Dementia with Lewy bodies: Difference between revisions
→Core features: And again. Now I remember why I don't come here any more. |
revert pointy comments that could be stated on talk or simply implemented in edits. which will i will do some of, in next edits |
||
| Line 58: | Line 58: | ||
In other severe cases of dementia (for example, advanced stages of AD), core features of DLB may also be present.<ref name= Walker2015/> |
In other severe cases of dementia (for example, advanced stages of AD), core features of DLB may also be present.<ref name= Walker2015/> |
||
'''Cognition, alertness or attention fluctuate''' throughout the day |
'''Cognition, alertness or attention fluctuate''' throughout the day and these fluctuations are often present early in the course of the disease.<ref name=McKeithConsensus2017/><ref name=Gomperts2016/> Impaired attention, [[executive function]], and visuospatial function are common symptoms.<ref name=Gomperts2016/> Karantzoulis and Galvin (2011) write that "marked attentional and executive function disturbance is central" and "attentional disturbance may serve as the basis of fluctuating cognition that is characteristic".<ref name=Karant2011/> Problems with executive function surface in activities requiring planning and organizing.<ref name= Levin2016/> These deficits can present with impaired job performance, difficulty multitasking, inability to follow conversations, or problems driving a car—such as becoming lost or misjudging distances.<ref name=Gomperts2016/> Individuals with DLB may be easily distracted, and have a hard time focusing on tasks,<ref name=Karant2011/> or appear to be "delirium-like", "zoning out", or in states of altered consciousness.<ref name=McKeithConsensus2017/> They may also exhibit disorganized speech and changing ability to organize their thoughts during the day.<ref name=McKeithConsensus2017/><ref name=Gomperts2016/> A person with DLB may experience problems of [[wakefulness]] or [[sleep disorder]]s including daytime sleepiness, drowsiness or napping more than two hours a day, [[insomnia]], and [[restless legs syndrome]].<ref name=NINDS2017Book/> |
||
{{quote box |
{{quote box |
||
| Line 71: | Line 71: | ||
'''REM sleep behavior disorder''' is a [[parasomnia]] that occurs frequently in DLB and may appear decades before any other symptoms, often as the first clinical indication of DLB and an [[prodome|early sign]] of a [[synucleinopathy]].<ref name=StLouisMay2017>{{cite journal |vauthors=St Louis EK, Boeve AR, Boeve BF |title=REM sleep behavior disorder in Parkinson's disease and other synucleinopathies |journal=Mov. Disord. |volume=32 |issue=5 |pages=645–58 |date=May 2017 |pmid=28513079 |doi=10.1002/mds.27018|type=Review }}</ref> Individuals with RBD lose the [[atony|paralysis of muscles (atonia)]] that is normal during [[rapid eye movement sleep|rapid eye movement (REM) sleep]], and act out their dreams or have other abnormal movements or vocalizations.<ref name=StLouisNov2017/> The individual with RBD may not be aware that they act out their dreams;<ref name=StLouisMay2017/> a bed partner may be the only person who knows of these behaviors.<ref name=NINDS2017Book/> |
'''REM sleep behavior disorder''' is a [[parasomnia]] that occurs frequently in DLB and may appear decades before any other symptoms, often as the first clinical indication of DLB and an [[prodome|early sign]] of a [[synucleinopathy]].<ref name=StLouisMay2017>{{cite journal |vauthors=St Louis EK, Boeve AR, Boeve BF |title=REM sleep behavior disorder in Parkinson's disease and other synucleinopathies |journal=Mov. Disord. |volume=32 |issue=5 |pages=645–58 |date=May 2017 |pmid=28513079 |doi=10.1002/mds.27018|type=Review }}</ref> Individuals with RBD lose the [[atony|paralysis of muscles (atonia)]] that is normal during [[rapid eye movement sleep|rapid eye movement (REM) sleep]], and act out their dreams or have other abnormal movements or vocalizations.<ref name=StLouisNov2017/> The individual with RBD may not be aware that they act out their dreams;<ref name=StLouisMay2017/> a bed partner may be the only person who knows of these behaviors.<ref name=NINDS2017Book/> |
||
RBD behaviors may include yelling, screaming, laughing, crying, unintelligible talking,<ref name=StLouisMay2017/> non-violent flailing or more violent punching, kicking,<ref name=Walker2015/> choking or scratching. People with RBD may fall out of bed,<ref name=StLouisMay2017/> or injure themselves or their bed partner,<ref name=Boot2015/> often with limb movements. |
RBD behaviors may include yelling, screaming, laughing, crying, unintelligible talking,<ref name=StLouisMay2017/> non-violent flailing or more violent punching, kicking,<ref name=Walker2015/> choking or scratching. People with RBD may fall out of bed,<ref name=StLouisMay2017/> or injure themselves or their bed partner,<ref name=Boot2015/> often with limb movements.<ref name=McKeithConsensus2017/> There may be resulting bruises or fractures, and more serious injuries like [[subdural hematoma]].<ref name=StLouisNov2017/> The reported dream enactment behaviors are frequently violent,<ref name=Gomperts2016/> and involve a theme of being chased or attacked.<ref name=Boot2015/> However, because people are more likely to remember or report violent dreams and behaviors, and to be referred to a specialist when injury occurs, [[recall bias|recall]] or [[selection bias]] may explain the prevalence of violence reported in RBD.<ref name=StLouisMay2017/> |
||
About 80% of people with DLB have RBD.<ref name=StLouisMay2017/> Abnormal sleep behaviors may begin before cognitive decline is observed in DLB.<ref name=McKeithConsensus2017/> On autopsy, 94 to 98% of individuals with [[polysomnography]]-confirmed RBD are found to have a synucleinopathy<ref name=StLouisNov2017/><ref name=Boot2013>{{cite journal |vauthors=Boot BP, McDade EM, McGinnis SM, Boeve BF |title=Treatment of dementia with Lewy bodies |journal=Curr Treat Options Neurol |volume=15 |issue=6 |pages=738–64 |date=December 2013 |pmid=24222315 |pmc=3913181 |doi=10.1007/s11940-013-0261-6 |type=Review}}</ref><ref name=RBDSecPriLay>{{cite journal |vauthors=Boot BP |title=Comprehensive treatment of dementia with Lewy bodies |journal=Alzheimers Res Ther |volume=7 |issue=1 |page=45 |date=2015 |pmid=26029267 |pmc=4448151 |doi=10.1186/s13195-015-0128-z |type=Review | lay-url= https://www.mdedge.com/familypracticenews/article/58442/geriatrics/rem-sleep-problems-predict-parkinsons-lewy-body-dementia |lay-source= Family Practice News |lay-date= April 17, 2013}} Original study [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3745815/ here.]</ref>—most commonly DLB or Parkinson's disease—that develops within 15 years,<ref name=Walker2015/> and sometimes as long as 50 years after RBD. |
About 80% of people with DLB have RBD.<ref name=StLouisMay2017/> Abnormal sleep behaviors may begin before cognitive decline is observed in DLB.<ref name=McKeithConsensus2017/> On autopsy, 94 to 98% of individuals with [[polysomnography]]-confirmed RBD are found to have a synucleinopathy<ref name=StLouisNov2017/><ref name=Boot2013>{{cite journal |vauthors=Boot BP, McDade EM, McGinnis SM, Boeve BF |title=Treatment of dementia with Lewy bodies |journal=Curr Treat Options Neurol |volume=15 |issue=6 |pages=738–64 |date=December 2013 |pmid=24222315 |pmc=3913181 |doi=10.1007/s11940-013-0261-6 |type=Review}}</ref><ref name=RBDSecPriLay>{{cite journal |vauthors=Boot BP |title=Comprehensive treatment of dementia with Lewy bodies |journal=Alzheimers Res Ther |volume=7 |issue=1 |page=45 |date=2015 |pmid=26029267 |pmc=4448151 |doi=10.1186/s13195-015-0128-z |type=Review | lay-url= https://www.mdedge.com/familypracticenews/article/58442/geriatrics/rem-sleep-problems-predict-parkinsons-lewy-body-dementia |lay-source= Family Practice News |lay-date= April 17, 2013}} Original study [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3745815/ here.]</ref>—most commonly DLB or Parkinson's disease—that develops within 15 years,<ref name=Walker2015/> and sometimes as long as 50 years after RBD.<ref name=StLouisNov2017/> RBD may subside over time.<ref name=McKeithConsensus2017/> |
||
'''Parkinsonism''' |
'''Parkinsonism''' occurs in more than 85% of people with DLB, who may have one or more of the cardinal features that occur in Parkinson's disease—[[bradykinesia|slowness of movement]], rigidity,<ref name=McKeithConsensus2017/> and less commonly, [[tremor]] at rest.<ref name=Gomperts2016/> Motor symptoms may include [[shuffling gait]], problems with balance, falls, blank expression (reduced range of facial expression), low speech volume or a weak voice and [[difficulty swallowing]].<ref name=NINDS2017Book/> Presentation of motor symptoms is variable, but they are usually symmetric, presenting on both sides of the body.<ref name=Gomperts2016/> For a DLB diagnosis, only one of the cardinal symptoms of [[parkinsonism]] need be present,<ref name=McKeithConsensus2017/> and they may be less severe than in persons with Parkinson's disease.<ref name=Tousi2017/> |
||
'''Visual hallucinations''' are defined by Pezzoli, |
'''Visual hallucinations''' are defined by Pezzoli, et al (2017) as "well-formed images perceived without the presence of real stimuli".<ref name=Pezzoli2017/> Up to 80% of people with DLB have visual hallucinations.<ref name=McKeithConsensus2017/> early in the course of DLB.<ref name=Burghaus2012/> They are recurrent,<ref name=Pezzoli2017>{{cite journal |vauthors=Pezzoli S, Cagnin A, Bandmann O, Venneri A |title=Structural and functional neuroimaging of visual hallucinations in Lewy body disease: A systematic literature review |journal=Brain Sci |volume=7 |issue=7 |pages= |date=July 2017 |pmid=28714891 |pmc=5532597 |doi=10.3390/brainsci7070084 |type=Review}}</ref> frequent,<ref name=Burghaus2012>{{cite journal |vauthors=Burghaus L, Eggers C, Timmermann L, Fink GR, Diederich NJ |title=Hallucinations in neurodegenerative diseases |journal=CNS Neurosci Ther |volume=18 |issue=2 |pages=149–59 |date=February 2012 |pmid=21592320 |doi=10.1111/j.1755-5949.2011.00247.x |type=Review |url=https://onlinelibrary.wiley.com/doi/full/10.1111/j.1755-5949.2011.00247.x}}</ref> and usually involve animated perceptions of animals or people, including children and family members.<ref name=Gomperts2016/> They may be scenic, elaborate and detailed.<ref name=Burghaus2012/> |
||
These hallucinations can sometimes provoke fear, although their content is more typically neutral.<ref name=Gomperts2016/> They are not necessarily disturbing, |
These hallucinations can sometimes provoke fear, although their content is more typically neutral.<ref name=Gomperts2016/> They are not necessarily disturbing, and in some cases, the person with DLB may be conscious they are not real,<ref name=Boot2013/> and have [[Insight in psychology and psychiatry|insight]] about the hallucinations.<ref name=Burghaus2012/> In individuals with more disrupted cognition, the hallucinations can become more complex, and they may be less aware that their hallucinations are not real.<ref name=Pezzoli2017/> Individuals with visual hallucinations and either of the two Lewy body dementias have more cognitive impairment, and those cognitive deficits are predictive of hallucinations.<ref name=Pezzoli2017/> |
||
Different than visual ''hallucinations'' |
Different than visual ''hallucinations'', but also common in DLB, are visual misperceptions or ''illusions'', explained by Pezzoli (2017) as "incorrect perceptions of real stimuli".<ref name=Pezzoli2017/> The viewer with DLB may have problems with vision (for example, at night) and misinterpret what they see (for example, mistaking a pile of socks for snakes or a clothes closet for the bathroom).<ref name=Gomperts2016/> |
||
===Supportive features=== |
===Supportive features=== |
||
Revision as of 00:31, 12 April 2018
| Dementia with Lewy bodies | |
|---|---|
| Other names | Diffuse Lewy body disease, cortical Lewy body disease, senile dementia of Lewy type |
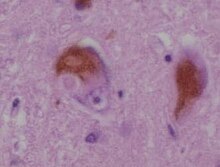 | |
| Microscopic image of Lewy bodies | |
| Specialty | Neurology |
| Symptoms | Dementia, abnormal behavior during REM sleep, fluctuations in alertness, visual hallucinations, slowness of movement[1] |
| Usual onset | After the age of 50[2] |
| Duration | Long term[2] |
| Causes | Unknown[3] |
| Diagnostic method | Based on symptoms and supported by specific biomarkers[1] |
| Differential diagnosis | Parkinson's disease dementia, Alzheimer's disease, certain mental illnesses, vascular dementia[1][4] |
| Medication | Acetylcholinesterase inhibitors such as donepezil,[4] melatonin[5] |
| Prognosis | Average survival 6 years, as long as 20[2] |
| Frequency | 0.4% (> 65 years old)[6] |
Dementia with Lewy bodies (DLB) is a type of dementia accompanied by changes in behavior, cognition and movement.[1][2] Dementia relentlessly worsens over time,[7] and is diagnosed when cognitive decline interferes with normal daily functioning.[1][8] Memory loss does not always present early.[9] A core feature of DLB is REM sleep behavior disorder (RBD), in which individuals lose the muscle paralysis that is normal during REM sleep and act out their dreams.[1] RBD may appear years or decades before other symptoms.[5] Other core symptoms include visual hallucinations; slowness of movement, trouble walking, or rigidity, and fluctuations in attention or alertness.[1] Urinary incontinence and constipation are common,[10] as are mood changes such as depression and apathy.[1]
The exact cause is unknown,[3] but involves deposits of Lewy bodies and Lewy neurites, abnormal clumps of alpha-synuclein protein, in neurons.[11][12] Typically, no family history is apparent,[3] but there is a genetic association in some families, and the APOE gene increases risk.[2][7] A probable diagnosis is based on symptoms and may be supported by specific biomarkers.[1] Blood tests and medical imaging can be performed to rule out other possible causes of the symptoms.[2] Other conditions that share some symptoms of DLB include Alzheimer's disease (AD), Parkinson's disease, delirium and, rarely, psychosis.[9]
There is no cure or medication that will modify the progression of the disease.[2] Treatments aim to relieve some of its symptoms[3] and reduce the burden on caregivers.[8][13][14] Medications for one symptom may worsen another.[11] Acetylcholinesterase inhibitors (AChEI), such as donepezil, may provide some benefit, and melatonin can be used for sleep-related symptoms.[1] Antipsychotics, even for hallucinations, should be avoided because people with DLB are sensitive to them,[1] and their use can result in death.[15]
DLB is one of the three most common types of dementia, along with Alzheimer's disease and vascular dementia.[2][16][a] Together with Parkinson's disease dementia, it is one of two dementias classified as the Lewy body dementias.[10] It typically begins after the age of 50,[2] and about 0.4% of people over 65 are affected.[6] It is slightly more common in men than women.[11] In the latter stages of the disease, people with DLB may depend entirely on others for their care.[17] Life expectancy following diagnosis is about six years but may reach twenty years.[2] The abnormal deposits of protein that are the underlying mechanism of the disease were discovered in 1912 by Frederic Lewy, and DLB was first described by Kenji Kosaka in 1976.[7]
Classification
Dementia with Lewy bodies (DLB) is a progressive neurodegenerative dementia.[7] Together with Parkinson's disease dementia, it is one of the Lewy body dementias,[10] which are also classified as atypical parkinsonian syndromes.[6] It is one of the synucleinopathies—neurodegenerative diseases that are due to an abnormal accumulation of alpha-synuclein protein in the brain—along with Parkinson's disease, multiple system atrophy, and other more rare conditions.[18]
The Lewy body dementias are as a group the second most common form of dementia after Alzheimer's disease (AD).[11] DLB itself is one of the three most common types of dementia, along with AD and vascular dementia, with AD making up about half of all cases.[2][11][16][a]
Signs and symptoms
The alpha-synuclein protein deposits that cause DLB can lead to damage in different regions of the nervous system, including multiple brain regions in the central nervous system, as well as the autonomic nervous system,[19] and affect several domains of functioning,[b] resulting in a disease that is more complex than many other dementias, with widely varying symptoms.[15][17] The symptoms of DLB can be divided into essential, core, and supportive features.[7]
Essential features
Dementia is present, but does not always appear early on with DLB, and is more likely to present as the condition progresses,[1][8] typically after age 55.[10] According to the 2017 Fourth Consensus Report of the DLB Consortium, dementia is diagnosed when there is a "progressive cognitive decline of sufficient magnitude to interfere with normal social or occupational functions, or with usual daily activities".[1]
Memory loss is not always noticeable early on.[9] In contrast to AD, in which episodic memory loss related to encoding of memories is typically the earliest symptom,[20] memory impairment occurs later in the progression of DLB, verbal memory is not as severely affected, and deterioration in memory function is related to retrieval rather than encoding of new memories.[10][20]
Core features
While the specific symptoms may vary, core features—based on "diagnostic specificity and the volume of good-quality evidence available"[1]—designated by the 2017 DLB Consortium are:[1]
- fluctuating cognition, alertness or attention;
- REM sleep behavior disorder (RBD);
- "spontaneous cardinal features of parkinsonism"; and
- repeated visual hallucinations.[1]
In other severe cases of dementia (for example, advanced stages of AD), core features of DLB may also be present.[11]
Cognition, alertness or attention fluctuate throughout the day and these fluctuations are often present early in the course of the disease.[1][10] Impaired attention, executive function, and visuospatial function are common symptoms.[10] Karantzoulis and Galvin (2011) write that "marked attentional and executive function disturbance is central" and "attentional disturbance may serve as the basis of fluctuating cognition that is characteristic".[20] Problems with executive function surface in activities requiring planning and organizing.[6] These deficits can present with impaired job performance, difficulty multitasking, inability to follow conversations, or problems driving a car—such as becoming lost or misjudging distances.[10] Individuals with DLB may be easily distracted, and have a hard time focusing on tasks,[20] or appear to be "delirium-like", "zoning out", or in states of altered consciousness.[1] They may also exhibit disorganized speech and changing ability to organize their thoughts during the day.[1][10] A person with DLB may experience problems of wakefulness or sleep disorders including daytime sleepiness, drowsiness or napping more than two hours a day, insomnia, and restless legs syndrome.[2]
and dementia with Lewy bodies
"REM sleep behavior disorder (RBD) has been studied more thoroughly in correlation with DLB and is now considered a core feature. ... Basically, dementia in the presence of polysomnogram-confirmed RBD suggests possible DLB."
—B. Tousi (2017), Diagnosis and Management of Cognitive and Behavioral Changes in Dementia With Lewy Bodies.[9]
REM sleep behavior disorder is a parasomnia that occurs frequently in DLB and may appear decades before any other symptoms, often as the first clinical indication of DLB and an early sign of a synucleinopathy.[5] Individuals with RBD lose the paralysis of muscles (atonia) that is normal during rapid eye movement (REM) sleep, and act out their dreams or have other abnormal movements or vocalizations.[8] The individual with RBD may not be aware that they act out their dreams;[5] a bed partner may be the only person who knows of these behaviors.[2]
RBD behaviors may include yelling, screaming, laughing, crying, unintelligible talking,[5] non-violent flailing or more violent punching, kicking,[11] choking or scratching. People with RBD may fall out of bed,[5] or injure themselves or their bed partner,[15] often with limb movements.[1] There may be resulting bruises or fractures, and more serious injuries like subdural hematoma.[8] The reported dream enactment behaviors are frequently violent,[10] and involve a theme of being chased or attacked.[15] However, because people are more likely to remember or report violent dreams and behaviors, and to be referred to a specialist when injury occurs, recall or selection bias may explain the prevalence of violence reported in RBD.[5]
About 80% of people with DLB have RBD.[5] Abnormal sleep behaviors may begin before cognitive decline is observed in DLB.[1] On autopsy, 94 to 98% of individuals with polysomnography-confirmed RBD are found to have a synucleinopathy[8][14][21]—most commonly DLB or Parkinson's disease—that develops within 15 years,[11] and sometimes as long as 50 years after RBD.[8] RBD may subside over time.[1]
Parkinsonism occurs in more than 85% of people with DLB, who may have one or more of the cardinal features that occur in Parkinson's disease—slowness of movement, rigidity,[1] and less commonly, tremor at rest.[10] Motor symptoms may include shuffling gait, problems with balance, falls, blank expression (reduced range of facial expression), low speech volume or a weak voice and difficulty swallowing.[2] Presentation of motor symptoms is variable, but they are usually symmetric, presenting on both sides of the body.[10] For a DLB diagnosis, only one of the cardinal symptoms of parkinsonism need be present,[1] and they may be less severe than in persons with Parkinson's disease.[9]
Visual hallucinations are defined by Pezzoli, et al (2017) as "well-formed images perceived without the presence of real stimuli".[22] Up to 80% of people with DLB have visual hallucinations.[1] early in the course of DLB.[23] They are recurrent,[22] frequent,[23] and usually involve animated perceptions of animals or people, including children and family members.[10] They may be scenic, elaborate and detailed.[23]
These hallucinations can sometimes provoke fear, although their content is more typically neutral.[10] They are not necessarily disturbing, and in some cases, the person with DLB may be conscious they are not real,[14] and have insight about the hallucinations.[23] In individuals with more disrupted cognition, the hallucinations can become more complex, and they may be less aware that their hallucinations are not real.[22] Individuals with visual hallucinations and either of the two Lewy body dementias have more cognitive impairment, and those cognitive deficits are predictive of hallucinations.[22]
Different than visual hallucinations, but also common in DLB, are visual misperceptions or illusions, explained by Pezzoli (2017) as "incorrect perceptions of real stimuli".[22] The viewer with DLB may have problems with vision (for example, at night) and misinterpret what they see (for example, mistaking a pile of socks for snakes or a clothes closet for the bathroom).[10]
Supportive features
According to the DLB Consortium, "[a]lthough carrying less diagnostic weight, supportive items are often valuable in clinical decision-making, acting as signposts to or adding evidence for a DLB diagnosis."[1] Supportive features may persist over time, be present early in the progression of DLB, and are common, but they are not specific to the diagnosis.[1] The supportive features are:
- marked sensitivity to antipsychotics;
- marked dysautonomia (autonomic dysfunction) in which the autonomic nervous system does not work properly;
- hallucinations in senses other than vision (hearing, touch, taste and smell[9]);
- hypersomnia (excessive sleepiness);
- hyposmia (reduced ability to smell);
- false beliefs and delusions organized around a common theme;
- postural instability, loss of consciousness and frequent falls;
- apathy, anxiety or depression.[1][7]

Severe sensitivity to antipsychotics. Antipsychotic treatment of people with DLB results in adverse reactions about half of the time,[11] and this can be fatal after a single dose.[14] The Fourth Consensus Report continues to caution against the use of antipsychotics (neuroleptics) for people with DLB.[1] Partly because of dopamine cell loss, people with DLB may have neuroleptic malignant syndrome, impairments in cognition or alertness, or irreversible exacerbation of parkinsonism including severe rigidity,[10] and dysautonomia from the use of antipsychotics.[14]
Antipsychotic medications that should be used with great caution, if at all, for people with DLB include chlorpromazine,[24] haloperidol, olanzapine, risperidone, thioridazine, and injectable antipsychotics.[14]
Dysautonomia (or autonomic dysfunction) occurs in the synucleinopathies because Lewy pathology can also affect the peripheral autonomic nervous system and the nerves that serve organs including the intestines, heart, and urinary tract.[19] The first signs of autonomic dysfunction are often subtle in all synucleinopathies.[5] These symptoms can include poorly regulated body temperature and blood pressure,[2] including dizziness after quickly standing up,[15] loss of sense of smell or reduced ability to smell,[9][5] problems with constipation[15] and urination,[10] and excessive sweating or drooling.[9]
Among the other supportive features, psychiatric symptoms are more likely to cause more impairment, when compared to AD, and to be present when the individual first comes to clinical attention.[20] Anxiety affects 27% and depression affects 59% of people with DLB;[15] these symptoms are more common in DLB than in the general population,[11] and may have been present for decades.[15] Anxiety leads to increased risk of falls.[9] Apathy may lead to less social interaction.[2]
Agitation, behavioral disturbances,[15] and delusions may appear later in the course of the disease.[10] Delusions may have a paranoid quality, revolving around themes like a house being broken in to, infidelity,[10] or abandonment.[9] As the individual with DLB misplaces items, they may have delusions centered around theft.[10] Capgras delusion may occur, where the person with DLB loses knowledge of the spouse, caregiver or partner's face,[23] and is convinced that an imposter has replaced their caregiver.[10] Hallucinations in other modalities may be present, but are less frequent.[9]
Sleep disorders are common in DLB (and may lead to hypersomnia); these include disrupted sleep cycles, sleep apnea, and arousal from periodic limb movement disorder.[11] Loss of sense of smell may occur several years before other symptoms.[10]
Medications (including tricyclic antidepressants as well as treatments for urinary incontinence) with anticholinergic properties that cross the blood brain barrier can cause memory loss,[25] dopamine agonists may lead to psychosis,[25] benzodiazepines may exacerbate confusion[10] or neuropsychiatric symptoms,[14] and the antihistamine medication diphenhydramine (Benadryl) or sleep medications like zolpidem may worsen confusion.[25] General anesthetics may cause confusion or delirium upon waking, and may result in permanent mental impairment.[2]
Causes

The exact cause is unknown,[2] and is probably multifactorial.[11] The genetics are "vastly understudied", because the large homogeneous DLB populations that would be needed for genetic studies have not been identified.[7] Typically the disease is not seen clustered in families, although having another family member with DLB is a risk factor, leading to the belief that DLB does not result from simple genetic alterations.[2][7]
Genetics, however, are likely to play a role; DLB is not considered a purely genetic disease, but there is a genetic association in a small number of families.[2] DLB risk is heightened with inheritance of the ε4 allele of the apolipoprotein E (APOE) gene,[7] and mutations in the PARK11 and GBA genes are associated with DLB.[12] Further, there is genetic overlap between dementia with Lewy bodies, Parkinson's disease, and Alzheimer's.[7][11] Also, RBD is found more often among individuals who have GBA and SNCA mutations.[7]
The greatest risk factor is age (over 50); other risk factors include having Parkinson's disease or REM sleep behavior disorder, and having an unhealthy lifestyle, which is known to contribute to dementia.[2]
Pathophysiology

The precise mechanisms contributing to DLB are not well understood, and a matter of some dispute.[7]
DLB is characterized by the development of abnormal collections of alpha-synuclein protein within neurons, known as Lewy bodies and Lewy neurites.[11][12] When these clumps of protein form in neurons, those neurons function less optimally and die.[17] Damage in the brain is widespread, and affects many domains of functioning.[17][b] In DLB, loss of acetylcholine-producing neurons is thought to account for degeneration in memory and learning, while the death of dopamine-producing neurons appears to be responsible for degeneration of "behavior, cognition, movement, motivation, sleep, and mood".[2]
The role played by the the alpha-synucleins is still unclear, because individuals with no signs of DLB have been found on autopsy to have advanced alpha-synuclein pathology.[11] It is not known if the pathology spreads between cells or follows another pattern.[7] The mechanisms that contribute to cell death, how the disease advances through the brain, and the timing of cognitive decline are all poorly understood; nor is there a model to account for the specific neurons and brain regions that are affected.[7]
A proposed pathophysiology for RBD implicates cells in the reticular formation that regulate REM sleep, which are affected earlier than other brain regions in the Lewy body dementias; this could be a potential explanation for the earlier appearance of RBD (often decades) than other symptoms.[11]
Diagnosis
Dementia with Lewy bodies can only be definitively diagnosed after death with an autopsy of the brain,[2] so diagnosis of the living is referred to as probable or possible.[1] DLB is often misdiagnosed or confused in its early stages with Alzheimer's disease.[9] Another complicating factor is that DLB can occur along with Parkinson's or Alzheimer's diseases;[2] in research settings, autopsy may reveal previously undiagnosed Lewy bodies in as many as half of people with AD.[1] Despite the difficulty in diagnosis, a prompt diagnosis is important because of the serious risks of sensitivity to certain neuroleptic (antipsychotic) medications and the need to inform both the person with DLB and the person's caregivers about potentially irreversible side effects of those medications.[10] In comparison to many other neurodegenerative diseases, the management of DLB is difficult, so an accurate diagnosis is important.[15]
Criteria
The 2017 Fourth Consensus Report established diagnostic criteria for probable and possible DLB, in recognition of advances in detection and improvements from the earlier Third Consensus (2005)[27] version. The 2017 criteria are based on essential, core and supportive clinical features, and diagnostic biomarkers.[1]
The essential feature is dementia; for a DLB diagnosis, it must be sufficient to interfere with social or occupational functioning.[1] Dementia is diagnosed based on the person's medical history, physical exam, and assessment of neurological function, and by ruling out conditions that may cause similar symptoms.[28]
The core clinical features (described in the Signs and symptoms section) are: fluctuating cognition, visual hallucinations, REM sleep behavior disorder, and signs of parkinsonism.[1] Supportive clinical features are marked sensitivity to antipsychotics; marked dysautonomia autonomic dysfunction; non-visual hallucinations; hypersomnia; hyposmia; false beliefs and delusions organized around a common theme; "postural instability", loss of consciousness and frequent falls; apathy, anxiety or depression.[1][7]

The diagnostic biomarkers are:[1]
Indicative
- PET or SPECT showing reduced dopamine transporter uptake in the basal ganglia;
- abnormal myocardial MIBG scintigraphy;
- REM sleep without atonia evidenced on polysomnography; and
Supportive from PET, SPECT, CT, MRI or EEG brain studies showing:[1][7]
- lack of damage to medial temporal lobe;
- reduced occipital activity; or
- prominent slow-wave activity.
Probable DLB can be diagnosed when dementia and at least two core features are present, or one core feature with at least one indicative biomarker is present.[1] Possible DLB can be diagnosed when dementia and only one core feature is present or if no core features are present, there is at least one indicative biomarker.[1]
DLB bodies is distinguished from Parkinson's disease dementia by the time frame in which dementia symptoms appear relative to Parkinson symptoms.[1] DLB is diagnosed when cognitive symptoms begin before or at the same time as parkinsonism.[1] Parkinson's disease dementia would be the diagnosis when Parkinson's disease is well established before the dementia occurs;[1] that is, typically (in a research setting) the onset of dementia is more than a year after the onset of parkinsonian symptoms.[1]
DLB is listed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) as "Major or mild neurocognitive disorder with Lewy bodies".[11] The differences between the DSM and DLB Consortium criteria are:
- the DSM does not include low dopamine transporter uptake as a supportive feature,[11] and
- there is unclear diagnostic weight assigned to biomarkers in the DSM.[11]
Clinical history and testing

Diagnostic tests can be used to establish some features of the condition and distinguish them from symptoms of other conditions; diagnosis may include the person's medical history and medical exam, testing to rule out other conditions, brain imaging, neuropsychological testing to assess cognitive function,[2] sleep studies, or myocardial scintigraphy.[1] Laboratory testing can rule out conditions like depression, abnormal thyroid function, or vitamin deficiencies that may cause symptoms similar to dementia.[28]
Dementia screening tests are the Mini-Mental State Examination[1][29] the Montreal Cognitive Assessment, and others.[9][c] For tests of attention, digit span, serial sevens, and spatial span can be used for simple screening, and the Revised Digit Symbol Subtest of the Wechsler Adult Intelligence Scale may show defects in attention that are characteristic of DLB.[30] The Frontal Assessment Battery, Stroop test and Wisconsin Card Sorting Test are used for tests of executive function, and there are many shorter screening instruments available.[31]
If DLB is suspected when parkinsonism and dementia are the only presenting features, PET or SPECT imaging may show reduced dopamine transporter activity. A DLB diagnosis may be warranted if other conditions with reduced dopamine transporter uptake can be ruled out.[1][10] Dopamine transporter imaging also helps distinguish between DLB and AD.[1] Myocardial MIBG scintigraphy is used in East Asia and Japan to differentiate between DLB and AD.[9]
RBD is diagnosed either by sleep study recording or, when sleep studies cannot be performed, by medical history and validated questionnaires.[1][8][d] Similar conditions (for example, severe sleep apnea and periodic limb movement disorder) must be ruled out.[1] A prior history of violence or injury should be inquired about, as they increase the likelihood of future injurious dream enactment behaviors.[5] Individuals with RBD may not be able to provide a history of dream enactment behavior, so bed partners are also consulted.[1][5] The REM Sleep Behavior Disorder Single-Question Screen offers diagnostic sensitivity and specificity in the absence of polysomnography with one question:[8] "Have you ever been told, or suspected yourself, that you seem to 'act out your dreams' while asleep (for example, punching, flailing your arms in the air, making running movements, etc.)?"[9]
Differential
The cognitive and motor symptoms of many neurodegenerative conditions overlap with or can be confused with dementia with Lewy bodies. The differential diagnosis includes Alzheimer's disease; such synucleinopathies as Parkinson's disease dementia, Parkinson's disease, and multiple system atrophy; vascular dementia (multi-infarct dementia); and progressive supranuclear palsy, corticobasal degeneration, and corticobasal syndrome.[10] DLB may also be misdiagnosed as delirium[13] and, rarely, as psychosis.[9]
Lewy pathology can affect the peripheral autonomic nervous system, and autonomic dysfunction is a feature of DLB that is observed less often in Alzheimer's, frontotemporal, or vascular dementias, so its presence can help differentiate them.[32]
Alzheimer's disease. Short-term memory impairment is seen early in AD and is a prominent feature, while fluctuating attention is uncommon; impairment in DLB is more often seen earlier as fluctuating cognition.[10] While 74% of people with early DLB confirmed at autopsy have deficits in planning and organization, they show up in only 45% of people with AD.[11] In AD, it is unclear if executive function is impacted early.[20] Impairments in visuospatial processing are present in most individuals with DLB,[11] and they show up earlier and are more pronounced than in AD.[20] Hallucinations typically occur early in the course of DLB. They are less common in early AD, but usually occur later.[10][23]
PET or SPECT imaging can be used to detect reduced dopamine transporter uptake to distinguish AD and DLB.[10][33] Severe atrophy of the hippocampus is more typical of AD than DLB.[10] Other indicative and supportive biomarkers are useful in distinguishing DLB and AD (myocardial scintigraphy, preservation of medial temporal lobe structures, reduced occipital activity, and slow-wave EEG activity).[1]
Synucleinopathies. Dementia with Lewy bodies and Parkinson's disease dementia are clinically similar after dementia occurs in Parkinson's disease.[11] Delusions in Parkinson's disease dementia are less common than in DLB,[10] and persons with Parkinson's disease are typically less caught up in their visual hallucinations than those with DLB.[23] There is a lower incidence of tremor at rest in DLB than in Parkinson's disease, and signs of parkinsonism in DLB are more symmetrical.[5] In multiple system atrophy, autonomic dysfunction appears earlier and is more severe, and is accompanied by uncoordinated movements, while visual hallucinations and fluctuating cognition are less common than in DLB.[10]
Frontotemporal. Corticobasal syndrome, corticobasal degeneration and progressive supranuclear palsy are frontotemporal dementias[34] with features of parkinsonism and impaired cognition. Similar to DLB, imaging may show reduced dopamine transporter uptake. According to Gomperts (2016), "[c]areful history and examination remain the method of choice"[10] for distinguishing corticobasal syndrome and degeneration, and progressive supranuclear palsy, from DLB. Motor movements in corticobasal syndrome are asymmetrical. There are differences in posture, gaze and facial expressions in the most common variants of progressive supranuclear palsy, and falling backwards is more common relative to DLB. Visual hallucinations and fluctuating cognition are core features of DLB, but unusual in corticobasal syndrome and degeneration, and progressive supranuclear palsy.[10]
Vascular dementia. The Dementia Cognitive Fluctuation Scale is a screening questionnaire used to measure fluctuating attention and alertness that has shown promise in distinguishing between DLB and vascular dementia, but as of 2014, it had not been fully validated.[10]
Other. DLB may be commonly misdiagnosed as delirium[13] or more rarely as psychosis.[9] Mismanagement of delirium is a particular concern because of the risks to people with DLB associated with antipsychotics.[13] The symptoms of DLB are easily confused with delirium, and dopamine transporter imaging can help distinguish DLB from delirium.[13]
Management
Only palliative care can be offered,[7] as there are no medications which will modify the course of the disease.[12] No medications to treat DLB are approved by the United States Food and Drug Administration as of 2017,[9] although donepezil was licensed in 2014 in Japan for the treatment of DLB.[35] Management can be challenging because of the need to balance treatment of cognitive dysfunction, neuropsychiatric features, impairments related to the motor system,[10] and other nonmotor symptoms.[1] A multidisciplinary approach should go beyond early and accurate diagnosis to educating and supporting the caregivers.[1] Treatment modalities are divided into pharmaceutical and non-pharmaceutical,[10] but there is little systematic evidence for non-pharmaceutical approaches and more research is needed.[1][11][12]
Pharmaceutical
"The most fraught decision in the management of DLB relates to the use of antipsychotic medications ... DLB patients are particularly at risk of antipsychotic medication morbidity and mortality."
—B.P. Boot (2015), Comprehensive treatment of dementia with Lewy bodies[15]
Management of DLB is complicated by the wide range of symptoms to be treated (cognitive, motor, neuropsychiatric, autonomic, and sleep),[1][15] and adverse effects to medications in people with DLB.[11] Anticholinergic and dopaminergic agents can have adverse effects in individuals with DLB,[1] and a medication that addresses one feature might worsen another.[11] For example, acetylcholinesterase inhibitors (AChEIs) for cognitive symptoms can lead to complications in dysautonomia features; treatment of movement symptoms with dopaminergic agents may worsen neuropsychiatric symptoms; and treatment of hallucinations and psychosis with antipsychotics may worsen other symptoms or lead to a potentially fatal reaction.[15] Dopaminergic agonists and anticholinergics can result in psychosis.[1] All pharmaceutical management of DLB symptoms requires extra diligence.[11]
Extreme caution is required in the use of antipsychotic medication in people with DLB because of their sensitivity to these agents.[1] According to Boot (2013), "electing not to use neuroleptics is often the best course of action."[14] Due to hypersensitivity to neuroleptics, preventing people with Lewy body dementias from taking these medications is important. People with DLB are at risk for neuroleptic malignant syndrome, a life-threatening illness.[10] There is little evidence to support the use of antipsychotics to treat the Lewy body dementias, and they carry the additional risk of stroke when used in the elderly with dementia.[11]
Cognitive symptoms. There is strong evidence for the use of AChEIs as treatment for cognitive problems.[12] Even if the AChEIs donepezil (Aricept) and rivastigmine (Exelon) do not lead to improvement in cognitive symptoms, people taking them may have less deterioration,[1] although there may be adverse gastrointestinal effects.[11] DLB may be more responsive than AD to donepezil.[24] Memantine also may be useful; there is less evidence for its efficacy in DLB, but it may be used alone or with an AChEI because of its low side effect profile.[1] Anticholinergic drugs are avoided because they worsen cognitive symptoms.[11]
To improve daytime alertness, there is mixed evidence for the use of stimulants such as methylphenidate and dextromethamphetamine; they can increase the risk of psychosis, although worsening of neuropsychiatric symptoms is not common.[15][14] In the U.S., modafinil and armodafinil are not always covered by insurance, but may be effective for daytime sleepiness.[14][15]
Motor symptoms. Motor symptoms appear to respond in DLB somewhat less to the medications used to treat Parkinson's disease, like levodopa, and neuropsychiatric symptoms can be increased.[1] If such medications are needed for motor symptoms, cautious introduction with slow increases to the lowest possible dose may help avoid psychosis.[1]
Neuropsychiatric symptoms. The first line of defense in reducing visual hallucinations is to reduce the use of dopaminergic drugs, which can worsen hallucinations.[11] Although it has been shown effective in Parkinson's disease, there is limited evidence for the use of clozapine to treat visual hallucinations in DLB, and its use requires regular blood monitoring.[11] Quetiapine is relatively safe[1] and well-tolerated for psychosis and agitation in DLB, but there is little evidence for its efficacy.[11]
Apathy may be treated with AChEIs, and they may also reduce hallucinations and delusions;[1] reduction in anxiety and agitation may be a secondary effect.[1] Mirtazapine and SSRIs can be used to treat depression, depending on how well they are tolerated, and guided by general advice for the use of antidepressants in dementia.[1] Antidepressants can worsen RBD.[9] Antidepressants with anticholinergic properties may worsen hallucinations and delusions.[11] People with Capgras syndrome may not tolerate AChEIs.[9]
Sleep disorders. Injurious dream enactment behaviors are a treatment priority.[5] RBD may be treated with melatonin or clonazepam.[8] Melatonin may be more helpful in preventing injuries,[5] and it offers a safer alternative, because clonazepam can produce deteriorating cognition,[1] and worsen sleep apnea.[5] For some people, memantine or AChEIs are useful.[11] No trials support its use in DLB, but modafinil may be used for hypersomnia.[11] Mirtazapine can be used for hypersomnia, but it can exacerbate RBD.[11] Antidepressants (SSRIs, SSNRIs, tricyclics, and MAOIs), AChEIs, beta blockers, caffeine, and tramadol may worsen RBD.[5]
Autonomic symptoms. Decreasing the dosage of dopaminergic or neuroleptic drugs may be needed with orthostatic hypertension, and high blood pressure drugs can sometimes be stopped.[11]
Antihypotensive agents may help with fainting and other problems associated with orthostatic hypotension.[medical citation needed]
Non-pharmaceutical
For autonomic dysfunction, several non-medication strategies may be helpful. Dietary changes include avoiding sugary foods, eating smaller and more frequent meals,[36] and increasing table salt to reduce orthostatic hypotension, and increasing fluids or dietary fiber to treat constipation.[11] Physical exercise in a sitting or recumbent position, or exercise in a pool helps maintain conditioning when orthostatic hypotension is a problem.[36] Compression stockings and elevating the head of the bed may also help.[11] To lessen the risk of fractures in individuals with DLB who may be at risk for falls, bone mineral density screening and testing of vitamin D levels can be done,[1] and caregivers should be educated on the importance of preventing falls.[15] Physical therapy may be helpful for motor symptoms.[15]
Cognitive behavioral therapy can be tried for depression, although there is no evidence for its use in DLB.[11] It may also be tried for hallucinations.[12]
The frequency and severity of RBD may be lessened by treating sleep apnea, if it is present.[8]
Caregiving
Because of the neuropsychiatric symptoms associated with DLB, the demands placed on caregivers are higher than in AD,[13] but education for caregivers has not been studied as thoroughly as in AD.[1][12] Contributing factors to the caregiver burden in DLB are psychosis, aggression, agitation, and night-time behaviors such as parasomnias.[13] Caregivers of people with DLB may experience depression, exhaustion, and be in need of support.[13] Other family members who are not present in the daily caregiving may not observe all the fluctuating behaviors or recognize the stress on the caregiver; conflict can result when family members are not supportive.[2]
Visual hallucinations associated with DLB create a particular burden on caregivers,[37] so they should be educated on how to distract or change the subject when confronted with hallucinations rather than arguing over the reality of the hallucination.[14] Coping strategies may help and are worth trying, even though there is no evidence for their efficacy.[23] These strategies include having the person with DLB look away or look at something else, focus on or try to touch the hallucination, wait for it to go away on its own, and speak with others about the visualization.[23] Delusions and hallucinations may be reduced by increasing lighting in the evening, and making sure there is no light at night when the individual with DLB is sleeping.[14]
Caregivers and people with the condition should be educated about the increased risks of antipsychotics for people with DLB; if evaluation or treatment in an emergency room is needed, they may be able to explain that, in the words of Gomperts (2016) "patients with DLB are essentially 'allergic' to haloperidol and other neuroleptics".[10] Caregiver training, watchful waiting, identifying sources of pain, and increasing social interaction can help with agitation.[15]
When RBD is a problem, sleep-related injuries from falling or jumping out of bed can be avoided by placing a mattress next to the bed to soften the impact of a fall, and removing sharp objects from around the bed may help.[11] Sharp surfaces near the bed can be padded, and bed alarm systems may help with sleepwalking.[8] Bed partners may be advised to sleep in another room, and firearms should not be kept in the bedroom.[8] A home safety assessment can be done for when there is risk of falling.[1]
Prognosis
The prognosis for DLB has not been well studied; early studies had methodological limitations, such as small sample size and selection bias.[13] Compared to AD, which is better studied, memory is retained longer, while verbal fluency may be lost faster.[13] There are more neuropsychiatric symptoms, and they may emerge earlier, in DLB than AD, so according to Mueller (2017) those with DLB "might have a less favourable prognosis, with accelerated cognitive decline, shorter lifespan, and increased admission to residential care", although studies are conflicting.[13] Data suggest that admissions to hospital and time in nursing care may be higher than in AD; the difference may be explained by the presence of hallucinations.[13]
Prognosis varies depending on the individual, but depending on age and overall health,[2] generally DLB will lead to a decrease in life expectancy and quality of life (QOL), with increased disability and costs of care.[13] Depression, apathy, and visual hallucinations contribute to reduced QOL.[13] Decline may be more rapid when severe visuospatial deficits show up early in the course of the Lewy body dementias,[11] when the APOE gene is present, or when AD is also present.[13] The severity of orthostatic hypertension also predicts a worse prognosis.[15]
In the late part of the disease, people may depend entirely on others for their care.[17] Life expectancy is difficult to predict, and limited study data is available;[13] people with DLB typically live five to seven years following diagnosis, though some people live with DLB for twenty years.[2] Shorter life expectancy is more likely when visual hallucinations, abnormal gait, and variable cognition are present early on.[13] Aspiration pneumonia, a complication of difficulty in swallowing that results from dysautonomia, commonly causes death among people with synucleinopathies.[36]
Epidemiology
Dementia with Lewy bodies is under-recognized,[11] partly because the old diagnostic criteria (prior to 2017) were highly specific to DLB but not very sensitive, so many diagnoses were missed.[14]
About 0.4% of those over the age 65 are affected with DLB,[6] and about 1 per 1,000 people newly develop the condition each year.[38] DLB is slightly more common in men than women.[11] Symptoms usually appear between the ages of 50 and 80,[6] and it is not uncommon for it to be diagnosed before the age of 65.[11] An estimated 10 to 15% of diagnosed dementias are Lewy body type, but estimates range as high as 24%.[11]
DLB affects more than one million individuals in the United States.[2]
History
Frederic Lewy (1885–1950) was the first to discover the abnormal protein deposits (later called "Lewy body inclusions") in the early 1900s.[10][39] In 1912, studying Parkinson's disease (paralysis agitans),[40] he described findings of these inclusions in the vagus nerve, the nucleus basalis of Meynert and other brain regions.[41] He published a book, The Study on Muscle Tone and Movement. Including Systematic Investigations on the Clinic, Physiology, Pathology, and Pathogenesis of Paralysis agitans, in 1923 and except for one brief paper a year later, never mentioned his findings again.[42]
In 1961, Okazaki et al published an account of diffuse Lewy-type inclusions associated with dementia.[10] Dementia with Lewy bodies was first described in an autopsied case by Japanese psychiatrist and neuropathologist Kenji Kosaka in 1976;[7][43] he first proposed the term Lewy body disease four years later.[9] DLB was thought to be rare until it became easier to diagnose in the 1980s after the discovery of alpha-synuclein immunostaining that highlighted Lewy bodies in post mortem brains.[10] Kosaka et al described thirty-four more cases in 1984, which were mentioned along with four UK cases by Gibb et al in 1987 in the journal Brain, bringing attention of the Japanese work to the Western world.[44] A year later, Burkhardt et al published the first general description of diffuse Lewy Body Disease.[45]
With U.S., U.K. and Japanese researchers finding in the 1990s that DLB was a common dementia, there were nonetheless no diagnostic guidelines, and each group was using different terminology.[46] The DLB Consortium was established, and in 1996, the first criteria for diagnosing DLB were elaborated.[9] Between 1995 and 2005, the Consortium issued three Consensus Reports on DLB.[47] DLB was included in the fourth text revision of the DSM (DSM-IV-TR, published in 2000) under "Dementia due to other general medical conditions”. In the 2010s, the possibility of a genetic basis began to emerge.[7] The Fourth Consensus Report was issued in 2017, giving increased diagnostic weighting to RBD.[1]
Society and culture

Robin Williams, the American actor and comedian, died by suicide on August 11, 2014. He had been diagnosed with Parkinson's disease,[48] and according to his wife he experienced depression, anxiety and increasing paranoia.[49] Upon autopsy his wife said he was found to have diffuse DLB.[50] Ian McKeith, a dementia researcher and professor of Old Age Psychiatry at Newcastle University, commented that DLB was still too little known, and that Williams' symptoms were explained by DLB.[51]
The British author and poet Mervyn Peake died in 1968 and was diagnosed posthumously as a probable case of DLB in a 2003 study published in JAMA Neurology.[52] Sahlas (2003) said his death was "variously ascribed to Alzheimer disease, Parkinson disease, or postencephalitic parkinsonism".[52] Based on signs in his work and letters of progressive deterioration, fluctuating cognitive decline, deterioration in visuospatial function, declining attention span, and visual hallucinations and delusions, his may be the earliest known case where DLB was found to have been the likely cause of death.[52]
Other persons who had or died from DLB are Los Angeles Times publisher Otis Chandler;[53] and entertainers and artists including Estelle Getty, an actress known for her role in the television series The Golden Girls,[54] actress Dina Merrill,[55] Donald Featherstone, who created the plastic pink flamingo,[56] American radio and television host Casey Kasem,[57] and Canadian singer Pierre Lalonde.[58][59]
In the sports realm, Stan Mikita, Canadian ice hockey player,[60] and Jerry Sloan, American professional basketball player and coach,[61] have been diagnosed with DLB.
Research directions
Pimavanserin is approved by the U.S. Food and Drug Administration for treating psychosis in Parkinson's disease, and "holds promise"[15] in DLB, but as of 2017, there were no controlled studies of its use for psychosis in DLB.[9][12]
Cognitive training, deep brain stimulation and transcranial direct-current stimulation have been studied more in Parkinson's and Alzheimer's disease than they have in dementia with Lewy bodies, and all are potential therapies for DLB.[12]
Future strategies involve interventions to modify the course of the disease using immunotherapy, gene therapy, stem cell therapy, and reducing amyloid beta accumulation.[12] Identification of biomarkers for DLB will enable treatments to begin sooner[12] and improve the ability to select subjects and measure efficacy in clinical trials.[33] As of 2018 there were no well-validated neuroimaging modalities to measure alpha-synuclein in the brains of living people, but this was an active area of research.[33]
Notes
- ^ a b Kosaka (2017) writes: "Dementia with Lewy bodies (DLB) is now well known to be the second most frequent dementia following Alzheimer disease (AD). Of all types of dementia, AD is known to account for about 50%, DLB about 20% and vascular dementia (VD) about 15%. Thus, AD, DLB, and VD are now considered to be the three major dementias."[16] Walker (2015) states that an estimated 10 to 15% of diagnosed dementias are Lewy body type, but estimates range as high as 24%.[11] The NINDS (2017) says that Lewy body dementia "is one of the most common causes of dementia, after Alzheimer’s disease and vascular disease."[2]
- ^ a b Areas of the brain and function affected:[17]
- Cerebral cortex—thought, perception and language
- Limbic cortex—emotions and behavior
- Hippocampus—memory
- Midbrain and substantia nigra—movement
- Brainstem—sleep, alertness, and autonomic dysfunction
- Hypothalamus—autonomic dysfunction
- Olfactory cortex—smell.
- ^ Other dementia screening tests are the Parkinson's Disease Cognitive Rating Scale, Parkinson's Neuropsychometric Dementia Instrument, and Scales for Outcomes in Parkinson's Disease–Cognition.[9]
- ^ Questionnaires such as the REM Sleep Behavior Disorder Screening Questionnaire (RBDSQ), the REM Sleep Behavior Questionnaires – Hong-Kong (RBD-HK), the Mayo Sleep Questionnaire (MSQ), the Innsbruck REM Sleep Behavior Disorder Inventory, and the REM Sleep Behavior Disorder Single-Question Screen are well-validated.[5]
Sources
Kosaka K, ed. (2017). Dementia with Lewy bodies: clinical and biological aspects (1st ed.). Japan: Springer. doi:10.1007/978-4-431-55948-1. ISBN 978-4-431-55948-1.
References
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq br bs bt McKeith IG, Boeve BF, Dickson DW, et al. (July 2017). "Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium". Neurology (Review). 89 (1): 88–100. doi:10.1212/WNL.0000000000004058. PMC 5496518. PMID 28592453.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad "Lewy body dementia: Hope through research". National Institute of Neurological Disorders and Stroke. U.S. National Institutes of Health. December 8, 2017. Retrieved April 6, 2018.
- ^ a b c d "Dementia with Lewy bodies information page". National Institute of Neurological Disorders and Stroke. May 25, 2017. Retrieved April 7, 2018.
- ^ a b "Diagnosing Lewy body dementia". National Institute on Aging. U.S. National Institutes of Health. May 17, 2017. Retrieved April 6, 2018.
- ^ a b c d e f g h i j k l m n o p q r St Louis EK, Boeve AR, Boeve BF (May 2017). "REM sleep behavior disorder in Parkinson's disease and other synucleinopathies". Mov. Disord. (Review). 32 (5): 645–58. doi:10.1002/mds.27018. PMID 28513079.
- ^ a b c d e f Levin J, Kurz A, Arzberger T, Giese A, Höglinger GU (February 2016). "The differential diagnosis and treatment of atypical parkinsonism". Dtsch Arztebl Int (Review). 113 (5): 61–9. doi:10.3238/arztebl.2016.0061. PMC 4782269. PMID 26900156.
- ^ a b c d e f g h i j k l m n o p q r s Weil RS, Lashley TL, Bras J, Schrag AE, Schott JM (2017). "Current concepts and controversies in the pathogenesis of Parkinson's disease dementia and dementia with Lewy bodies". F1000Res (Review). 6: 1604. doi:10.12688/f1000research.11725.1. PMC 5580419. PMID 28928962.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g h i j k l m St Louis EK, Boeve BF (November 2017). "REM sleep behavior disorder: Diagnosis, clinical implications, and future directions". Mayo Clin. Proc. (Review). 92 (11): 1723–36. doi:10.1016/j.mayocp.2017.09.007. PMID 29101940.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x Tousi B (October 2017). "Diagnosis and management of cognitive and behavioral changes in dementia with Lewy bodies". Curr Treat Options Neurol (Review). 19 (11): 42. doi:10.1007/s11940-017-0478-x. PMID 28990131.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq Gomperts SN (April 2016). "Lewy body dementias: Dementia with Lewy bodies and Parkinson disease dementia". Continuum (Minneap Minn) (Review). 22 (2 Dementia): 435–63. doi:10.1212/CON.0000000000000309. PMC 5390937. PMID 27042903.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av Walker Z, Possin KL, Boeve BF, Aarsland D (October 2015). "Lewy body dementias". Lancet (Review). 386 (10004): 1683–97. doi:10.1016/S0140-6736(15)00462-6. PMC 5792067. PMID 26595642.
- ^ a b c d e f g h i j k l Velayudhan L, Ffytche D, Ballard C, Aarsland D (September 2017). "New therapeutic strategies for Lewy body dementias". Curr Neurol Neurosci Rep (Review). 17 (9): 68. doi:10.1007/s11910-017-0778-2. PMID 28741230.
- ^ a b c d e f g h i j k l m n o p q Mueller C, Ballard C, Corbett A, Aarsland D (May 2017). "The prognosis of dementia with Lewy bodies". Lancet Neurol (Review). 16 (5): 390–98. doi:10.1016/S1474-4422(17)30074-1. PMID 28342649.
- ^ a b c d e f g h i j k l m Boot BP, McDade EM, McGinnis SM, Boeve BF (December 2013). "Treatment of dementia with Lewy bodies". Curr Treat Options Neurol (Review). 15 (6): 738–64. doi:10.1007/s11940-013-0261-6. PMC 3913181. PMID 24222315.
- ^ a b c d e f g h i j k l m n o p q r s t Boot BP (2015). "Comprehensive treatment of dementia with Lewy bodies". Alzheimers Res Ther (Review). 7 (1): 45. doi:10.1186/s13195-015-0128-z. PMC 4448151. PMID 26029267.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c Kosaka K, ed. (2017), p. v.
- ^ a b c d e f "What is Lewy body dementia?". National Institute on Aging. U.S. National Institutes of Health. May 17, 2017. Retrieved April 7, 2018.
- ^ Goedert M, Jakes R, Spillantini MG (2017). "The synucleinopathies: Twenty years on". J Parkinsons Dis (Review). 7 (s1): S53–S71. doi:10.3233/JPD-179005. PMC 5345650. PMID 28282814.
- ^ a b Orimo S, Chapter 9 in Kosaka K, ed. (2017), pp. 111–12.
- ^ a b c d e f g Karantzoulis S, Galvin JE (November 2011). "Distinguishing Alzheimer's disease from other major forms of dementia". Expert Rev Neurother (Review). 11 (11): 1579–91. doi:10.1586/ern.11.155. PMC 3225285. PMID 22014137.
- ^ Boot BP (2015). "Comprehensive treatment of dementia with Lewy bodies". Alzheimers Res Ther (Review). 7 (1): 45. doi:10.1186/s13195-015-0128-z. PMC 4448151. PMID 26029267.
{{cite journal}}: Unknown parameter|lay-date=ignored (help); Unknown parameter|lay-source=ignored (help); Unknown parameter|lay-url=ignored (help)CS1 maint: unflagged free DOI (link) Original study here. - ^ a b c d e Pezzoli S, Cagnin A, Bandmann O, Venneri A (July 2017). "Structural and functional neuroimaging of visual hallucinations in Lewy body disease: A systematic literature review". Brain Sci (Review). 7 (7). doi:10.3390/brainsci7070084. PMC 5532597. PMID 28714891.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b c d e f g h i Burghaus L, Eggers C, Timmermann L, Fink GR, Diederich NJ (February 2012). "Hallucinations in neurodegenerative diseases". CNS Neurosci Ther (Review). 18 (2): 149–59. doi:10.1111/j.1755-5949.2011.00247.x. PMID 21592320.
- ^ a b Neef D, Walling AD (2006). "Dementia with Lewy bodies: an emerging disease". Am Fam Physician (Review). 73 (7): 1223–29. PMID 16623209. Archived from the original on June 6, 2011.
{{cite journal}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b c Gomperts SN (April 2016). "Lewy body dementias: Dementia with Lewy bodies and Parkinson disease dementia (Table 4-6)". Continuum (Minneap Minn) (Review). 22 (2 Dementia): 11. doi:10.1212/CON.0000000000000309. PMID 27042903.
- ^ Orimo S, Chapter 9 in Kosaka K, ed. (2017), p. 113.
- ^ McKeith IG, Dickson DW, Lowe J, et al. (December 2005). "Diagnosis and management of dementia with Lewy bodies: Third report of the DLB Consortium". Neurology. 65 (12): 1863–72. doi:10.1212/01.wnl.0000187889.17253.b1. PMID 16237129.
- ^ a b "Diagnosing dementia". National Institute on Aging. U.S. National Institutes of Health. May 17, 2017. Retrieved April 6, 2018.
{{cite web}}: Cite has empty unknown parameter:|1=(help) - ^ Mori E, Chapter 6 in Kosaka K, ed. (2017), p. 73.
- ^ Mori E, Chapter 6 in Kosaka K, ed. (2017), p. 74.
- ^ Mori E, Chapter 6 in Kosaka K, ed. (2017), pp. 75–76.
- ^ Orimo S, Chapter 9 in Kosaka K, ed. (2017), p. 112.
- ^ a b c Siderowf A, Aarsland D, Mollenhauer B, Goldman JG, Ravina B (April 2018). "Biomarkers for cognitive impairment in Lewy body disorders: Status and relevance for clinical trials". Mov. Disord. (Review). 33 (4): 528–36. doi:10.1002/mds.27355. PMID 29624752.
- ^ Finger EC (April 2016). "Frontotemporal dementias". Continuum (Minneap Minn). 22 (2 Dementia): 464–89. doi:10.1212/CON.0000000000000300. PMC 5390934. PMID 27042904.
- ^ Kosaka K, Chapter 1 in Kosaka K, ed. (2017), p. 7.
- ^ a b c Palma JA, Kaufmann H (March 2018). "Treatment of autonomic dysfunction in Parkinson disease and other synucleinopathies". Mov. Disord. (Review). 33 (3): 372–90. doi:10.1002/mds.27344. PMID 29508455.
- ^ Cheng ST (August 2017). "Dementia caregiver burden: a research update and critical analysis". Curr Psychiatry Rep (Review). 19 (9): 64. doi:10.1007/s11920-017-0818-2. PMC 5550537. PMID 28795386.
- ^ Hogan DB, Fiest KM, Roberts JI, et al. (April 2016). "The prevalence and incidence of dementia with Lewy bodies: a systematic review". Can J Neurol Sci (Review). 43 Suppl 1: S83–95. doi:10.1017/cjn.2016.2. PMID 27307129.
- ^ Kosaka K (2014). "Lewy body disease and dementia with Lewy bodies". Proc. Jpn. Acad., Ser. B, Phys. Biol. Sci. (Historical Review). 90 (8): 301–6. PMC 4275567. PMID 25311140.
- ^ Engelhardt E (October 2017). "Lafora and Trétiakoff: the naming of the inclusion bodies discovered by Lewy". Arq Neuropsiquiatr (Historical article). 75 (10): 751–753. doi:10.1590/0004-282X20170116. PMID 29166468.
- ^ Lewy F (1912). Paralysis agitans. I. Pathologische Anatomie In Handbuch der Neurologie, Vol 3, Lewandowsky M, Abelsdorff G, eds. Springer Verlag, Berlin, pp. 920–33. as cited in Goedert M, Jakes R, Spillantini MG (2017). "The synucleinopathies: Twenty years on". J Parkinsons Dis (Review). 7 (s1): S53–S71. doi:10.3233/JPD-179005. PMC 5345650. PMID 28282814.
- ^ Engelhardt E, Gomes M (2017). "Lewy and his inclusion bodies: Discovery and rejection". Dement Neuropsychol. 11 (2): 198–201. doi:10.1590/1980-57642016dn11-020012. PMC 5710688. PMID 29213511.
- ^ Kosaka K, Oyanagi S, Matsushita M, Hori A (1976). "Presenile dementia with Alzheimer-, Pick- and Lewy-body changes". Acta Neuropathol. 36 (3): 221–33. doi:10.1007/bf00685366. PMID 188300.
- ^ McKeith IG, Chapter 5 in Kosaka K, ed. (2017), p. 60.
- ^ McKeith IG, Chapter 5 in Kosaka K, ed. (2017), pp. 60–61.
- ^ McKeith IG, Chapter 5 in Kosaka K, ed. (2017), p. 63.
- ^ McKeith IG, Chapter 5 in Kosaka K, ed. (2017), pp. 64–67.
- ^ a b Gallman S (November 4, 2015). "Robin Williams' widow speaks: Depression didn't kill my husband". CNN. Archived from the original on April 11, 2015. Retrieved April 6, 2018.
{{cite news}}:|archive-date=/|archive-url=timestamp mismatch; November 4, 2015 suggested (help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ a b Williams SS (September 2016). "The terrorist inside my husband's brain". Neurology. 87 (13): 1308–11. doi:10.1212/WNL.0000000000003162. PMID 27672165.
- ^ Robbins R (September 30, 2016). "How Lewy body dementia gripped Robin Williams". Scientific American. Retrieved April 9, 2018.
- ^ McKeith, IG. "Robin Williams had dementia with Lewy bodies -- so, what is it and why has it been eclipsed by Alzheimer's?". The Conversation. Archived from the original on April 11, 2016. Retrieved April 6, 2018.
{{cite news}}:|archive-date=/|archive-url=timestamp mismatch; November 4, 2016 suggested (help); Unknown parameter|deadurl=ignored (|url-status=suggested) (help); Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ a b c Sahlas DJ (June 2003). "Dementia with Lewy bodies and the neurobehavioral decline of Mervyn Peake". Arch. Neurol. 60 (6): 889–92. doi:10.1001/archneur.60.6.889. PMID 12810496.
- ^ Shaw D, Landsberg M (February 27, 2006). "L.A. icon Otis Chandler dies at 78". The Los Angeles Times. Archived from the original on April 26, 2007. Retrieved July 23, 2008.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Carlson M (July 24, 2008). "Obituary: Estelle Getty". theguardian.com. Archived from the original on September 2, 2013. Retrieved October 13, 2013.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Dangremond S (May 23, 2017). "Actress and philanthropist Dina Merrill dies at 93". Town and Country Magazine. Retrieved March 22, 2018.
- ^ Woo E (June 24, 2015). "Don Featherstone dies at 79; creator of the plastic pink flamingo". Los Angeles Times. Retrieved March 22, 2018.
- ^ Caffrey J (April 18, 2016). "Casey Kasem and a lesson about end-of-life care". CNN. Retrieved March 22, 2018.
- ^ Papineau P (June 23, 2016). "L'idole d'une génération s'éteint" (in French). Le Devoir. Retrieved April 9, 2018.
- ^ Belanger C (June 22, 2016). "Pierre Lalonde souffrait aussi de la démence à corps de Lewy" (in French). Le Journal de Montréal. Retrieved March 22, 2018.
- ^ Kuc C (June 15, 2015). "For Stan Mikita, all the Blackhawks memories are gone". Chicago Tribune. Archived from the original on June 16, 2015. Retrieved March 22, 2018.
{{cite news}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) - ^ Wood B (April 6, 2016). "Utah doctor: Diagnosing Parkinson's, Lewy body dementia has improved, but cure remains out of reach". Salt Lake Tribune. Retrieved April 6, 2018.
External links
- Ferman TJ (2007). Behavioral challenges in dementia with Lewy bodies, from 'The many faces of Lewy body dementia' series at Coral Springs Medical Center, FL (Video). Lewy Body Dementia Association. Archived from the original on 2017-02-13.
{{cite AV media}}: Unknown parameter|deadurl=ignored (|url-status=suggested) (help) – Lewy Body Dementia Association conference video oriented towards caregivers - McKeith I (October 10, 2017). Updated diagnostic criteria and management of Lewy body dementia (Video). ALZForum co-hosted with Lewy Body Dementia Association. Retrieved April 8, 2018.
