Lacritin
Lacritin is a 12.3 kDa glycoprotein encoded in humans by the LACRT gene.[3][4] Lacritin's discovery emerged from a screen for factors that stimulate tear protein secretion.[4][5] Lacritin is a secreted protein found in tears and saliva. Lacritin also promotes tear secretion,[4][6] the proliferation[4] and survival of epithelial cells,[7] and corneal wound healing[8] Lacritin is thus a multifunctional prosecretory mitogen with cell survival activity. Natural or bacterial cleavage of lacritin releases a C-terminal fragment that is bactericidal.[9]
Most lacritin is produced by the lacrimal gland,[4] including the accessory lacrimal gland of Wolfring.[10] Some lacritin is produced by the meibomian gland, and by epithelial cells of the conjunctiva and cornea.[11] Together these epithelia comprise much of the lacrimal functional unit (LFU). Dry eye is the most common disease of the LFU. A growing number of studies suggest that lacritin may be differentially downregulated in dry eye,[12] including contact lens-related dry eye.[13] Topical lacritin promotes tearing in rabbit preclinical studies.[14] In the Aire knockout mouse model of dry eye (considered similar to human Sjogren's syndrome), topical lacritin restores pilocarpine-induced tearing, largely eliminates lissamine green staining and reduces the size of inflammatory foci in the lacrimal gland.[15]
Lacritin cell targeting is dependent on the cell surface heparan sulfate proteoglycan syndecan-1 (SDC1).[16][17] Binding utilizes an enzyme-regulated 'off-on' switch in which active epithelial heparanase (HPSE) cleaves off heparan sulfate to expose a binding site in the N-terminal region of syndecan-1's core protein.[16] A G-protein-coupled receptor (GPCR) then appears to be ligated.[18] Targeted cells signal to NFAT and mTOR[18] if conditions are suitable for proliferation, or to AKT and FOXO3 under conditions of stress.[7]
Structure
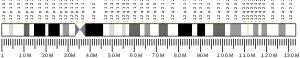
[edit]Lacritin consists of 119 amino acids after cleavage of the N-terminal signal peptide and displays several predicted alpha helices, mostly in the C-terminal half. Of these, the two C-terminal ones have been confirmed by circular dichroism.[18] The most C-terminal alpha helix is amphipathic with hydrophobic and hydrophilic residues on opposite faces. The hydrophobic face is an important syndecan-1 binding element.[17] PONDR (Predictor of Naturally Disordered Regions)[19] predicts that the C-terminal and N-terminal halves are respectively 'ordered' and 'disordered'. 11 - 12 predicted O-glycosylation sites populate the N-terminal half. The C-terminal amphipathic alpha helix is also the site of lacritin's only N-glycosylation site. In 'climatic droplet keratopathy' this site is not glycosylated.[20] Lacritin recombinantly generated in E. coli (no glycosylation) and lacritin in tears (glycosylated) differ in size with respective mobilities of ~18 and ~25 kDa by SDS-PAGE. With a predicted protein core molecular weight of 12.3 kDa, it is possible that mobility is partially retarded by lacritin's amphipathic alpha helices. Predicted pI of lacritin's core protein is 5.[12]
Lacritin is subject to crosslinking by tissue transglutaminase, thereby giving rise to lacritin multimers including dimers and trimers.[21] Crosslinking is initiated within 1 min in vitro, requiring as little as 0.1 nM lacritin.[21] The ~0.6 micro molar level of tissue transglutaminase estimated in human tears is sufficient to promote crosslinking.[21] Crosslinking involves the donors lysine 82 and 85 and the acceptor glutamine 106.[21] Glutamine 106 resides within the amphipathic alpha helix near the C-terminus responsible for binding the N-terminus of syndecan-1.[17] Accordingly, crosslinked lacritin binds syndecan-1 poorly[21] and is inactive.
Several lacritin splice variants have been detected in Aceview,[22] from NEIBank EST data.[23] Lacritin-b (11.1 kDa; pI 5.3) lacks the sequence SIVEKSILTE. Lacritin-c (10.7 kDa; pI 4.6) displays a novel C-terminus that should be incapable of binding syndecan-1, and lacks cell survival activity.[7]
Splice variants are proteoforms. Proteoforms include proteolytically processed forms of lacritin. Top down mass spec sequencing revealed that human tears contain five N- and forty-two different C-terminal lacritin-a proteoforms.[24] Some approximate the bioactive lacritin synthetic peptides 'N-104',[9] 'N-94' and 'N-94/C-6'[25] from lacritin's C-terminus. Protease inhibitor studies suggest that processing of lacritin into C-terminal proteoforms requires a variety of tear proteases including cathepsin B, calpain, alanyl amino peptidase, arginyl aminopeptidase, MMP9, MMP10, cathepsin G, plasma kallikrein, plasmin, thrombin and trypsin.[25] C-terminal proteoforms, like intact lacritin, are selectively deficient in dry eye tears.[25]
Cell targeting
[edit]Lacritin targets a restricted group of epithelial cells (including human corneal epithelia), and not fibroblastic, glioma, or lymphoblastic cells.[18] Cell surface proteoglycan syndecan-1 is partly responsible.[16][17]
Biotinylated cell surface proteins from a lacritin-responsive cell were incubated with lacritin under conditions of physiological salt. Those that bound lacritin were sequenced by mass spectrometry. Few bound. The most prominent was syndecan-1 (SDC1). In confirmatory pull-down assays, binding was not shared with family members syndecan-2 or syndecan-4,[16] indicating that the protein core (and not the negatively charged heparan sulfate side-chains) was the main site of binding. Further analysis narrowed the site to syndecan-1's N-terminal 51 amino acids,[16] and subsequently to the N-terminal sequence GAGAL that is conserved in syndecan-1's from different species.[17] GAGAL promotes the alpha helicity of lacritin's C-terminal amphipathic alpha helix and likely binds to the hydrophobic face.[17] Syndecan-1 binds many growth factors through its long heparan sulfate side-chains. Yet, long heparan sulfate chains interfere with lacritin binding. Since syndecans are always decorated with heparan sulfate, this means that heparanase must be available to partially or completely cleave off heparan sulfate, allowing lacritin to bind. Indeed, no binding was detected from cells lacking heparanase after siRNA depletion.[16] Binding was restored by spiking in exogenous heparanase or heparitinase.[16] Thus, heparanase regulates lacritin function as an 'on-switch'. Exposed 3-O sulfated groups on heparanase-cleaved heparan sulfate[17] (that likely interacts with the cationic face of lacritin's C-terminal amphipathic alpha helix), and an N-terminal chondroitin sulfate chain (likely also binds to the cationic face) appear to contribute to binding.[17] Point mutagenesis of lacritin has narrowed the ligation site.[17] This novel heparanase mechanism appears at first glance to be poor for ocular health since heparanase release from invading lymphocytes in the corneal stroma is inflammatory. Yet heparanase is a normal secretory product of the corneal epithelium.[26]
Lacritin-dependent mitogenesis is inhibitable by pertussis toxin,.[18] The implication is that another key element of lacritin targeting specificity is a G-protein-coupled receptor that would presumably form a cell surface targeting complex with SDC1. Involvement of a G-protein coupled receptor would explain the rapidity of lacritin signaling.
Function
[edit]Lacritin is a glycoprotein of the human tear film, and to a lesser extent of saliva, lung lavage[27] and plasma.[28] It is mainly produced by the lacrimal gland.[4] Some lacritin also is produced by the meibomian gland, and also by epithelial cells of the conjunctiva and cornea.[11] The lacritin gene (LACRT) is one of the most transcriptionally regulated genes in the human eye.[29] Functional studies suggest a role in epithelial renewal of some non-germative epithelia. By flowing downstream through ducts, it may generate a 'proliferative field'.[18] Lacritin also promotes secretion[4] (including that of lipocalin-1 and lactoferrin[6]), cell survival and regeneration of the corneal epithelium after wounding.[8] Three times daily topical treatment with C-terminal lacritin synthetic peptide 'Lacripep' (also known as 'N-94/C-6') at a 4 μM concentration regenerated corneal nerves and the ocular surface epithelium in the mouse Aire-/- dry eye model.[30] This raises the possibility that lacritin may have clinical applications in the treatment of dry eye, the most common eye disease. It also may be beneficial in promoting healing after LASIK or PRK surgery. Recent studies suggest that lacritin monomer is differentially down regulated in not only in dry eye,[31] but also in blepharitis.[32]
Lacritin is an LFU prosecretory mitogen and survival factor with a biphasic dose response that is optimal at 1 - 10 nM for human recombinant lacritin on human cells.[18] Higher human lacritin concentrations are optimal on rat or mouse cells[4] or on rabbit eyes.[14] In a recent phase I/II clinical trial, a 22 μM topical dose of 'Lacripep' applied three times daily was effective at two weeks in primary Sjogren's Syndrome patients with an eye dryness score greater than 60, a score indicative of moderate to severe dry eye. Both corneal fluorescein staining and the symptom of burning/stinging were reduced. In keeping with a biphasic dose response, the 44 μM dose was largely ineffective.[33] A biphasic dose response has a bell-shaped curve, with doses lower or higher than the dose optimum less effective. Other mitogens share this property.[18] However, in secretion assays using monkey lacritin on monkey lacrimal acinar cells, the dose response appears to be sigmoidal with increasing lipocalin or lactoferrin secretion through a narrow 0.1, 0.3 and 1 μM dose range.[6] Lacritin flows downstream from the lacrimal gland through ducts onto the eye.
Artificial depletion of lacritin from normal human tears revealed that tears lacking lacritin are unable to promote the survival of ocular surface cells stressed with inflammatory cytokines.[7] Human dry eye tears also lack this activity. However, dry eye tears supplemented with lacritin are fully protective.[7] Similarly, tears artificially depleted of lacritin are deficient in bactericidal activity.[9] The antibody used to deplete lacritin also depletes C-terminal proteoforms.[25] These observations suggest that among all tear proteins, lacritin may be the master protector.
Dry eye tears are subject to premature collapse, as are normal human tears artificially depleted of C-terminal proteoforms.[25] In both cases, stability is largely restored by spiking in synthetic lacritin peptides N-94 or N-94/C-6 as proxy C-terminal proteoforms.[25] Each peptide inserts rapidly into (O-acyl)-omega-hydroxy fatty acid (OAHFA)[25] thought to reside at the aqueous lipid boundary in tears. OAHFA is the only class of tear lipids apparently downregulated in dry eye.[34]
Signaling
[edit]Lacritin mitogenic, survival and secretion signaling have been studied.
Lacritin mitogenic signaling[18] follows two pathways:
Rapid dephosphorylation of PKCα causes it to transiently move from the cytoplasm to the area of the Golgi apparatus and peripheral nucleus. Here, it forms a complex with PKCα and PLCγ2 from which downstream mTOR and NFAT signaling is initiated.[18] The upstream Gαi or Gαo signaling suggests the involvement of a G-protein-coupled receptor (GPCR). A candidate GPCR is under study. Syndecan-1 likely serves as a co-receptor. Binding lacritin may improve its GPCR affinity.
Lacritin survival signaling is observed when cells are stressed.[7] Lacritin promotes survival and homeostasis by transiently stimulating autophagy.[7] The mechanism appears to involve lacritin stimulated acetylation of the transcription factor FOXO3. Acetylated FOXO3 serves as a ligand for the autophagic mediator ATG101. Lacritin also promotes coupling of FOXO1 (that becomes acetylated with stress) with autophagic mediator ATG7. In the absence of lacritin, no coupling is observed.[7] Thus acetylation alone is likely insufficient for FOXO1-ATG7 ligation, unlike an initial claim.[35] Lacritin also restores oxidative phosphorylation and other metabolic events to rescue cells from stress.[7]
Lacritin stimulated secretion of tear proteins lipocalin and lactoferrin from monkey lacrimal acinar cells does not appear to be mediated by Ca2+, unlike the agonist carbachol.[6] When monkey lacrimal acinar cells are stressed with inflammatory cytokines (as occurs in dry eye), carbachol loses its capacity to promote the secretion of lipocalin. However, lacritin stimulates lipocalin secretion even in the presence of stress.[6]
Distribution
[edit]Species
[edit]Genomic sequencing assembled by Ensembl reveals the existence of putative lacritin orthologues in other species.[36] Comparative genomic alignment suggests that horse lacritin is most similar to human lacritin among all non-primate sequences examined.[31] Moreover, it is detectable in horse tears by immunoblotting or by ELISA.[37] Antibodies directed to the C-, but not N-, terminus of human lacritin are most effective[37] - in keeping with the predicted conservation of the C-terminal amphipathic alpha helix[37] necessary for cell targeting.[16]
Tissue
[edit]Tissue distribution has been examined in humans and monkeys. Lacritin is most highly expressed in the lacrimal gland, including the accessory lacrimal gland of Wolfring.[10] Expression is moderate in salivary glands and slight in mammary (cancer but not or rarely normal), and thyroid glands.[4][29][38][39] The salivary gland expression appears to be attributable to a discrete group of unidentified ductal-like cells.[4] Some lacritin was reported in lung bronchoalveolar lavage[40] and plasma.[28] In lacrimal gland, polarized lacrimal acinar cells appear to be the most prolific lacritin producers, as evidenced by strong staining of secretory granules[4] in keeping with lacritin release after carbachol stimulation.[11] Carbachol-dependent release involves PKC and calcium signaling.[41] Some lacritin is produced by the meibomian gland, and also by epithelial cells of the conjunctiva and cornea[11] that together with lacrimal gland comprise much of the lacrimal functional unit (LFU). Viewed collectively, the LFU is the primary source of lacritin in the body, and the eye the main target.[4]
Disease
[edit]Dry eye is the most common eye disease, affecting 5 - 6% of the population. Prevalence rises to 6 - 9.8% in postmenopausal women,[42] and as high as 34% in the elderly.[43] Tears lubricate the lid and are important for the refraction of light. Tears also promote epithelial health. Only a small fraction of the estimated 1543 proteins[44] in tears are differentially deficient or upregulated in dry eye.[31] Lacritin monomer is differentially downregulated in mild to severe aqueous deficient dry eye,[45] and in contact lens-related dry eye.[13] In a larger trial, 95% of tears from patients with aqueous deficient dry eye were lacritin monomer deficient.[46] Two studies that did not differentiate monomer from multimer did note any change of lacritin in dry eye. Topical treatment of eyes of dry eye mice (Aire knockout mouse model of dry eye) restored tearing, and suppressed both corneal staining and the size of inflammatory foci in lacrimal glands.[15] Lacritin monomer deficiency in tears of patients with blepharitis was also reported.[32] Blepharitis is an inflammation of the eyelid often associated with dry eye.[12] In climatic droplet keratopathy, N119 appears to be un-glycosylated. Also a normal breast cancer localization reported by some has not been replicated in Unigene (the 'mammary gland' hit is for breast cancer) and gene array studies,[39] but some breast cancers appear to display elevated expression[39] or LACRT gene amplification.[47] iTRAQ analysis of tears from diabetics at different stages of disease detected relatively more lacritin, lysozyme, lipophilin A, lipocalin 1, immunoglobulin lambda chain and lactotransferrin in tears of patients with diabetic retinopathy. The analysis did not distinguish lacritin monomer from polymer, and proposed the application of all as biomarkers.[48] Tear lacritin monomer is barely detectable in the initial stage of infection by Fusarium solani in fungal keratitis.[49] Also down regulated are tear lipocalin-1 and cystatin S.[49] Fungal keratitis accounts for half of all corneal ulcers in Africa and India[50][51][52] - the primary source of blindness in these countries.[53] Phase II clinical trial of 'Lacripep™ in Subjects With Dry Eye Associated With Primary Sjögren's Syndrome' (NCT03226444)[54] is complete. Lacripep™ is lacritin synthetic peptide 'N-94/C-6'.
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000135413 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Entrez Gene: LACRT lacritin".
- ^ a b c d e f g h i j k l Sanghi S, Kumar R, Lumsden A, Dickinson D, Klepeis V, Trinkaus-Randall V, Frierson HF, Laurie GW (June 2001). "cDNA and genomic cloning of lacritin, a novel secretion enhancing factor from the human lacrimal gland". Journal of Molecular Biology. 310 (1): 127–39. doi:10.1006/jmbi.2001.4748. PMID 11419941.
- ^ "Lacritin and Dry Eye". Facebook.
- ^ a b c d e Fujii A, Morimoto-Tochigi A, Walkup RD, Shearer TR, Azuma M (April 2013). "Lacritin-induced secretion of tear proteins from cultured monkey lacrimal acinar cells". Invest Ophthalmol Vis Sci. 54 (4): 2533–40. doi:10.1167/iovs.12-10394. PMC 3626314. PMID 23482462.
- ^ a b c d e f g h i Wang N, Zimmerman K, Raab RW, McKown RL, Hutnik CM, Talla V, Tyler MF, Lee JK, Laurie GW (June 2013). "Lacritin Rescues Stressed Epithelia via Rapid Forkhead Box O3 (FOXO3)-associated Autophagy That Restores Metabolism". J Biol Chem. 288 (25): 18146–61. doi:10.1074/jbc.M112.436584. PMC 3689958. PMID 23640897.
- ^ a b Wang W, Despanie J, Shi P, Edman-Woolcott MC, Lin Y, Cui H, Heur JM, Fini ME, Hamm-Alvarez SF, MacKay JA (December 2014). "Lacritin-mediated regeneration of the corneal epithelia by protein polymer nanoparticles". J. Mater. Chem. B. 2 (46): 8131–8141. doi:10.1039/c4tb00979g. PMC 4270104. PMID 25530855.
- ^ a b c McKown RL, Coleman Frazier EV, Zadrozny KK, Deleault AM, Raab RW, Ryan DS, Sia RK, Lee JK, Laurie GW (Aug 2014). "A Cleavage-potentiated Fragment of Tear Lacritin Is Bactericidal". J Biol Chem. 289 (32): 22172–82. doi:10.1074/jbc.M114.570143. PMC 4139230. PMID 24942736.
- ^ a b Ubels JL, Gipson IK, Spurr-Michaud SJ, Tisdale AS, Van Dyken RE, Hatton MP (October 2012). "Gene expression in human accessory lacrimal glands of Wolfring". Invest Ophthalmol Vis Sci. 53 (25): 6738–47. doi:10.1167/iovs.12-10750. PMC 4113189. PMID 22956620.
- ^ a b c d Nakajima T, Walkup RD, Tochigi A, Shearer TR, Azuma M (November 2007). "Establishment of an appropriate animal model for lacritin studies: cloning and characterization of lacritin in monkey eyes". Experimental Eye Research. 85 (5): 651–8. doi:10.1016/j.exer.2007.07.019. PMID 17850790.
- ^ a b c McKown RL, Wang N, Raab RW, Karnati R, Zhang Y, Williams PB, Laurie GW (September 2008). "Lacritin and other new proteins of the lacrimal functional unit". Experimental Eye Research. 88 (5): 848–58. doi:10.1016/j.exer.2008.09.002. PMC 2712882. PMID 18840430.
- ^ a b Nichols JJ, Green-Church KB (December 2009). "Mass spectrometry-based proteomic analyses in contact lens-related dry eye". Cornea. 28 (10): 1109–17. doi:10.1097/ICO.0b013e3181a2ad81. PMID 19770725. S2CID 23889689.
- ^ a b Samudre S, Lattanzio FA, Lossen V, Hosseini A, Sheppard JD, McKown RL, Laurie GW, Williams PB (November 2010). "Lacritin, a Novel Human Tear Glycoprotein, Promotes Sustained Basal Tearing and is Well Tolerated". Invest Ophthalmol Vis Sci. 52 (9): 6265–70. doi:10.1167/iovs.10-6220. PMC 3176019. PMID 21087963.
- ^ a b Vijmasi T, Chen FY, Balasubbu S, Gallup M, McKown RL, Laurie GW, McNamara NA (July 2014). "Topical administration of lacritin is a novel therapy for aqueous-deficient dry eye disease". Invest Ophthalmol Vis Sci. 55 (8): 5401–9. doi:10.1167/iovs.14-13924. PMC 4148924. PMID 25034600.
- ^ a b c d e f g h Ma P, Beck SL, Raab RW, McKown RL, Coffman GL, Utani A, Chirico WJ, Rapraeger AC, Laurie GW (September 2006). "Heparanase deglycanation of syndecan-1 is required for binding of the epithelial-restricted prosecretory mitogen lacritin". The Journal of Cell Biology. 174 (7): 1097–106. doi:10.1083/jcb.200511134. PMC 1666580. PMID 16982797.
- ^ a b c d e f g h i Zhang Y, Wang N, Raab RW, McKown RL, Irwin JA, Kwon I, van Kuppevelt TH, Laurie GW (March 2013). "Targeting of heparanase-modified syndecan-1 by prosecretory mitogen lacritin requires conserved core GAGAL plus heparan and chondroitin sulfate as a novel hybrid binding site that enhances selectivity". The Journal of Biological Chemistry. 288 (17): 12090–101. doi:10.1074/jbc.M112.422717. PMC 3636894. PMID 23504321.
- ^ a b c d e f g h i j Wang J, Wang N, Xie J, Walton SC, McKown RL, Raab RW, Ma P, Beck SL, Coffman GL, Hussaini IM, Laurie GW (August 2006). "Restricted epithelial proliferation by lacritin via PKCalpha-dependent NFAT and mTOR pathways". The Journal of Cell Biology. 174 (5): 689–700. doi:10.1083/jcb.200605140. PMC 1761701. PMID 16923831.
- ^ "ENSG00000135413". In Silico Transcriptomics Online. Molecular Kinetics. 2008-04-29.
- ^ Zhou L, Beuerman R, Chew AP, Koh SK, Cafaro T, Urrets-Zavalia E, Urrets-Zavalia J, Li S, Serra H (February 2009). "Quantitative Analysis of N-linked Glycoproteins in Tear Fluid of Climatic Droplet Keratopathy by Glycopeptide Capture and iTRAQ". J Proteome Res. 8 (4): 1992–2003. doi:10.1021/pr800962q. PMID 19187007.
- ^ a b c d e Velez VF, Romano JA, McKown RL, Green K, Zhang L, Raab RW, Ryan DS, Hutnik CM, Frierson HF, Laurie GW (March 2013). "Tissue transglutaminase is a negative regulator of monomeric lacritin bioactivity". Invest Ophthalmol Vis Sci. 54 (17): 2123–32. doi:10.1167/iovs.12-11488. PMC 3621506. PMID 23425695.
- ^ "Homo sapiens gene LACRT, encoding lacritin". The AceView genes. National Center for Biotechnology Information (NCBI), U.S. National Library of Medicine.
- ^ Ozyildirim AM, Wistow GJ, Gao J, Wang J, Dickinson DP, Frierson HF, Laurie GW (2005). "The lacrimal gland transcriptome is an unusually rich source of rare and poorly characterized gene transcripts". Invest. Ophthalmol. Vis. Sci. 46 (5): 1572–80. CiteSeerX 10.1.1.123.3574. doi:10.1167/iovs.04-1380. PMID 15851553.
- ^ Azkargorta M, Soria J, Ojeda C, Guzmán F, Acera A, Iloro I, Suárez T, Elortza F (May 2015). "Human Basal Tear Peptidome Characterization by CID, HCD, and ETD Followed by in Silico and in Vitro Analyses for Antimicrobial Peptide Identification". J Proteome Res. 14 (6): 2649–2658. doi:10.1021/acs.jproteome.5b00179. PMC 2429281. PMID 2594603.
- ^ a b c d e f g Georgiev GA, Sharifian Gh M, Romano J, Dias Teixeira KL, Struble C, Ryan DS, Sia RK, Kitt JP, Harris JM, Hsu KL, Libby A, Odrich MG, Suárez T, McKown RL, Laurie GW. "Lacritin proteoforms prevent tear film collapse and maintain epithelial homeostasis". J Biol Chem. 296: 100070. doi:10.1074/jbc.RA120.015833. PMC 7948570. PMID 33187980.
- ^ Berk RS, Dong Z, Alousi S, Kosir MA, Wang Y, Vlodavsky I (April 2004). "Murine ocular heparanase expression before and during infection with Pseudomonas aeruginosa". Invest Ophthalmol Vis Sci. 45 (4): 1182–11876. doi:10.1167/iovs.03-0589. PMID 15037586.
- ^ "LACRT".
- ^ a b "PPD".
- ^ a b "LOC90070".
- ^ Efraim Y, Chen FY, Cheong KN, Gaylord EA, McNamara NA, Knox SM (August 2022). "A synthetic tear protein resolves dry eye through promoting corneal nerve regeneration". Cell Rep. 40 (9): 111307. doi:10.1016/j.celrep.2022.111307. PMC 9549932. PMID 36044852.
- ^ a b c Karnati R, Laurie DE, Laurie GW (June 2013). "Lacritin and the tear proteome as natural replacement therapy for dry eye". Exp Eye Res. 117: 39–52. doi:10.1016/j.exer.2013.05.020. PMC 3844047. PMID 23769845.
- ^ a b Koo BS, Lee DY, Ha HS, Kim JC, Kim CW (2005). "Comparative analysis of the tear protein expression in blepharitis patients using two-dimensional electrophoresis". Journal of Proteome Research. 4 (3): 719–24. doi:10.1021/pr0498133. PMID 15952718.
- ^ Tauber J, Laurie GW, Parsons EC, Odrich MG (August 2022). "Lacripep for the Treatment of Primary Sjögren's-Associated Ocular Surface Disease: Results of the First-In-Human Study". Cornea. 42 (7): 847–857. doi:10.1097/ICO.0000000000003091. PMC 9895125. PMID 35942530. S2CID 251443621.
- ^ Lam SM, Tong L, Yong SS, Li B, Chaurasia SS, Shui G, Wenk MR (Oct 2011). "Meibum lipid composition in Asians with dry eye disease". PLOS ONE. 6 (10): e24339. Bibcode:2011PLoSO...624339L. doi:10.1371/journal.pone.0024339. PMC 3197196. PMID 22043274.
- ^ Zhao Y, Yang J, Liao W, Liu X, Zhang H, Wang S, Wang D, Feng J, Yu L, Zhu WG (June 2010). "Cytosolic FoxO1 is essential for the induction of autophagy and tumour suppressor activity". Nat Cell Biol. 12 (7): 665–75. doi:10.1038/ncb2069. PMID 20543840. S2CID 12208376.
- ^ "Gene report for ENSG00000135413". Ensembl release 72: Homo sapiens. EMBL-EBI and the Sanger Centre.
- ^ a b c Laurie DE, Splan RK, Green K, Still KM, McKown RL, Laurie GW (Sep 2012). "Detection of prosecretory mitogen lacritin in nonprimate tears primarily as a C-terminal-like fragment". Invest Ophthalmol Vis Sci. 53 (10): 6130–6. doi:10.1167/iovs.11-8567. PMC 3441044. PMID 22871838.
- ^ "Expression Profile Viewer: Hs.307096". UniGene. National Center for Biotechnology Information (NCBI), United States National Institutes of Health.
- ^ a b c "LACRT ENSG00000135413". Insilico Transcriptomics Online. GeneSapiens. 2008-04-29.[permanent dead link]
- ^ "HuPA_00022".
- ^ Morimoto-Tochigi A, Walkup RD, Nakajima E, Shearer TR, Azuma M (September 2010). "Mechanism for carbachol-induced secretion of lacritin in cultured monkey lacrimal acinar cells". Invest Ophthalmol Vis Sci. 51 (9): 4395–406. doi:10.1167/iovs.09-4573. PMID 20375347.
- ^ Schaumberg DA, Sullivan DA, Buring JE, Dana MR (August 2003). "Prevalence of dry eye syndrome among US women". Am J Ophthalmol. 136 (2): 318–26. doi:10.1016/S0002-9394(03)00218-6. PMID 12888056.
- ^ Lin PY, Cheng CY, Hsu WM, Tsai SY, Lin MW, Liu JH, Chou P (May 2005). "Association between symptoms and signs of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study". Invest Ophthalmol Vis Sci. 46 (5): 1593–. doi:10.1167/iovs.04-0864. PMID 15851556.
- ^ Zhou L, Zhao SZ, Koh SK, Chen L, Vaz C, Tanavde V, Li XR, Beuerman RW (July 2012). "In-depth analysis of the human tear proteome". J Proteomics. 75 (13): 3877–85. doi:10.1016/j.jprot.2012.04.053. PMID 22634083.
- ^ Srinivasan S, Thangavelu M, Zhang L, Green KB, Nichols KK (July 2012). "iTRAQ quantitative proteomics in the analysis of tears in dry eye patients". Invest Ophthalmol Vis Sci. 53 (8): 5052–9. doi:10.1167/iovs.11-9022. PMC 3410666. PMID 22736608.
- ^ Aluru SV, Agarwal S, Srinivasan B, Iyer GK, Rajappa SM, Tatu U, Padmanabhan P, Subramanian N, Narayanasamy A (2012). "Lacrimal proline rich 4 (LPRR4) protein in the tear fluid is a potential biomarker of dry eye syndrome". PLOS ONE. 7 (12): e51979. Bibcode:2012PLoSO...751979A. doi:10.1371/journal.pone.0051979. PMC 3525644. PMID 23272196.
- ^ Porter D, Weremowicz S, Chin K, Seth P, Keshaviah A, Lahti-Domenici J, Bae YK, Monitto CL, Merlos-Suarez A, Chan J, Hulette CM, Richardson A, Morton CC, Marks J, Duyao M, Hruban R, Gabrielson E, Gelman R, Polyak K (2003). "A neural survival factor is a candidate oncogene in breast cancer". Proc. Natl. Acad. Sci. U.S.A. 100 (19): 10931–6. Bibcode:2003PNAS..10010931P. doi:10.1073/pnas.1932980100. PMC 196905. PMID 12953101.
- ^ Csősz É, Boross P, Csutak A, Berta A, Tóth F, Póliska S, Török Z, Tőzsér J (April 2012). "Quantitative analysis of proteins in the tear fluid of patients with diabetic retinopathy". J Proteomics. 75 (7): 2196–204. doi:10.1016/j.jprot.2012.01.019. PMID 22300579.
- ^ a b Ananthi S, Venkatesh Prajna N, Lalitha P, Valarnila M, Dharmalingam K (Jan 2013). "Pathogen induced changes in the protein profile of human tears from Fusarium keratitis patients". PLOS ONE. 8 (1): e53018. Bibcode:2013PLoSO...853018A. doi:10.1371/journal.pone.0053018. PMC 3540078. PMID 23308132.
- ^ Srinivasan M, Gonzales CA, George C, Cevallos V, Mascarenhas JM, Asokan B, Wilkins J, Smolin G, Whitcher JP (Nov 1997). "Epidemiology and aetiological diagnosis of corneal ulceration in Madurai, south India". Br J Ophthalmol. 81 (11): 965–71. doi:10.1136/bjo.81.11.965. PMC 1722056. PMID 9505820.
- ^ Poole TR, Hunter DL, Maliwa EM, Ramsay AR (Aug 2002). "Aetiology of microbial keratitis in northern Tanzania". Br J Ophthalmol. 86 (8): 941–2. doi:10.1136/bjo.86.8.941. PMC 1771226. PMID 12140229.
- ^ Hagan M, Wright E, Newman M, Dolin P, Johnson G (Nov 1995). "Causes of suppurative keratitis in Ghana". Br J Ophthalmol. 79 (11): 1024–8. doi:10.1136/bjo.79.11.1024. PMC 505322. PMID 8534648.
- ^ Whitcher JP, Srinivasan M (Aug 1997). "Corneal ulceration in the developing world--a silent epidemic". Br J Ophthalmol. 81 (8): 622–3. doi:10.1136/bjo.81.8.622. PMC 1722289. PMID 9349145.
- ^ "Lacripep™ in Subjects With Dry Eye Associated With Primary Sjögren's Syndrome2".
Further reading
[edit]- Green-Church KB, Nichols JJ (2008). "Mass spectrometry-based proteomic analyses of contact lens deposition". Molecular Vision. 14: 291–7. PMC 2254969. PMID 18334948.
- Tsai PS, Evans JE, Green KM, Sullivan RM, Schaumberg DA, Richards SM, Dana MR, Sullivan DA (March 2006). "Proteomic analysis of human meibomian gland secretions". The British Journal of Ophthalmology. 90 (3): 372–7. doi:10.1136/bjo.2005.080846. PMC 1856970. PMID 16488965.
- Zhou L, Beuerman RW, Foo Y, Liu S, Ang LP, Tan DT (June 2006). "Characterisation of human tear proteins using high-resolution mass spectrometry" (PDF). Annals of the Academy of Medicine, Singapore. 35 (6): 400–7. doi:10.47102/annals-acadmedsg.V35N6p400. PMID 16865190. S2CID 33555528.
- Kumar R, Huebner A, Laurie GW (2002). "Genetic Separation of the Human Lacritin Gene ("LACRT") and Triple A (Allgrove) Syndrome on 12Q13". Lacrimal Gland, Tear Film, and Dry Eye Syndromes 3. Advances in Experimental Medicine and Biology. Vol. 506. pp. 167–74. doi:10.1007/978-1-4615-0717-8_22. ISBN 978-1-4613-5208-2. PMID 12613904.
- Weigelt B, Bosma AJ, van 't Veer LJ (2004). "Expression of a novel lacrimal gland gene lacritin in human breast tissues". J. Cancer Res. Clin. Oncol. 129 (12): 735–6. doi:10.1007/s00432-003-0514-y. PMID 14574570. S2CID 24990940.
- Koo BS, Lee DY, Ha HS, Kim JC, Kim CW (2005). "Comparative analysis of the tear protein expression in blepharitis patients using two-dimensional electrophoresis". J. Proteome Res. 4 (3): 719–24. doi:10.1021/pr0498133. PMID 15952718.
- Tsai PS, Evans JE, Green KM, Sullivan RM, Schaumberg DA, Richards SM, Dana MR, Sullivan DA (2006). "Proteomic analysis of human meibomian gland secretions". The British Journal of Ophthalmology. 90 (3): 372–7. doi:10.1136/bjo.2005.080846. PMC 1856970. PMID 16488965.
- Ramachandran P, Boontheung P, Xie Y, Sondej M, Wong DT, Loo JA (2006). "Identification of N-linked glycoproteins in human saliva by glycoprotein capture and mass spectrometry". J. Proteome Res. 5 (6): 1493–503. doi:10.1021/pr050492k. PMID 16740002.
- Zhou L, Beuerman RW, Foo Y, Liu S, Ang LP, Tan DT (2007). "Characterisation of human tear proteins using high-resolution mass spectrometry". Ann. Acad. Med. Singap. 35 (6): 400–7. doi:10.47102/annals-acadmedsg.V35N6p400. PMID 16865190. S2CID 33555528.
External links
[edit]- LACRT protein, human at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- "LACRT". Wikigenes.
- "Lacritin". University of Virginia.
- "Ducts Out of Water". James Madison University.