS), predominant dysautonomia is common along with fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and interstitial cystitis, raising the possibility that such dysautonomia could be their common clustering underlying pathogenesis.[12]
In addition to sometimes being a symptom of dysautonomia, anxiety can sometimes physically manifest symptoms resembling autonomic dysfunction.[13][14][15] A thorough investigation ruling out physiological causes is crucial, but in cases where relevant tests are performed and no causes are found or symptoms do not match any known disorders, a primary anxiety disorder is possible, but should not be presumed.[16] For such patients, the anxiety sensitivity index may have better predictivity for anxiety disorders, while the Beck anxiety inventory may misleadingly suggest anxiety for patients with dysautonomia.[17]
Mechanism
The autonomic nervous system is a component of the peripheral nervous system and comprises two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PSNS). The SNS controls the more active responses such as increasing heart rate and blood pressure. The PSNS slows down the heart rate and aids in digestion, for example. Symptoms typically arise from abnormal responses of either the sympathetic or parasympathetic systems based on situation or environment.[5][18]
Diagnosis

The diagnosis of dysautonomia depends on the overall function of three autonomic functions – cardiovagal, adrenergic, and sudomotor. A diagnosis should, at a bare minimum, include measurements of blood pressure and heart rate while lying flat, and after at least 3 minutes of standing. The best way to achieve a diagnosis includes a range of testing, notably an autonomic reflex screen, tilt table test, and testing of the sudomotor response (QSART or thermoregulatory sweat test).[19]
Additional tests and examinations to determine a diagnosis of dysautonomia include
- Ambulatory blood pressure and EKG monitoring[4]
- Cold pressor test[19]
- Deep breathing[19]
- Hyperventilation test[19]
- Nerve biopsy for small fiber neuropathy[1]
- Quantitative sudomotor axon reflex test (QSART)[19]
- Testing for orthostatic intolerance[19]
- Thermoregulatory sweat test[19]
- Tilt table test[19]
- Valsalva maneuver[19]
Tests to elucidate the cause of dysautonomia can include:
- Evaluation for acute (intermittent) porphyria.[1]
- Evaluation of cerebrospinal fluid by lumbar puncture[1]
Vegetative-vascular dystonia
Particularly in the Russian literature,[20] a subtype of dysautonomia which particularly affects the vascular system has been called vegetative-vascular dystonia.[21][22][23][24][25] The term "vegetative" reflects an older name for the autonomic nervous system: the vegetative nervous system.[citation needed]
Management

The treatment of dysautonomia can be difficult; since it is made up of many different symptoms, a combination of drug therapies is often required to manage individual symptomatic complaints. Therefore, if an autoimmune neuropathy is the case, then treatment with immunomodulatory therapies is done, or if diabetes mellitus is the cause, control of blood glucose is important.[1] Treatment can include proton-pump inhibitors and H2 receptor antagonists used for digestive symptoms such as acid reflux.[26]
For the treatment of genitourinary autonomic neuropathy medications may include sildenafil (a guanine monophosphate type-5 phosphodiesterase inhibitor). For the treatment of hyperhidrosis, anticholinergic agents such as trihexyphenidyl or scopolamine can be used, also intracutaneous injection of botulinum toxin type A can be used for management in some cases.[27]
Balloon angioplasty, a procedure referred to as transvascular autonomic modulation, is specifically not approved for the treatment of autonomic dysfunction.[28]
Prognosis
The prognosis of dysautonomia depends on several factors; individuals with chronic, progressive, generalized dysautonomia in the setting of central nervous system degeneration such as Parkinson's disease or multiple system atrophy have a generally poorer long-term prognosis. Consequently, dysautonomia could be fatal due to pneumonia, acute respiratory failure, or sudden cardiopulmonary arrest.[5]
Autonomic dysfunction symptoms such as orthostatic hypotension, gastroparesis, and gustatory sweating are more frequently identified in mortalities.[29]
See also
References
- ^ a b c d e f g h i j k l m "Autonomic Neuropathy Clinical Presentation: History, Physical, Causes". emedicine.medscape.com. Retrieved 2016-02-21.
- ^ a b "Dysautonomia Information Page | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Retrieved 2 January 2018.
- ^ "Dysautonomia | Autonomic Nervous System Disorders | MedlinePlus". NIH. Retrieved 2 January 2018.
- ^ a b c d e f g h i j k l m n o "Autonomic Neuropathy. Information about AN. Patient | Patient". Patient. Retrieved 2016-02-21.
- ^ a b c d e "Dysautonomia". NINDS. Archived from the original on 2016-12-02. Retrieved 2012-04-03.
- ^ Castori M, Voermans NC (October 2014). "Neurological manifestations of Ehlers-Danlos syndrome(s): A review". Iranian Journal of Neurology. 13 (4): 190–208. PMC 4300794. PMID 25632331.
- ^ Iodice V, Kimpinski K, Vernino S, Sandroni P, Fealey RD, Low PA (June 2009). "Efficacy of immunotherapy in seropositive and seronegative putative autoimmune autonomic ganglionopathy". Neurology. 72 (23): 2002–8. doi:10.1212/WNL.0b013e3181a92b52. PMC 2837591. PMID 19506222.
- ^ a b c d e f g h i j "Autonomic neuropathy: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Retrieved 2016-02-20.
- ^ Kirk KA, Shoykhet M, Jeong JH, Tyler-Kabara EC, Henderson MJ, Bell MJ, Fink EL (August 2012). "Dysautonomia after pediatric brain injury". Developmental Medicine and Child Neurology. 54 (8): 759–64. doi:10.1111/j.1469-8749.2012.04322.x. PMC 3393822. PMID 22712762.
- ^ De Wandele I, Rombaut L, Leybaert L, Van de Borne P, De Backer T, Malfait F, et al. (August 2014). "Dysautonomia and its underlying mechanisms in the hypermobility type of Ehlers-Danlos syndrome". Seminars in Arthritis and Rheumatism. 44 (1): 93–100. doi:10.1016/j.semarthrit.2013.12.006. PMID 24507822.
- ^ "Paraneoplastic syndromes of the nervous system". Mayo Clinic. Mayo Clinic. Retrieved 13 September 2016.
- ^ Martínez-Martínez LA, Mora T, Vargas A, Fuentes-Iniestra M, Martínez-Lavín M (April 2014). "Sympathetic nervous system dysfunction in fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome, and interstitial cystitis: a review of case-control studies". Journal of Clinical Rheumatology. 20 (3): 146–50. doi:10.1097/RHU.0000000000000089. PMID 24662556.
- ^ Soliman K, Sturman S, Sarkar PK, Michael A (2010). "Postural orthostatic tachycardia syndrome (POTS): a diagnostic dilemma". British Journal of Cardiology. 17 (1): 36–9.
- ^ Ackerman, Kurt; DiMartini, Andrea F. (2015). Psychosomatic Medicine. Oxford University Press, Incorporated. ISBN 9780199329311.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Carr, Alan; McNulty, Muireann (2016-03-31). The Handbook of Adult Clinical Psychology: An Evidence Based Practice Approach. Routledge. ISBN 9781317576143.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Tasman, Allan; Kay, Jerald; First, Michael B .; Lieberman, Jeffrey A.; Riba, Michelle (2015-03-30). Psychiatry, 2 Volume Set. John Wiley & Sons. ISBN 9781118845479.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Raj V, Haman KL, Raj SR, Byrne D, Blakely RD, Biaggioni I, et al. (March 2009). "Psychiatric profile and attention deficits in postural tachycardia syndrome". Journal of Neurology, Neurosurgery, and Psychiatry. 80 (3): 339–44. doi:10.1136/jnnp.2008.144360. PMC 2758320. PMID 18977825.
{{cite journal}}:|access-date=requires|url=(help) - ^ Information, National Center for Biotechnology; Pike, U. S. National Library of Medicine 8600 Rockville; MD, Bethesda; Usa, 20894. "Autonomic Nervous System - National Library of Medicine". PubMed Health. Retrieved 2016-02-21.
{{cite web}}:|first4=has numeric name (help)CS1 maint: numeric names: authors list (link) - ^ a b c d e f g h i Mustafa HI, Fessel JP, Barwise J, Shannon JR, Raj SR, Diedrich A, et al. (January 2012). "Dysautonomia: perioperative implications". Anesthesiology. 116 (1): 205–15. doi:10.1097/ALN.0b013e31823db712. PMC 3296831. PMID 22143168.
- ^ Loganovsky, Konstantin (1999). "Vegetative-Vascular Dystonia and Osteoalgetic Syndrome or Chronic Fatigue Syndrome as a Characteristic After-Effect of Radioecological Disaster". Journal of Chronic Fatigue Syndrome. 7 (3): 3–16. doi:10.1300/J092v07n03_02.
{{cite journal}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Ivanova ES, Mukharliamov FI, Razumov AN, Uianaeva AI (2008). "[State-of-the-art corrective and diagnostic technologies in medical rehabilitation of patients with vegetative vascular dystonia]". Voprosy Kurortologii, Fizioterapii, I Lechebnoi Fizicheskoi Kultury (1): 4–7. PMID 18376477.
- ^ Malysheva OA, Shirinskiĭ VS (1998). "[Seasonal changes of secondary immunodeficiency in patients with vascular dystonia]". Klinicheskaia Meditsina. 76 (5): 34–6. PMID 9644934.
- ^ Lobzin VS, Poliakova LA, Shiman AG, Zavodnik AI (March 1989). "[Treatment of autonomic vascular dystonia by combined physiotherapy methods]". Vrachebnoe Delo (3): 22–3. PMID 2750110.
- ^ Solov'eva AD, Kolosova OA, Loseva MM, Mindlina GE, Ginzburg LI (1985). "[Thermography in healthy subjects and in the syndrome of vegetative-vascular dystonia]". Zhurnal Nevropatologii I Psikhiatrii Imeni S.S. Korsakova. 85 (6): 905–10. PMID 4024817.
- ^ Isaev DN, Efremov KD (1983). "[Psychogenic factors participating in the development of vegetovascular dystonia of the hypertensive type in children]". Zhurnal Nevropatologii I Psikhiatrii Imeni S.S. Korsakova. 83 (10): 1548–52. PMID 6659792.
- ^ "H2 Blockers. Reducing stomach acid with H2 Blockers. | Patient". Patient. Retrieved 2016-02-21.
- ^ "Diabetic Autonomic Neuropathy".
- ^ "Safety Alerts for Human Medical Products - Balloon angioplasty devices to treat autonomic dysfunction: FDA Safety Communication - FDA concern over experimental procedures". www.fda.gov. Retrieved 9 March 2017.
- ^ Vinik AI, Maser RE, Mitchell BD, Freeman R (May 2003). "Diabetic autonomic neuropathy". Diabetes Care. 26 (5): 1553–79. doi:10.2337/diacare.26.5.1553. PMID 12716821.
Further reading
- Brading, Alison (1999). The autonomic nervous system and its effectors. Oxford: Blackwell Science. ISBN 978-0632026241.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - Goldstein, David (2016). Principles of Autonomic Medicine (PDF) (free online version ed.). Bethesda, Maryland: National Institute of Neurological Disorders and Stroke, National Institutes of Health. ISBN 9780824704087.
- Jänig, Wilfrid (2008). Integrative action of the autonomic nervous system : neurobiology of homeostasis (Digitally printed version. ed.). Cambridge: Cambridge University Press. ISBN 978-0521067546.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - Lara A, Damasceno DD, Pires R, Gros R, Gomes ER, Gavioli M, et al. (April 2010). "Dysautonomia due to reduced cholinergic neurotransmission causes cardiac remodeling and heart failure". Molecular and Cellular Biology. 30 (7): 1746–56. doi:10.1128/MCB.00996-09. PMC 2838086. PMID 20123977.
- Schiffer, Randolph B.; Rao, Stephen M.; Fogel, Barry S. (2003-01-01). Neuropsychiatry. Lippincott Williams & Wilkins. ISBN 9780781726559.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help)
