Usual interstitial pneumonia: Difference between revisions
m Journal cites, added 1 DOI using AWB (10270) |
|||
| Line 10: | Line 10: | ||
==Causes== |
==Causes== |
||
The cause of the scarring in UIP may be known (less commonly) or unknown (more commonly). Since the medical term for conditions of unknown cause is "idiopathic", the clinical term for UIP of unknown cause is [[idiopathic pulmonary fibrosis]] (IPF). Examples of known causes of UIP include [[systemic sclerosis]]/[[scleroderma]], [[rheumatoid arthritis]], [[asbestosis]] and chronic [[nitrofurantoin]] toxicity. |
The cause of the scarring in UIP may be known (less commonly) or unknown (more commonly). Since the medical term for conditions of unknown cause is "idiopathic", the clinical term for UIP of unknown cause is [[idiopathic pulmonary fibrosis]] (IPF). Examples of known causes of UIP include [[systemic sclerosis]]/[[scleroderma]], [[rheumatoid arthritis]], [[asbestosis]], and chronic [[nitrofurantoin]] toxicity. |
||
==Symptoms== |
==Symptoms== |
||
Revision as of 18:49, 23 January 2015
| Usual interstitial pneumonia |
|---|
Usual interstitial pneumonia (UIP) is a form of lung disease characterized by progressive scarring of both lungs.[1] The scarring (fibrosis) involves the supporting framework (interstitium) of the lung. UIP is thus classified as a form of interstitial lung disease. The term "usual" refers to the fact that UIP is the most common form of interstitial fibrosis. "Pneumonia" indicates "lung abnormality", which includes fibrosis and inflammation. The term used for UIP in the British literature is cryptogenic fibrosing alveolitis, a term that has fallen out of favor since the basic underlying pathology is now thought to be fibrosis, not inflammation.
Causes
The cause of the scarring in UIP may be known (less commonly) or unknown (more commonly). Since the medical term for conditions of unknown cause is "idiopathic", the clinical term for UIP of unknown cause is idiopathic pulmonary fibrosis (IPF). Examples of known causes of UIP include systemic sclerosis/scleroderma, rheumatoid arthritis, asbestosis, and chronic nitrofurantoin toxicity.
Symptoms
The typical symptoms of UIP are progressive shortness of breath and cough for a period of months. In some patients, UIP is diagnosed only when a more acute disease supervenes and brings the patient to medical attention.
Diagnosis
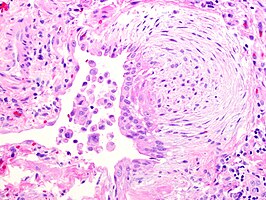
UIP may be diagnosed by a radiologist using a computed tomogram of the chest (CT scan of the chest), or by a pathologist using tissue obtained by a lung biopsy. Radiologically, the main feature required for a confident diagnosis of UIP is honeycomb change in the periphery and the lower portions (bases) of the lungs.[2] The histologic hallmarks of UIP, as seen in lung tissue under a microscope by a pathologist, are interstitial fibrosis in a "patchwork pattern", honeycomb change and fibroblast foci (see images below).[3]
- Pathological findings in usual interstitial pneumonia (UIP)
-
Appearance of usual interstitial pneumonia (UIP) in a surgical lung biopsy at low magnification. The tissue is stained with hematoxylin (purple dye) and eosin (pink dye) to make it visible. The pink areas in this picture represent lung fibrosis (collagen stains pink). Note the "patchwork" (quilt-like) pattern of the fibrosis.
-
Appearance of honeycomb change in a surgical lung biopsy at low magnification. The dilated spaces seen here are filled with mucin. Hematoxylin-eosin stain, low magnification.
-
A fibroblast focus in a surgical lung biopsy of UIP. Hematoxylin-eosin stain, high magnification. The white space to the left is an airspace. The pale area to the right is a fibroblast focus. It is an area of active fibroblast proliferation within the interstitium of the lung.
Differential diagnosis
The differential diagnosis includes other types of lung disease that cause similar symptoms and show similar abnormalities on chest radiographs. Some of these diseases cause fibrosis, scarring or honeycomb change. The most common considerations include:
- chronic hypersensitivity pneumonitis
- non-specific interstitial pneumonia
- sarcoidosis
- pulmonary Langerhans cell histiocytosis
- asbestosis [4]
Prognosis
Regardless of etiology, UIP is relentlessly progressive, usually leading to respiratory failure and death. Some patients do well for a prolonged period of time, but then deteriorate rapidly because of a superimposed acute illness (so-called "accelerated UIP"). The outlook for long-term survival is poor. In most studies, the median survival is 3 to 4 years. Patients with UIP in the setting of rheumatoid arthritis have a slightly better prognosis than UIP without a known cause (IPF).
History
UIP, as a term, first appeared in the pathology literature. It was coined by Averill Abraham Liebow.[5]
See also
References
- ^ Travis WD, King TE, Bateman ED; et al. (2002). "ATS/ERS international multidisciplinary consensus classification of idiopathic interstitial pneumonias. General principles and recommendations". American Journal of Respiratory and Critical Care Medicine. 165 (5): 277–304. doi:10.1164/ajrccm.165.2.ats01. PMID 11790668.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Sumikawa H; et al. (2008). "Computed tomography findings in pathological usual interstitial pneumonia: relationship to survival". American Journal of Respiratory and Critical Care Medicine. 177 (4): 433–439. doi:10.1164/rccm.200611-1696OC. PMID 17975197.
{{cite journal}}: Explicit use of et al. in:|author=(help) - ^ Katzenstein AL, Mukhopadhyay S, Myers JL (2008). "Diagnosis of usual interstitial pneumonia and distinction from other fibrosing interstitial lung diseases". Human Pathology. 39 (9): 1275–1294. doi:10.1016/j.humpath.2008.05.009. PMID 18706349.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Leslie, Kevin O; Wick, Mark R. (2005). Practical pulmonary pathology: a diagnostic approach. Edinburgh: Churchill Livingstone. ISBN 0-443-06631-0. OCLC 156861539.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ^ Averill Abraham Liebow at Who Named It?