Variant angina
| Variant angina | |
|---|---|
| Specialty | Cardiology |
Prinzmetal's or Prinzmetal angina (/ˈprɪntsmɛtəl/, sounds like "prints metal") (also known as variant angina, vasospastic angina (VSA), angina inversa, or coronary vessel spasm) is a syndrome typically consisting of angina (cardiac chest pain) at rest that occurs in cycles. It is caused by vasospasm, a narrowing of the coronary arteries caused by contraction of the smooth muscle tissue in the vessel walls rather than directly by atherosclerosis (buildup of fatty plaque and hardening of the arteries).
For a portion of patients Prinzmetal's angina may be a manifestation of vasospastic disorder and is associated with migraine, Raynaud's phenomenon or aspirin-induced asthma.[1]
Signs and symptoms
In contrast to patient with unstable angina secondary to coronary atherosclerosis, patients with variant angina are generally younger and have fewer coronary risk factors (except smoking). Episode of chest pain usually does not progress from a period of chronic stable angina. Cardiac examination is usually normal in the absence of ischemia.[1]
Symptoms typically occur at rest, rather than on exertion (thus attacks usually occur in early morning hours).[2] Two-thirds of patients have concurrent atherosclerosis of a major coronary artery, but this is often mild or not in proportion to the degree of symptoms.
Prinzmetal's should be suspected by a cardiologist when the pain occurs at rest and/or in clusters, and in the absence of a positive treadmill stress test, as Prinzmetal's is exercise tolerant and can generally only be diagnosed after other forms of cardiac disease have been ruled out.
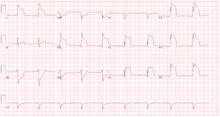
It is associated with specific ECG changes (elevation rather than depression of the ST segment) together with small elevation of cardiac enzymes (especially with long attacks). However, in order to be diagnosed, these ECG changes can only be tracked when the electrocardiogram occurs while the patient is experiencing an attack. Therefore, many experts recommend provocative testing during electrocardiogram testing to attempt to induce an attack when Prinzmetal's is suspected.
Mechanism
The mechanism that causes such intense vasospasm, as to cause a clinically significant narrowing of the coronary arteries is so far unknown, but there are three relevant hypotheses:
- Enhanced contractility of coronary vascular smooth muscle due to reduced nitric oxide bioavailability caused by a defect in the endothelial nitric oxide synthetase enzyme which leads to endothelial function abnormalities.[3][4]
- Acetylcholine is normally released by the parasympathetic nervous system (PSNS) at rest, and causes dilation of the coronary arteries.[5] While acetylcholine induces vasoconstriction of vascular smooth muscle cells through a direct mechanism, acetylcholine also stimulates endothelial cells to produce nitric oxide (NO). NO then diffuses out of the endothelial cells, stimulating relaxation of the nearby smooth muscle cells. In healthy arterial walls, the overall indirect relaxation induced by acetylcholine (via nitric oxide) is of greater effect than any contraction that is induced.
- When the endothelium is dysfunctional, stimulation with acetylcholine will fail to produce, or produce very little, nitric oxide. Thus, acetylcholine released by the PSNS at rest will simply cause contraction of the vascular smooth muscle.
- Thromboxane A2, a vasoconstrictor released by platelets to aid in clot formation, may also play a role in Prinzmetal's angina. Lipoprotein(a) interferes with fibrinolysis by competing with plasminogen. The impaired fibrinolysis triggers thrombus formation, which also results in coronary vasospasm in variant angina.[6][7]
- Increased alpha-adrenergic receptor activity on epicardial coronary arteries leads to coronary vasospasm.[8]
Apart from the hypotheses mentioned above; hypercontractility of vascular smooth muscle is also thought to be associated with vasoconstrictor mitogens and serotonin.[1]
Diagnosis
Although Prinzmetal's angina has been documented in between 2% to 10% of angina patients, it can be overlooked by cardiologists who stop testing protocol after ruling out typical angina. Rarely, an ECG can capture diffuse ST elevations.
Patients who develop cardiac chest pain are generally treated empirically as an "acute coronary syndrome", and are generally tested for cardiac enzymes such as creatine kinase isoenzymes or troponin I or T. These may or may not show a degree of positivity, as coronary spasm too can cause myocardial damage or may leave the arteries undamaged. Echocardiography or thallium scintigraphy is often performed.
The gold standard is coronary angiography with injection of provocative agents into the coronary artery. Rarely, an active spasm can be documented angiographically (e.g. if the patient receives an angiogram with intent of performing a primary coronary intervention with angioplasty). Depending on the local protocol, provocation testing may involve substances such as ergonovine, methylergonovine or acetylcholine and hyperventilation. Exaggerated spasm is diagnostic of Prinzmetal angina.
Treatment
Prinzmetal's angina typically responds to nitrates and calcium channel blockers.[9]
Use of a beta blocker such as propranolol is contraindicated in Prinzmetal's angina.[10] Prazosin has also been found to be of value in some patients.[1] Coronary revascularization is only useful when the patient shows concomitant coronary atherosclerosis on coronary angiogram.
Eponym
It was described as "A variant form of angina pectoris" in 1959 by the American cardiologist Myron Prinzmetal (1908–1987).[6] However, it had been described twice in the 1930s by other authors.[7][11]
It was first referred to as cardiac syndrome X (CSX) by Kemp in 1973, to describe patients with exercise-induced angina and normal coronary angiograms.[12]
See also
References
- ^ a b c d Harrison's Cardiovascular Medicine 2/E (2 ed.). New York: McGraw-Hill Education / Medical. 2013-08-02. ISBN 9780071814980.
- ^ "Prinzmetal's Angina, Variant Angina and Angina Inversa". American Heart Association. Retrieved 2015-06-20.
- ^ Yoo, Sang-Yong; Kim, Jang-Young (2009). "Recent Insights into the Mechanisms of Vasospastic Angina". Korean Circulation Journal. 39 (12): 505–11. doi:10.4070/kcj.2009.39.12.505. PMC 2801457. PMID 20049135.
- ^ Egashira, Kensuke; Katsuda, Yousuke; Mohri, Masahiro; Kuga, Takeshi; Tagawa, Tatuya; Shimokawa, Hiroaki; Takeshita, Akira (1996). "Basal release of endothelium-derived nitric oxide at site of spasm in patients with variant angina". Journal of the American College of Cardiology. 27 (6): 1444–9. doi:10.1016/0735-1097(96)00021-6. PMID 8626956.
- ^ Sun, Hongtao; Mohri, Masahiro; Shimokawa, Hiroaki; Usui, Makoto; Urakami, Lemmy; Takeshita, Akira (28 February 2002). "Coronary microvascular spasm causes myocardial ischemia in patients with vasospastic angina". Journal of the American College of Cardiology. 39 (5): 847–851. doi:10.1016/S0735-1097(02)01690-X. PMID 11869851.
- ^ a b Prinzmetal, Myron; Kennamer, Rexford; Merliss, Reuben; Wada, Takashi; Bor, Naci (1959). "Angina pectoris I. A variant form of angina pectoris". The American Journal of Medicine. 27 (3): 375–88. doi:10.1016/0002-9343(59)90003-8. PMID 14434946.
- ^ a b Parkinson, John; Bedford, D. Evan (1931). "Electrocardiographic Changes During Brief Attacks of Angina Pectoris". The Lancet. 217 (5601): 15–9. doi:10.1016/S0140-6736(00)40634-3.
- ^ "Prinzmetal's variant form of angina as a manifestation of alpha-adrenergic receptor-mediated coronary artery spasm: Documentation by coronary arteriography". American Heart Journal. 91(2): 148–155. February 1976. doi:10.1016/S0002-8703(76)80568-6.
{{cite journal}}: Unknown parameter|authors=ignored (help) - ^ American Heart Association http://www.americanheart.org/presenter.jhtml?identifier=4496 Archived 2010-06-20 at the Wayback Machine "Angina Pectoris Treatments"
- ^ British National Formulary, Vol 58, 2009, pg 88.
- ^ Brown, G.R.; Holman, Delavan V. (1933). "Electrocardiographic study during a paroxysm of angina pectoris". American Heart Journal. 9 (2): 259–64. doi:10.1016/S0002-8703(33)90720-6.
- ^ Kemp HG, Jr; Vokonas, PS; Cohn, PF; Gorlin, R (June 1973). "The anginal syndrome associated with normal coronary arteriograms. Report of a six year experience". The American Journal of Medicine. 54 (6): 735–42. doi:10.1016/0002-9343(73)90060-0. PMID 4196179.
External links
- Prinzmetal's angina at Who Named It?
- Coronary artery spasm at the Heart Foundation
- Crea, F; Lanza, GA. "Vasospastic Angina". European Society of Cardiology.
- www.prinzmetal.dk A site about Prinzmetal variant angina and cardiac syndrome x
- APAA - American Prinzmetal's Angina Association A site that gathers and shows both information for the public and also technical information for medical practitioners.
