Colitis
| Colitis | |
|---|---|
 | |
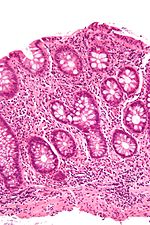
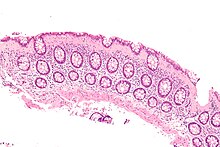
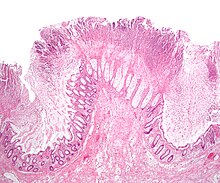
| A micrograph demonstrating cryptitis, a microscopic correlate of colitis. H&E stain. | |
| Specialty | Gastroenterology |
Colitis is swelling or inflammation of the large intestine (colon).[1] Colitis may be acute and self-limited or long-term. It broadly fits into the category of digestive diseases.
In a medical context, the label colitis (without qualification) is used if:
- The cause of the inflammation in the colon is undetermined; for example, colitis may be applied to Crohn's disease at a time when the diagnosis is unknown, or
- The context is clear; for example, an individual with ulcerative colitis is talking about their disease with a physician who knows the diagnosis.
Signs and symptoms
The signs and symptoms of colitis are quite variable and dependent on the cause of the given colitis and factors that modify its course and severity.[citation needed]
Common symptoms of colitis may include: mild to severe abdominal pains and tenderness (depending on the stage of the disease), persistent hemorrhagic diarrhea with pus either present or absent in the stools, fecal incontinence, flatulence, fatigue, loss of appetite and unexplained weight loss.[2]
More severe symptoms may include: shortness of breath, a fast or irregular heartbeat and fever.[2]
Other less common or rare non-specific symptoms that may accompany colitis include: arthritis, mouth ulcers, painful, red and swollen skin and irritated, bloodshot eyes.[2]
Signs seen on colonoscopy include: colonic mucosal erythema (redness of the colon's inner surface), ulcerations and hemorrhage.[medical citation needed]
Diagnosis
Symptoms suggestive of colitis are worked-up by obtaining the medical history, a physical examination and laboratory tests (CBC, electrolytes, stool culture and sensitivity, stool ova and parasites et cetera). Additional tests may include medical imaging (e.g. abdominal computed tomography, abdominal X-rays) and an examination with a camera inserted into the rectum (sigmoidoscopy, colonoscopy).[3]
An important investigation in the assessment of colitis is biopsy. A very small piece of tissue (usually about 2mm) is removed from the bowel mucosa during endoscopy and examined under the microscope by a histopathologist. It can provide important information regarding the cause of the disease and the extent of bowel damage.[citation needed]
Types
There are many types of colitis. They are usually classified by the cause.
Types of colitis include:
Autoimmune
- Inflammatory bowel disease (IBD) – a group of chronic colitides.
- Ulcerative colitis (UC) – a chronic colitis that affects the large intestine.
- Crohn's disease (CD) – another type of IBD that often leads to colitis.
Unknown
- Microscopic colitis – a colitis diagnosed by microscopic examination of colonic tissue; macroscopically ("to the eye") it appears normal.
Treatment-caused
- Diversion colitis
- Chemical colitis
- Chemotherapy-induced colitis
- Radiation colitis
- Checkpoint inhibitor induced colitis
Vascular disease
Infectious
- Infectious colitis
A subtype of infectious colitis is Clostridioides difficile colitis,[4] which is informally abbreviated as "C-diff colitis". It classically forms pseudomembranes and is often referred to as pseudomembranous colitis, which is its (nonspecific) histomorphologic description.
Enterohemorrhagic colitis may be caused by Shiga toxin in Shigella dysenteriae or Shigatoxigenic group of Escherichia coli (STEC), which includes serotype O157:H7 and other enterohemorrhagic E. coli.[5]
Parasitic infections, like those caused by Entamoeba histolytica, can also cause colitis.
Unclassifiable colitides
Indeterminate colitis is the classification for colitis that has features of both Crohn's disease and ulcerative colitis.[6] Indeterminate colitis' behaviour is usually closer to ulcerative colitis than Crohn's disease.[7]
Atypical colitis is a phrase that is occasionally used by physicians for a colitis that does not conform to criteria for accepted types of colitis. It is not an accepted diagnosis per se and, as such, a colitis that cannot be definitively classified.[citation needed]
Treatment
Some people may be admitted into the hospital following the colonoscopy depending on results. It is sometimes necessary to get the patient started on a steroid to speed up the healing of the colon. It may also be necessary to get the patient hydrated from the fluid loss and iron replaced from the loss of blood. After a hospital stay, the patient may be put on a daily medication to manage their chronic colitis. The medication can be an anti-inflammatory or an immunosuppressant. There are many different types of medication used and the doctor will prescribe the one they see fit. If the patient doesn't respond, new medications will be tried until there is a good fit.[citation needed]
Moreover, several studies recently have found significant relationship between colitis and dairy allergy (including: cow milk, cow milk UHT and casein),[8][9][10][11] suggesting some patients may benefit from an elimination diet.
Research
In the lab, the CRISPR-Cas systems effectively killed C. difficile bacteria. Researchers tested this approach in mice infected with C. difficile. Two days after the CRISPR treatment, the mice showed reduced C. difficile levels. Next steps include retooling the phage to prevent C. difficile from returning after the initial effective killing.[12]
In 2022 Yang et al. published a report on a successful treatment, using mesenchymal stem cells, of experimental colitis in mice.[13]
Additional research was conducted by Huang et al. that analyzed specific genes and biological markers that are associated with the risk of colon cancer development in patients with colitis. The results showed a correlation between certain biomarkers and the development of disease.[14]
References
- ^ "Colitis". www.pennmedicine.org. July 1, 2021. Retrieved 2022-11-18.
- ^ a b c NHS Choices. "Ulcerative colitis - Symptoms - NHS Choices". www.nhs.uk. Retrieved 2015-11-03.
- ^ "Diagnosis of Ulcerative Colitis | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved 2022-11-18.
- ^ "Clostridium Difficile Colitis – Overview". WebMD, LLC. Retrieved 2006-09-15.
- ^ Beutin L (September 2006). "Emerging enterohaemorrhagic Escherichia coli, causes and effects of the rise of a human pathogen". Journal of Veterinary Medicine. B, Infectious Diseases and Veterinary Public Health. 53 (7): 299–305. doi:10.1111/j.1439-0450.2006.00968.x. PMID 16930272.
- ^ Romano C, Famiani A, Gallizzi R, Comito D, Ferrau' V, Rossi P (December 2008). "Indeterminate colitis: a distinctive clinical pattern of inflammatory bowel disease in children". Pediatrics. 122 (6): e1278 – e1281. doi:10.1542/peds.2008-2306. PMID 19047226. S2CID 1409823.
- ^ Melton GB, Kiran RP, Fazio VW, He J, Shen B, Goldblum JR, et al. (October 2010). "Do preoperative factors predict subsequent diagnosis of Crohn's disease after ileal pouch-anal anastomosis for ulcerative or indeterminate colitis?". Colorectal Disease. 12 (10): 1026–1032. doi:10.1111/j.1463-1318.2009.02014.x. PMID 19624520. S2CID 44406331.
- ^ Yang M, Geng L, Chen P, Wang F, Xu Z, Liang C, et al. (March 2015). "Effectiveness of dietary allergen exclusion therapy on eosinophilic colitis in Chinese infants and young children ≤ 3 years of age". Nutrients. 7 (3): 1817–1827. doi:10.3390/nu7031817. PMC 4377883. PMID 25768952.
- ^ Lucendo AJ, Serrano-Montalbán B, Arias Á, Redondo O, Tenias JM (July 2015). "Efficacy of Dietary Treatment for Inducing Disease Remission in Eosinophilic Gastroenteritis". Journal of Pediatric Gastroenterology and Nutrition. 61 (1): 56–64. doi:10.1097/MPG.0000000000000766. PMID 25699593. S2CID 26195645.
- ^ Judaki A, Hafeziahmadi M, Yousefi A, Havasian MR, Panahi J, Sayehmiri K, Alizadeh S (2014). "Evaluation of dairy allergy among ulcerative colitis patients". Bioinformation. 10 (11): 693–696. doi:10.6026/97320630010693. PMC 4261114. PMID 25512686.
- ^ Sun J, Lin J, Parashette K, Zhang J, Fan R (February 2015). "Association of lymphocytic colitis and lactase deficiency in pediatric population". Pathology, Research and Practice. 211 (2): 138–144. doi:10.1016/j.prp.2014.11.009. PMID 25523228.
- ^ "Study shows CRISPR effectiveness against colitis pathogen". medicalxpress.com. Retrieved 2020-03-13.
- ^ Yang F, Ni B, Liu Q, He F, Li L, Zhong X, et al. (September 2022). "Human umbilical cord-derived mesenchymal stem cells ameliorate experimental colitis by normalizing the gut microbiota". Stem Cell Research & Therapy. 13 (1): 475. doi:10.1186/s13287-022-03118-1. PMC 9476645. PMID 36104756.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Huang Y, Zhang X, Li Y, Yao J (June 2022). "Identification of hub genes and pathways in colitis-associated colon cancer by integrated bioinformatic analysis". BMC Genomic Data. 23 (1): 48. doi:10.1186/s12863-022-01065-7. PMC 9219145. PMID 35733095.
{{cite journal}}: CS1 maint: unflagged free DOI (link)
