Medial palpebral ligament
| Medial palpebral ligament | |
|---|---|
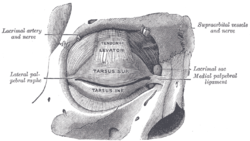 The tarsi and their ligaments. Right eye; front view. | |
| Details | |
| Origin | frontal process of the maxilla, lacrimal bone |
| Insertion | tarsus of the upper and lower eyelids |
| Artery | medial palpebral artery |
| Identifiers | |
| Latin | Ligamentum palpebrale mediale, tendo oculi |
| TA98 | A15.2.07.041 |
| TA2 | 6832 |
| FMA | 323068 |
| Anatomical terminology | |
The medial palpebral ligament (medial canthal tendon) is a ligament of the face. It attaches to the frontal process of the maxilla, the lacrimal groove, and the tarsus of each eyelid. It has a superficial (anterior) and a deep (posterior) layer, with many surrounding attachments. It connects the medial canthus of each eyelid to the medial part of the orbit. It is a useful point of fixation during eyelid reconstructive surgery.
Structure
The anterior attachment of the medial palpebral ligament is to the frontal process of the maxilla in front of the lacrimal groove (near the nasal bone and the frontal bone),[1] and its posterior attachment is the lacrimal bone. Crossing the lacrimal sac, it divides into two parts, upper and lower, each attached to the medial end of the corresponding tarsus of each eyelid.[2]
As the ligament crosses the lacrimal sac, a strong aponeurotic lamina is given off from its posterior surface; this expands over the sac, and is attached to the posterior lacrimal crest.
The medial palpebral ligament consists of a superficial (anterior) and a deep (posterior) layer.[2][3] The superficial layer has a length of around 9.6 mm, a width of around 2.4 mm, and a thickness of around 4.5 mm.[2] The deep layer has a length of around 3.7, a width of around 2.9, and a thickness of around 0.3 mm.[2] Together, these have a strength of around 17 newtons, with most of this strength from the superficial layer.[2]
Relations
The superior branch of the medial palpebral artery runs directly behind the medial palpebral ligament.[4] Branches of the facial nerve, particularly the buccal branches, pass upwards over the medial palpebral ligament to reach the nose.[5]
Function
The medial palpebral ligament connects the medial canthus of each eyelid to the medial part of the orbit.[1]
Clinical significance
The medial palpebral ligament can be used as a point of fixation during eyelid reconstructive surgery, allowing for normal blinking.[6][7]
History
The medial palpebral ligament has also been known as the medial canthal tendon. Some consider it to be a tendon of the lacrimal part of the orbicularis oculi muscle.[3]
See also
References
![]() This article incorporates text in the public domain from page 381 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 381 of the 20th edition of Gray's Anatomy (1918)
- ^ a b Shinohara, Harumichi; Kominami, Rieko; Yasutaka, Satoru; Taniguchi, Yutaka (2001). "The Anatomy of the Lacrimal Portion of the Orbicularis Oculi Muscle (Tensor Tarsi or Horner's Muscle)". Okajimas Folia Anatomica Japonica. 77 (6): 225–232. doi:10.2535/ofaj1936.77.6_225.
- ^ a b c d e Hwang, Kun; Huan, Fan; Nam, Yong Seok; Han, Seung Ho; Kim, Dae Joong (November 2013). "Location and Tension of the Medial Palpebral Ligament". Journal of Craniofacial Surgery. 24 (6): 2119–2123. doi:10.1097/SCS.0b013e31827c7c3e. ISSN 1049-2275.
- ^ a b Ritleng, P.; Bourgeon, A.; Richelme, H. (1983-03-01). "New concepts of the anatomy of the lacrimal apparatus". Anatomia Clinica. 5 (1): 29–34. doi:10.1007/BF01798870. ISSN 1279-8517.
- ^ Erdogmus, Senem; Govsa, Figen (2007-03-01). "The arterial anatomy of the eyelid: importance for reconstructive and aesthetic surgery". Journal of Plastic, Reconstructive & Aesthetic Surgery. 60 (3): 241–245. doi:10.1016/j.bjps.2006.01.056. ISSN 1748-6815.
- ^ Nemoto, Yuji; Sekino, Yoshihisa; Kaneko, Hiroyuki (2001-09-01). "Facial Nerve Anatomy in Eyelids and Periorbit". Japanese Journal of Ophthalmology. 45 (5): 445–452. doi:10.1016/S0021-5155(01)00381-1. ISSN 0021-5155 – via ScienceDirect.
- ^ Ueda, K.; Oba, S.; Okada, M.; Hara, M.; Zen, N. (2007-03-01). "Eyelid reconstruction with a composite radial forearm palmaris longus tendon flap". Journal of Plastic, Reconstructive & Aesthetic Surgery. 60 (3): 256–259. doi:10.1016/j.bjps.2006.03.058. ISSN 1748-6815.
- ^ Srivastava, Kuldeep Kumar; Sundaresh, Kannan; Vijayalakshmi, Perumalsamy (2004-08-01). "A new surgical technique for ocular fixation in congenital third nerve palsy". Journal of American Association for Pediatric Ophthalmology and Strabismus. 8 (4): 371–377. doi:10.1016/j.jaapos.2004.01.015. ISSN 1091-8531.
