Shigella
| Shigella | |
|---|---|
| |
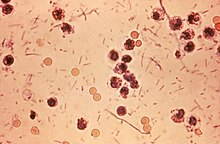
| Photomicrograph of Shigella sp. in a stool specimen | |
| Scientific classification | |
| Kingdom: | |
| Phylum: | |
| Class: | |
| Order: | |
| Family: | |
| Genus: | Shigella Castellani & Chalmers 1919
|
| Species | |
Shigella (/ʃɪˈɡɛlə/) is a genus of Gram-negative, facultative anaerobic, nonspore-forming, nonmotile, rod-shaped bacteria closely related to Salmonella. The genus is named after Kiyoshi Shiga, who first discovered it in 1897.[1]
The causative agent of human shigellosis, Shigella causes disease in primates, but not in other mammals.[2] It is only naturally found in humans and gorillas.[3][4] During infection, it typically causes dysentery.[5]
Shigella is one of the leading bacterial causes of diarrhea worldwide, causing an estimated 80-165 million cases.[6] The number of deaths it causes each year is estimated at between 74,000 and 600,000 deaths.[6][7] It is in the top four pathogens that cause moderate-to-severe diarrhea in African and South Asian children.[8]
Classification
Shigella species are classified by four serogroups:
- Serogroup A: S. dysenteriae (15 serotypes)[9]
- Serogroup B: S. flexneri (six serotypes)
- Serogroup C: S. boydii (19 serotypes)[10]
- Serogroup D: S. sonnei (one serotype)
Groups A–C are physiologically similar; S. sonnei (group D) can be differentiated on the basis of biochemical metabolism assays.[11] Three Shigella groups are the major disease-causing species: S. flexneri is the most frequently isolated species worldwide, and accounts for 60% of cases in the developing world; S. sonnei causes 77% of cases in the developed world, compared to only 15% of cases in the developing world; and S. dysenteriae is usually the cause of epidemics of dysentery, particularly in confined populations such as refugee camps.[12]
Each of the Shigella genomes includes a virulence plasmid that encodes conserved primary virulence determinants. The Shigella chromosomes share most of their genes with those of E. coli K12 strain MG1655.[13] Phylogenetic studies indicate Shigella is more appropriately treated as subgenus of Escherichia, and that certain strains generally considered E. coli – such as E. coli O157:H7 – are better placed in Shigella (see Escherichia coli#Diversity for details).
Pathogenesis
Shigella infection is typically by ingestion. Depending on the health of the host, fewer than 100 bacterial cells can be enough to cause an infection.[14] Shigella species generally invade the epithelial lining of the colon, causing severe inflammation and death of the cells lining the colon. This inflammation results in the diarrhea and even dysentery that are the hallmarks of Shigella infection.[11] Some strains of Shigella produce toxins which contribute to disease during infection. S. flexneri strains produce ShET1 and ShET2, which may contribute to diarrhea.[11] S. dysenteriae strains produce the enterotoxin Shiga toxin, which is similar to the verotoxin produced by enterohemorrhagic E. coli. Both Shiga toxin and verotoxin are associated with causing potentially fatal hemolytic uremic syndrome.[11]
Shigella species invade the host through the M-cells interspersed in the gut epithelia of the small intestine, as they do not interact with the apical surface of epithelial cells, preferring the basolateral side.[15] Shigella uses a type-III secretion system, which acts as a biological syringe to translocate toxic effector proteins to the target human cell. The effector proteins can alter the metabolism of the target cell, for instance leading to the lysis of vacuolar membranes or reorganization of actin polymerization to facilitate intracellular motility of Shigella bacteria inside the host cell. For instance, the IcsA effector protein triggers actin reorganization by N-WASP recruitment of Arp2/3 complexes, helping cell-to-cell spread.[citation needed]
After invasion, Shigella cells multiply intracellularly and spread to neighboring epithelial cells, resulting in tissue destruction and characteristic pathology of shigellosis.[16][17]
The most common symptoms are diarrhea, fever, nausea, vomiting, stomach cramps, and flatulence. It is also commonly known to cause large and painful bowel movements. The stool may contain blood, mucus, or pus. Hence, Shigella cells may cause dysentery. In rare cases, young children may have seizures. Symptoms can take as long as a week to appear, but most often begin two to four days after ingestion. Symptoms usually last for several days, but can last for weeks. Shigella is implicated as one of the pathogenic causes of reactive arthritis worldwide.[18]
Diagnosis
The diagnosis of shigellosis is made by isolating the organism from diarrheal fecal sample cultures. Shigella species are negative for motility and are generally not lactose fermenters, but S. sonnei can ferment lactose.[19] They typically do not produce gas from carbohydrates (with the exception of certain strains of S. flexneri) and tend to be overall biochemically inert. Shigella should also be urea hydrolysis negative. When inoculated to a triple sugar iron slant, they react as follows: K/A, gas -, and H2S -. Indole reactions are mixed, positive and negative, with the exception of S. sonnei, which is always indole negative. Growth on Hektoen enteric agar produces bluish-green colonies for Shigella and bluish-green colonies with black centers for Salmonella.
Prevention and treatment
Hand washing before handling food and thoroughly cooking all food before eating decreases the risk of getting shigellosis.[20]
Currently, no licensed vaccine targeting Shigella exists. Shigella has been a longstanding World Health Organization target for vaccine development. Sharp declines in age-specific diarrhea/dysentery attack rates for this pathogen indicate natural immunity does develop following exposure; thus, vaccination to prevent the disease should be feasible. Several vaccine candidates for Shigella are in various stages of development.[7][12]
Treatment mainly consists of replacing fluids and salts lost due to diarrhea. Severe dysentery can be treated with ampicillin, TMP-SMX, or fluoroquinolones, such as ciprofloxacin. Medical treatment should only be used in severe cases or for certain populations with mild symptoms (elderly, immunocompromised, food service industry workers, child care workers). For Shigella-associated diarrhea, antibiotics shorten the length of infection,[21] but they are usually avoided in mild cases because many Shigella strains are becoming resistant to common antibiotics. Furthermore, effective medications are often in short supply in developing countries, which carry the majority of the disease burden from Shigella. Antidiarrheal agents may worsen the sickness, and should be avoided.[22]
Also extensive research has been conducted into therapies, involving treatment with bacteriophages.[23]
See also
References
- ^ Yabuuchi, Eiko (2002). "Bacillus dysentericus (sic) 1897 was the first taxonomic rather than Bacillus dysenteriae 1898". International Journal of Systematic and Evolutionary Microbiology. 52 (Pt 3): 1041. doi:10.1099/00207713-52-3-1041. PMID 12054222.
- ^ Ryan, Kenneth James; Ray, C. George, eds. (2004). Sherris medical microbiology: an introduction to infectious diseases (4th ed.). McGraw-Hill Professional Med/Tech. ISBN 978-0-8385-8529-0.[page needed]
- ^ Pond, Kathy (2005). "Shigella". Water recreation and disease. Plausibility of associated infections: Acute effects, sequelae and mortality. WHO. pp. 113–8. ISBN 978-92-4-156305-5.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ "Shigellosis" (PDF). European Association of Zoo and Wildlife Veterinarians.
- ^ Mims, Cedric; Dockrell, Hazel; Goering, Richard; Roitt, Ivan; Wakelin, Derek; Zuckerman, Mark, eds. (2004). Medical Microbiology (3rd ed.). Mosby. p. 287. ISBN 978-0-7234-3259-3.
- ^ a b Bowen A (2016). "Chapter 3: Infectious Diseases Related to Travel". The Yellow Book: Health Information for International Travel. CDC. ISBN 978-0-19-937915-6. Retrieved 22 June 2016.
- ^ a b Mani, Sachin; Wierzba, Thomas; Walker, Richard I (2016). "Status of vaccine research and development for Shigella". Vaccine. 34 (26): 2887–2894.
- ^ Kotloff, Karen L; Nataro, James P; Blackwelder, William C; et al. (2013). "Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study". The Lancet. 382 (9888): 209–222.
{{cite journal}}: Explicit use of et al. in:|last4=(help) - ^ Ansaruzzaman, M; Kibriya, AK; Rahman, A; Neogi, PK; Faruque, AS; Rowe, B; Albert, MJ (1995). "Detection of provisional serovars of Shigella dysenteriae and designation as S. dysenteriae serotypes 14 and 15". Journal of Clinical Microbiology. 33 (5): 1423–5. PMC 228185. PMID 7615772.
- ^ Yang, Z; Hu, C; Chen, J; Chen, G; Liu, Z (1990). "[A new serotype of Shigella boydii]". Wei Sheng Wu Xue Bao (in Chinese). 30 (4): 284–95. PMID 2251827.
- ^ a b c d Hale, Thomas L.; Keusch, Gerald T. (1996). "Shigella". In Baron, Samuel (ed.). Medical microbiology (4th ed.). Galveston, Texas: University of Texas Medical Branch. ISBN 978-0-9631172-1-2.
{{cite book}}: External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help) - ^ a b "Shigellosis". State of the art of new vaccine research and development (PDF). Immunization, Vaccines and Biologicals. World Health Organization. 2006. pp. 10–2.
- ^ Yang, Fan; Yang, Jian; Zhang, Xiaobing; Chen, Lihong; Jiang, Yan; Yan, Yongliang; Tang, Xudong; Wang, Jing; Xiong, Zhaohui; Dong, Jie; Xue, Ying; Zhu, Yafang; Xu, Xingye; Sun, Lilian; Chen, Shuxia; Nie, Huan; Peng, Junping; Xu, Jianguo; Wang, Yu; Yuan, Zhenghong; Wen, Yumei; Yao, Zhijian; Shen, Yan; Qiang, Boqin; Hou, Yunde; Yu, Jun; Jin, Qi (2005). "Genome dynamics and diversity of Shigella species, the etiologic agents of bacillary dysentery". Nucleic Acids Research. 33 (19): 6445–58. doi:10.1093/nar/gki954. PMC 1278947. PMID 16275786.
- ^ Levinson, Warren E (2006). Review of Medical Microbiology and Immunology (9th ed.). McGraw-Hill Medical Publishing Division. p. 30. ISBN 978-0-07-146031-6.
- ^ Mounier, Joëlle; Vasselon, T; Hellio, R; Lesourd, M; Sansonetti, PJ (January 1992). "Shigella flexneri Enters Human Colonic Caco-2 Epithelial Cells through the Basolateral Pole". Infection and Immunity. 60 (1): 237–248. PMC 257528. PMID 1729185.
- ^ Todar, Kenneth. "Shigella and Shigellosis". Todar's Online Textbook of Bacteriology.[self-published source?]
- ^ Suzuki, Toshihiko; Sasakawa, Chihiro (2001). "Molecular basis of the intracellular spreading of Shigella". Infection and Immunity. 69 (10): 5959–66. doi:10.1128/IAI.69.10.5959-5966.2001. PMC 98722. PMID 11553531.
- ^ Hill Gaston, J (2003). "Arthritis associated with enteric infection". Best Practice & Research Clinical Rheumatology. 17 (2): 219–39. doi:10.1016/S1521-6942(02)00104-3. PMID 12787523.
- ^ Ito, Hideo; Kido, Nobuo; Arakawa, Yoshichika; Ohta, Michio; Sugiyama, Tsuyoshi; Kato, Nobuo (1991). "Possible mechanisms underlying the slow lactose fermentation phenotype in Shigella spp". Applied and Environmental Microbiology. 57 (10): 2912–7. PMC 183896. PMID 1746953.
- ^ Ram, P. K.; Crump, J. A.; Gupta, S. K.; Miller, M. A.; Mintz, E. D. (2008). "Part II. Analysis of data gaps pertaining to Shigella infections in low and medium human development index countries, 1984–2005". Epidemiology and Infection. 136 (5): 577–603. doi:10.1017/S0950268807009351. PMC 2870860. PMID 17686195.
- ^ Christopher, Prince RH; David, Kirubah V; John, Sushil M; Sankarapandian, Venkatesan; Christopher, Prince RH (2010). "Antibiotic therapy for Shigella dysentery". The Cochrane Database of Systematic Reviews (8): CD006784. doi:10.1002/14651858.CD006784.pub4. PMID 20687081.
- ^ "How can Shigella infections be treated?". Shigellosis: General Information. Centers for Disease Control and Prevention. Retrieved February 11, 2012.
- ^ Goodridge, Lawrence D. (2013). "Bacteriophages for managingShigellain various clinical and non-clinical settings". Bacteriophage. 3 (1): e25098. doi:10.4161/bact.25098. PMC 3694061. PMID 23819110.
External links
- Shigella genomes and related information at PATRIC, a Bioinformatics Resource Center funded by NIAID
- Vaccine Resource Library: Shigellosis and enterotoxigenic Escherichia coli (ETEC)
- US Centers for Disease Control and Prevention. Shigella - Shigellosis
