Respiratory therapist: Difference between revisions
| Line 65: | Line 65: | ||
===Sleep Disorder Specialist=== |
===Sleep Disorder Specialist=== |
||
{{Main|Sleep disorder specialist}} |
{{Main|Sleep disorder specialist}} |
||
The Sleep Disorder Specialist is a [[Registered Respiratory Therapist]] whom performs sleep disorders testing and therapeutic intervention along with diagnosis of sleep related disease such as [[Obstructive Sleep Apnea]] or [[Central sleep apnea|Central Apnea]]. The role is very similar to the [[Polysomnographic Technologist]]. |
The Sleep Disorder Specialist is a [[Registered Respiratory Therapist]] ([[RRT-SDS]]) whom performs sleep disorders testing and therapeutic intervention along with diagnosis of sleep related disease such as [[Obstructive Sleep Apnea]] or [[Central sleep apnea|Central Apnea]]. The role is very similar to the [[Polysomnographic Technologist]]. |
||
===Case Management=== |
===Case Management=== |
||
Revision as of 21:22, 8 October 2011
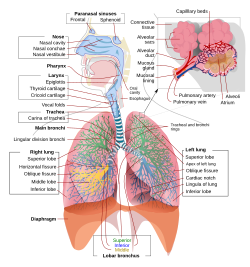 A complete view of the respiratory system. (Click to enlarge). | |
| Occupation | |
|---|---|
| Names | Respiratory Therapist, Cardiopulmonary Therapist |
Occupation type | Specialty |
Activity sectors | Medicine, Allied Health |
| Description | |
Education required | Associate of Science, Bachelors Degree, Masters Degree |
Fields of employment | Hospitals, Clinics |
Respiratory therapy is a healthcare profession in which specialists work with patients suffering from either acute or chronic respiratory problems. These specialists are termed Respiratory Therapists in most places internationally but may also be referred to as Respiratory Scientists or Respiratory Care Practitioners. Respiratory therapy clinicians are also sometimes referred to as cardio-pulmonary therapists or respiratory care practitioners. Respiratory therapists work independently and as part of a team to plan, integrate, and evaluate cardiac and pulmonary care.
Clinical practice

Respiratory therapists are found in various sectors of health care. In the hospital setting, respiratory therapists evaluate, treat and assist with diagnosis of respiratory/pulmonary diseases. In the United States, Registered Respiratory Therapists evaluate and treat patients with a great deal of autonomy under the direction of a pulmonologist[1], and in specialty facilities respiratory therapists are a preferred addition to surface or air transport[2]. In other settings respiratory therapists are found in schools as asthma educators, working with teachers and coachs about childhood symptoms of asthma and how to spot an emergency. In the United States, legislation has been introduced several times to allow asthma specialist registered respiratory therapists to prescribe and manage previously diagnosed respiratory patients in physician clinics.[3][4]. In sleep clinics respiratory therapists work with physicians in diagnosis of sleep-related illnesses.
History
Respiratory therapy is a young practice in the field of medicine, beginning in the United States around 1950 and in its current form beginning around 1990. In 2004 Vermont became the 48th state in the United States to enact a Respiratory Care Act, allowing for the practice and licensure of respiratory care clinicians in that state.
The Roman physician Galen may have been the first to describe mechanical ventilation: "If you take a dead animal and blow air through its larynx [through a reed], you will fill its bronchi and watch its lungs attain the greatest distention."[5] Vesalius too describes ventilation by inserting a reed or cane into the trachea of animals.[6] In 1908 George Poe demonstrated his mechanical respirator by asphyxiating dogs and seemingly bringing them back to life.[7]
Respiratory therapy has grown considerably through the past four decades. There was a time when respiratory therapists were on-the-job trained technicians, with little formal education. Their main function was to ensure safe oxygen use, to administer intermittent positive pressure breathing (IPPB) treatments, to perform cardiopulmonary resuscitation (CPR), and to operate negative pressure (iron lung) ventilators. They were initially titled inhalation therapists. With the advent of positive pressure mechanical ventilators, the more widespread hospital provision of Neonatal and Pediatric care, more sophisticated pulmonary function testing (PFT), a need for thoroughly trained clinical practitioners presented itself. Over the years respiratory therapists have evolved to being college and university trained clinicians who work in a variety of settings.
Treatment
Medication — Medication is the most important treatment of most diseases of pulmonology, usually by inhalation (bronchodilators and steroids) or also by mouth or IV(antibiotics, leukotriene antagonists). A common example being the usage of inhalers in the treatment of inflammatory lung conditions such as Asthma or Chronic obstructive pulmonary disease (Emphysema. Oxygen therapy is often necessary in severe respiratory disease such as pulmonary fibrosis.
Intensive Care — Mechanical ventilation may be required in instances of rapidly advancing disease or difficulty after surgery. Different modes of mechanical ventilation are used for various instances depending on the patients need.
Pulmonary Rehabilitation — Pulmonary rehabilitation may be initiated as a treatment as a source for continuity of improvement after a hospital stay or as a therapeutic way to increase quality of life. Pulmonary rehabilitation is intended to educate the patient, the family, and improve the overall quality of life and prognosis for the patient. Pulmonary Rehabilitation involves therapies and evaluations by Respiratory Therapists, Occupational Therapists and Physical Therapists.
Respiratory therapy as a career
In the United States and Canada, Respiratory Therapists are therapists who, after receiving a degree in cardiopulmonary science or respiratory science complete a credentialing process. After satisfactorily completing the required examinations and added to a registry, the therapist is then eligible to apply for a license to practice in their respective state or territory.
In the United States, specialist respiratory therapists are clinicians who hold specialized credentials in a specific field of study, such as a Asthma Educator or a Neonatal & Pediatric Transport Specialist.
Scientific research
Respiratory scientists are specialists in pulmonary function. Respiratory therapists work with Pulmonologists in both clinical and general research of the respiratory system, ranging from the anatomy of the respiratory epithelium to the most effective treatment of pulmonary hypertension in pediatrics. Scientific research also takes place to look for causes and possible treatment in diseases such as asthma and lung cancer.
Specialty areas
Asthma
Asthma specialist's work with clinics, hospitals and schools as an educator for teachers and practitioners on asthma and allergies. Respiratory Therapists in the role as an Asthma Educator additionally help diagnose and treat asthma and other respiratory illness.[8] An Asthma Educator is the resource clinician in inpatient and outpatient environments for evaluating and advising physicians on treatment plans and helping facilitate patient understanding and compliance with the plan. In the United States, Certified Asthma Educators (AE-C) are credentialed by the National Asthma Educator Certification Board (NAECB).[9]
Cystic fibrosis
Respiratory Therapists work with people suffering from cystic fibrosis in clinics and hospitals[10] by educating them about their disease and working with them on a treatment plan. While admitted to a hospital, patients with cystic fibrosis have their treatment schedule modified and maintained by respiratory therapists. Maintaining a healthy schedule for pharmokonetic and physical therapeutic airway clearance typically more frequent than home treatment plans because admissions are usually due to an increased need for therapy during the stay.
Extracorporeal Membrane Oxygenation (ECMO)
Extracorporeal membrane oxygenation (ECMO) is a modified cardiopulmonary bypass technique used for the treatment of life threatening cardiac or respiratory failure. An ECMO Specialist is the technical specialist educated to manage the ECMO system including blood pump, tubing, artificial oxygenator, and related equipment. The ECMO Specialist, under qualified medical direction and supervision, is also responsible for the clinical needs of the patient on ECMO which can include maintenance of normal acid-base balance, oxygenation, and ventilation, administration of blood and blood by-products, medication delivery, and maintenance of appropriate anticoagulation therapies for the blood.[11]
Intensive care
Intensive Care is one of the mainstays of respiratory therapy. Respiratory Therapists are taking an increased clinical role in recent years related to intensive care. Ventilatory support is usually the largest criteria for being placed into an intensive care setting which is maintained entirely by Respiratory Therapists and Cardiopulmonary specialists. Mechanical Ventilation is a rapidly expanding science and has been recognized as a complex technology by the respiratory therapy credentialing agency (NBRC) who in 2011 added the speciality credential called the "Adult Critical Care Specialist", available only to the registered respiratory therapist (RRT-ACCS).[12]
Neonatal & Pediatric Intensive Care
Much like adult intensivist therapists neonatal and pediatric specialists deal primarily with monitoring ventilation and perfusion[13]. The NPS practitioner is trained extensively in antenatal and intrapartum patients and family. Neonatal assessment and laboratory studies. The practitioner is also a specialist in ventilatory support and cardio-pulmonary therapy of neonatal and pediatric patients[13]. In the United States NPS credentialing is available to both the certified respiratory therapist (CRT-NPS) and the registered respiratory therapist (RRT-NPS) however the registered respiratory therapist (RRT-NPS) is preferred by most organizations[13][14].
Sleep Disorder Specialist
The Sleep Disorder Specialist is a Registered Respiratory Therapist (RRT-SDS) whom performs sleep disorders testing and therapeutic intervention along with diagnosis of sleep related disease such as Obstructive Sleep Apnea or Central Apnea. The role is very similar to the Polysomnographic Technologist.
Case Management
Case management is a collaborative process that assesses, plans, implements, coordinates, monitors, and evaluates the options and services required to meet the client's health and human services needs. It is characterized by advocacy, communication, and resource management and promotes quality and cost-effective interventions and outcomes. Eligibility and certification is maintained by the Commission for Case Management Certification, a body certifying healthcare professionals in the United States.[15]
Surface & Air Transport
Respiratory therapists work with nurses, physicians, and paramedics in emergency flight and ground transport.[16] They are a vital practitioner delivering care inside helicopters, air ambulance or ground ambulance working to pick up a patient and move them to a facility that has what they need. In the United States certification for transport (C-NPT) is currently awarded by The National Certification Corporation.[17] The NREMT has included respiratory therapists as qualifing for the advanced credentialing as a critical care paramedic CCEMT-P.
Respiratory therapy associations
North America
AARC — The American Association for Respiratory Care is a professional organization representing respiratory clinicians in the United States. Founded in 1943, the AARC has served as the only professional association for Respiratory Care in the US.
CSRT — The Canadian Society for Respiratory Therapists is the professional association and sole credentialing agency for Respiratory Therapists in Canada.
Latin America
LABPCRT — The LABPCRT is a credentialing association that maintains a registry and credentials practitioners in the nations of Colombia, Costa Rica, Guatemala, Mexico, Panama and Venezuela.
Middle East
SSRC — The Saudi Society for Respiratory Care is the association and credentialing agency serving the Kingdom of Saudi Arabia.
References
- ^ Harbrecht BG, Delgado E, Tuttle RP, Cohen-Melamed MH, Saul MI, Valenta CA (2009). "Improved outcomes with routine respiratory therapist evaluation of non-intensive-care-unit surgery patients". Respir Care. 54 (7): 861–7. PMID 19558737.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ O'Malley RJ, Rhee KJ (1993). "Contribution of air medical personnel to the airway management of injured patients". Air Med J. 12 (11–12): 425–8. doi:10.1016/S1067-991X(05)80138-5. PMID 10130326.
- ^ 112th Congress (2011) (Mar 8, 2011). "H.R. 941". Legislation. GovTrack.us. Retrieved August 28, 2011.
Medicare Respiratory Therapy Initiative Act of 2011
{{cite web}}: CS1 maint: numeric names: authors list (link) - ^ 110th Congress (2007) (Oct 25, 2007). "H.R. 3968". Legislation. GovTrack.us. Retrieved August 28, 2011.
Medicare Respiratory Therapy Initiative Act of 2007
{{cite web}}: CS1 maint: numeric names: authors list (link) - ^ Colice, Gene L (2006). "Historical Perspective on the Development of Mechanical Ventilation". In Martin J Tobin (ed.). Principles & Practice of Mechanical Ventilation (2 ed.). New York: McGraw-Hill. ISBN 978-0071447676.
- ^ Chamberlain D (2003) "Never quite there: A tale of resuscitation medicine" Clinical Medicine, Journal of the Royal College of Physicians' 3 6:573-577
- ^ "Smother Small Dog To See it Revived. Successful Demonstration of an Artificial Respiration Machine Cheered in Brooklyn. Women in the Audience, But Most of Those Present Were Physicians. The Dog, Gathered in from the Street, Wagged Its Tail". New York Times. May 29, 1908, Friday. Retrieved 2007-12-25.
An audience, composed of about thirty men and three or four women, most of the men being physicians, attended a demonstration of Prof. George Poe's machine for producing artificial respiration in the library of the Kings County Medical Society, at 1,313 Bedford Avenue, Brooklyn, last night, under the auspices of the First Legion of the Red Cross Society.
{{cite news}}: Check date values in:|date=(help); Cite has empty unknown parameter:|coauthors=(help) - ^ http://www.childrenshospital.vanderbilt.org/interior.php?mid=6587 Vanderbilt Children's Asthma Clinic
- ^ http://www.naecb.org National Asthma Educator Certification Board (NAECB)
- ^ http://www.childrenshospital.vanderbilt.org/interior.php?mid=6618 Vanderbilt Childrens Hospital Cystic Fibrosis Clinic
- ^ http://www.wakehealth.edu/ecmo/ Wake Forrest Baptist Health
- ^ http://www.nbrc.org/Examinations/ACCS/tabid/113/Default.aspx National Board of Respiratory Care, Adult Critical Care Specialist
- ^ a b c Kashani KB, Farmer JC (2006). "The support of severe respiratory failure beyond the hospital and during transportation". Curr Opin Crit Care. 12 (1): 43–9. PMID 16394783.
- ^ Beninati W, Meyer MT, Carter TE (2008). "The critical care air transport program". Crit Care Med. 36 (7 Suppl): S370-6. doi:10.1097/CCM.0b013e31817e3143. PMID 18594265.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ http://www.ccmcertification.org/secondary.php?section=About Commission for Case Management Certification
- ^ http://www.vanderbilthealth.com/lifeflight/16045
- ^ http://www.nccwebsite.org/catalogs/exam-npt/ The National Certification Corporation
