Menstrual cycle
The menstrual cycle is a recurring cycle of physiological changes in the females of some animal species that is associated with reproductive fertility.
This article concentrates on the menstrual cycle as it occurs in human beings.
Overview
Only human beings and the great apes experience a true menstrual cycle. Most placental mammals experience estrous instead. The menstrual cycle is under the control of the reproductive hormone system and is necessary for reproduction. In women, menstrual cycles occur typically on a monthly basis between puberty and menopause.
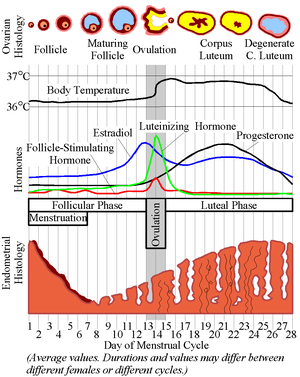
During the menstrual cycle, the sexually mature female body builds up the lining of the uterus with gradually increasing amounts of oestrogen, and when this hormone reaches a critical level, estradiol is produced, and shortly thereafterward there is the stimulation of the ovaries with Follicle Stimulating Hormone (FSH), and luteinizing hormone (LH). Follicles begin developing, and within a few days one "matures" into an ovum or egg. The ovary then releases this egg, (or occasionally two, which might result in dizygotic, or fraternal/non-identical, twins) at the time of ovulation. (Identical twins form from a single egg, as a result of the zygote splitting.) The lining of the uterus, the endometrium, peaks shortly there afterward in a synchronised fashion. After ovulation, this lining changes to prepare for potential conception and implantation of the fertilized egg to establish a pregnancy. The hormone progesterone rises after ovulation, and peaks shortly thereafter.
If fertilization and pregnancy do not ensue, the uterus sheds the lining, culminating with menstruation, which marks the low point for estrogen activity. This manifests itself to the outer world in the form of the menses (also menstruum): essentially part of the endometrium and blood products that pass out of the body through the vagina. Although this is commonly referred to as blood, it differs in composition from venous blood. Menstrual cycles are counted from the beginning of menstruation, because this is an outside sign that corresponds closely with the hormonal cycle. Menses, or bleeding and other menstrual signs may end at different points in the new cycle.
Common usage refers to menstruation and menses as a period. This bleeding serves as a sign that a woman has not become pregnant. (However, this cannot be taken as certainty, as sometimes there is some bleeding in early pregnancy.) During the reproductive years, failure to menstruate may provide the first indication to a woman that she may have become pregnant. A woman might say that her "period is late" when an expected menstruation has not started and she might have become pregnant.
Menstruation forms a normal part of a natural cyclic process occurring in healthy women between puberty and the end of the reproductive years. The onset of menstruation, known as menarche, occurs at an average age of 12, but is normal anywhere between 8 and 16. Factors such as heredity, diet and overall health can accelerate or delay the onset of menarche.[1]
The condition precocious puberty has caused menstruation to occur in girls as young as 8 months old.[2] Some women experience their first period in their late teens. The last period, menopause, usually occurs between the ages of 45 and 55. Deviations from this pattern deserve medical attention. Amenorrhea refers to a prolonged absence of menses during the reproductive years of a woman for reasons other than pregnancy. For example, women with very low body fat, such as athletes, may cease to menstruate. The presence of menstruation does not prove that ovulation took place; women who do not ovulate may have menstrual cycles. Those anovulatory cycles tend to take place less regularly and show greater variation in cycle length. In addition, the absence of menstruation also does not prove that fertilization did take place, because hormone disruptions in non-pregnant women can suppress bleeding on occasion.
The normal menstrual cycle in humans
Women show considerable variation in the lengths of their menstrual cycles, and the length of the menstrual cycle differs in different animals (see below).
While cycle length may vary, 28 days is generally taken as representative of the average ovulatory cycle in women. Convention uses the onset of menstrual bleeding to mark the beginning of the cycle, so the first day of bleeding is called "Cycle Day one".
One can divide the menstrual cycle into four phases:
Menstruation
Eumenorrhea denotes normal, regular menstruation that lasts for a few days (usually 3 to 5 days, but anywhere from 2 to 7 days is considered normal.[3] The average blood loss during menstruation is 35 millilitres with 10-80 mL considered normal;[4] many women also notice shed endometrium lining that appears as tissue mixed with the blood. An enzyme called plasmin — contained in the endometrium — tends to inhibit the blood from clotting. Because of this blood loss, women have higher dietary requirements for iron than do males to prevent iron deficiency. Many women experience uterine cramps, also referred to as dysmenorrhea, during this time. A vast industry has grown to provide sanitary products to help women to manage their menses.
Follicular phase
Through the influence of a rise in Follicle stimulating hormone (FSH), five to seven tertiary-stage ovarian follicles are recruited for entry into the menstrual cycle. These follicles, that have been growing for the better part of a year in a process known as folliculogenesis, compete with each other for dominance. In a signal cascade kicked off by luteinizing hormone (LH), the follicles secrete estradiol, a steroid that acts to inhibit pituitary secretion of FSH. With diminished FSH supply comes a slowing in growth that eventually leads to follicle death, known as atresia. The largest follicle secretes inhibin that serves as a finishing blow to less competent follicles by further suppressing FSH. This dominant follicle continues growing, forms a bulge near the surface of the ovary, and soon becomes competent to ovulate.
The follicles also secrete estrogens (of which estradiol is a member). Estrogens initiate the formation of a new layer of endometrium in the uterus, histologically identified as the proliferative endometrium. If fertilized, the embryo will implant itself within this hospitable flesh.
Ovulation

When the follicle has matured, it secretes enough estradiol to trigger the acute release of luteinizing hormone (LH). In the average cycle this LH surge starts around cycle day 12 and may last 48 hours. The release of LH matures the egg and weakens the wall of the follicle in the ovary. This process leads to ovulation: the release of the now mature ovum, the largest cell of the body (with a diameter of about 0.5 mm). Which of the two ovaries — left or right — ovulates appears essentially random; no known left/right co-ordination exists. The Fallopian tube needs to capture the egg and provide the site for fertilization. A characteristic clear and stringy mucus exhibiting spinnbarkeit develops at the cervix, ready to accept sperm from intercourse. In some women, ovulation features a characteristic pain called Mittelschmerz (German term meaning 'middle pain') which lasts for several hours. The sudden change in hormones at the time of ovulation also causes light mid-cycle bleeding for some women. Many women perceive the vaginal and cervical mucus changes at ovulation, particularly if they are monitoring themselves for signs of fertility. An unfertilized egg will eventually disintegrate or dissolve in the uterus. Scientific investigations have indicated that the olfactory acuity or the sense of smell is greatest during ovulation in women.[5]
Luteal phase
The corpus luteum is the solid body formed in the ovaries after the egg has been released from the fallopian tube which continues to grow and divide for a while. After ovulation, the residual follicle transforms into the corpus luteum under the support of the pituitary hormones. This corpus luteum will produce progesterone in addition to estrogens for approximately the next 2 weeks. Progesterone plays a vital role in converting the proliferative endometrium into a secretory lining receptive for implantation and supportive of the early pregnancy. It raises the body temperature by one-half to one degree Fahrenheit (one-quarter to one-half degree Celsius), thus women who record their temperature on a daily basis will notice that they have entered the luteal phase. If fertilization of an egg has occurred, it will travel as an early blastocyst through the fallopian tube to the uterine cavity and implant itself 6 to 12 days after ovulation. Shortly after implantation, the growing embryo will signal its existence to the maternal system. One very early signal consists of human chorionic gonadotropin (hCG), a hormone that pregnancy tests can measure. This signal has an important role in maintaining the corpus luteum and enabling it to continue to produce progesterone. In the absence of a pregnancy and without hCG, the corpus luteum demises and inhibin and progesterone levels fall. This will set the stage for the next cycle. Progesterone withdrawal leads to menstrual shedding (progesterone withdrawal bleeding), and falling inhibin levels allow FSH levels to rise to raise a new crop of follicles.
Physical experience of menstruation
In many women, various intense sensations brought about by the involved hormones and by cramping of the uterus can precede or accompany menstruation. Stronger sensations may include significant menstrual pain (dysmenorrhea), abdominal pain, migraine headaches, depression and emotional sensitivity, and changes in sex drive. Diarrhea or loose stools are common for the first few days of a woman's period.[citation needed] Breast discomfort caused by premenstrual water retention is very common. The sensations experienced vary from woman to woman and from cycle to cycle.
The fertile window
The length of the follicular phase — and consequently the length of the menstrual cycle — may vary widely. The luteal phase, however, almost always takes the same number of days. Some women have a luteal phase of 10 days, others of 16 days (the average is 14 days), but for each individual woman, this length will remain constant. Sperm survive inside a woman for 3 days on average, with survival time up to five days considered normal. A pregnancy resulting from sperm life of eight days has been documented.[6][7][8] The most fertile period (the time with the highest likelihood of sexual intercourse leading to pregnancy) covers the time from some 5 days before ovulation until 1-2 days after ovulation. In an average 28 day cycle with a 14-day luteal phase, this corresponds to the second and the beginning of the third week of the cycle. Fertility awareness methods of birth control attempt to determine the precise time of ovulation in order to find the relatively fertile and the relatively infertile days in the cycle.
People who have heard about the menstrual cycle and ovulation may commonly and mistakenly assume, for contraceptive purposes, that menstrual cycles always take a regular 28 days, and that ovulation always occurs 14 days after beginning of the menses. This assumption may lead to unintended pregnancies. Note too that not every bleeding event counts as a menstruation, and this can mislead people in their calculation of the fertile window.
If a woman wants to conceive, the most fertile time occurs between 19 and 10 days prior to the expected menses. Many women use ovulation detection kits that detect the presence of the LH surge in the urine to indicate the most fertile time. Other ovulation detection systems rely on observation of one or more of the three primary fertility signs (basal body temperature, cervical fluid, and cervical position).
Among women living closely together, the onsets of menstruation may tend to synchronise somewhat. This McClintock effect was first described in 1971, and possibly explained by the action of pheromones in 1998.[9] However, subsequent research has called this conclusion into question.
Hormonal control
Extreme intricacies regulate the menstrual cycle. For many years, researchers have argued over which regulatory system has ultimate control: the hypothalamus, the pituitary, or the ovary with its growing follicle; but all three systems have to interact. In any scenario, the growing follicle has a critical role: it matures the lining, provides the appropriate feedback to the hypothalamus and pituitary, and modifies the mucus changes at the cervix. Two sex hormones play a role in the control of the menstrual cycle: estradiol and progesterone. While estrogen peaks twice, during follicular growth and during the luteal phase, progesterone remains virtually absent prior to ovulation, but becomes critical in the luteal phase and during pregnancy. Many tests for ovulation check for the presence of progesterone. These sex hormones come under the influence of the pituitary gland, and both FSH and LH play necessary roles. FSH stimulates immature follicles in the ovaries to grow. LH triggers ovulation. The gonadotropin-releasing hormone of the hypothalamus controls the pituitary, yet both the pituitary and the hypothalamus receive feedback from the follicle. After ovulation the corpus luteum — which develops from the burst follicle and remains in the ovary — secretes both estradiol and progesterone. Only if pregnancy occurs do hormones appear in order to suspend the menstrual cycle, while production of estradiol and progesterone continues. Abnormal hormonal regulation leads to disturbance in the menstrual cycle.
Some women with neurological conditions experience increased activity of their conditions at about the same time every month. 80 percent of women with epilepsy have more seizures than usual in the phase of their cycle when progresterone declines and estrogen increases.
Mice have been used as an experimental system to investigate possible mechanisms by which levels of sex steroid hormones might regulate nervous system function. During the part of the mouse estrous cycle when progesterone is highest, the level of nerve-cell GABA receptor subtype delta was high. Since these GABA receptors are inhibitory, nerve cells with more delta receptors are less likely to fire than cells with lower numbers of delta receptors. During the part of the mouse estrous cycle when estrogen levels are higher than progesterone levels, the number of delta receptors decrease, increasing nerve cell activity, in turn increasing anxiety and seizure susceptibility.[10]
Hidden ovulation
Unlike almost all other species, the external physical changes of a human female near ovulation are very subtle. A woman may sense her own ovulation while it may remain indiscernible to others; this is considered to have sociobiological significance. In contrast, other species often signal receptivity through heat. The great apes are the only other mammals to have hidden ovulation.
The ovary as an egg-bank
Evidence suggests that eggs are formed from germ cells early in fetal life. The number is reduced to an estimated 400,000 to 450,000 immature eggs residing in each ovary at puberty. The menstrual cycle, as a biologic event, allows for ovulation of one egg typically each month. Thus over her lifetime a woman will ovulate approximately 400 to 450 times. All the other eggs dissolve by a process called atresia. As a woman's total egg supply is formed in fetal life, to be ovulated decades later, it has been suggested that this long lifetime may make the chromatin of eggs more vulnerable to division problems, breakage, and mutation than the chromatin of sperm, which are produced continuously during a man's reproductive life. This possibility is supported by the observation that fetuses and infants of older mothers have higher rates of chromosome abnormalities than those of older fathers.
The anovulatory menstrual cycle
Not all menstruations result from an ovulatory menstrual cycle (Anovulatory cycle - literally 'an-' absence of 'ovulation'). In some women, follicular development may start but not complete, nevertheless estrogens will form and will stimulate the uterine lining. Sooner or later the uterus will shed this lining. As no ovulation and no progesterone involvement occurs, doctors call this type of bleeding an estrogen breakthrough bleeding, and cannot always predict its duration or frequency. Anovulatory bleeding commonly occurs prior to menopause (premenopause) or in women with polycystic ovary syndrome. Infrequent or irregular ovulation is called oligoovulation.
Cycle abnormalities
Frequency
The "normal menstrual cycle" occurs every 28 days ± 7 days.
The medical term for cycles with intervals of 21 days or fewer is polymenorrhea and, on the other hand, the term for cycles with intervals exceeding 35 days is oligomenorrhea (or amenorrhea if intervals exceed 180 days).
Flow
The normal menstrual flow amounts to 50 mL ± 30 mL. It follows a "crescendo-decrescendo" pattern; that is, it starts at a moderate level, increases somewhat, and then slowly tapers. Sudden heavy flows or amounts in excess of 80 mL (hypermenorrhea or menorrhagia) may stem from hormonal disturbance, uterine abnormalities, including uterine leiomyoma or cancer, and other causes. Doctors call the opposite phenomenon, of bleeding very little, hypomenorrhea.
Duration
The typical woman bleeds for three to seven days at the beginning of each menstrual cycle.
Prolonged bleeding (metrorrhagia, also meno-metrorrhagia) no longer shows a clear interval pattern. Dysfunctional uterine bleeding refers to hormonally caused bleeding abnormalities, typically anovulation. All these bleeding abnormalities need medical attention; they may indicate hormone imbalances, uterine fibroids, or other problems. As pregnant patients may bleed, a pregnancy test forms part of the evaluation of abnormal bleeding.
Contraception and menstruation
Hormonal options
Estrogens and progesterone-like hormones make up the main active ingredients of birth control pills. Typically they tend to mimic a menstrual cycle in appearance, but to suppress the critical event of the ovulatory cycle, namely ovulation. Normally, a woman takes hormone pills for 21 days, followed by 7 days of non-functional sugar pills or no pills at all; then the cycle starts again. During the 7 placebo days, a withdrawal bleeding occurs; this differs from ordinary menstruation, and skipping the placebos and continuing with the next batch of hormone pills may suppress it. (Two main versions of the pill exist: monophasic and triphasic. With triphasic pills, skipping of the placebos and continuing with the next month's dose can make a woman more likely to experience spotting or breakthrough bleeding.) In 2003 the United States Food and Drug Administration (FDA) approved low-dose monophasic birth control pills which induce withdrawal bleedings only every 3 months. Yet another version of the pill is the recently-released Loestrin Fe, which has only a four-day placebo "week" (the placebos are actually iron supplements intended to replenish iron lost via bleeding), the other three placebos being replaced with active hormone pills; this system is intended to help shorten the duration of a period.
Other types of hormonal birth control which affect menstruation include the vaginal Nuvaring and the transdermal patch (like the standard pill pack: used for three weeks, then given a one-week break for bleeding) and the shot (which can eliminate bleeding for several months at a time).
Effects on menstruation
All such methods are designed to regulate monthly bleeding. Because of this, they are often chosen by females who wish to regulate the frequency and length of their period, often for basic convenience and especially when such factors are irregular and problematic on their own. Hormonal contraception has also been shown to improve menstrual factors such as cramping, heavy bleeding, and other bothersome physical and emotional issues related to periods.
Control and flexibility
Hormonal methods which are controlled by the user day-to-day, including pills, the ring, and the patch, need not always be used according to the standard cycle/calendar. Their use can be rescheduled and altered in various ways to postpone or skip periods when desired for reasons of convenience (e.g., traveling or scheduled gynecological exams), personal enjoyment (such as expected sexual encounters or events like a wedding or dance), or health (including very painful periods or sensitivity to hormone fluctuations). Similarly, abrupt cessation of use can induce a breakthrough period mid-cycle.
Other contraceptive methods
IUDs are not designed to affect menstruation or breakthrough bleeding, but may exacerbate cramps or the heaviness of the flow due to their placement within the uterus. Tubal sterilization alone will not affect menstruation, though the ablation option often performed at the same time will cease menstruation. Hysterectomy will, of course, completely stop menstruation as it entails the removal of the uterus (and sometimes related organs). Fertility awareness methods do not affect the period in and of themselves, but involve careful observation of various kinds, of which the timing of the period is an essential factor.
Etymology and the lunar month
The terms "menstruation" and "menses" come from the Latin mensis (month), which in turn relates to the Greek mene (moon) and to the roots of the English words month and moon — reflecting the fact that the moon also takes close to 28 days to revolve around the Earth (actually 27.32 days). The synodical lunar month, the period between two new moons (or full moons), is 29.53 days long.
A 1975 book by Louise Lacey documented the experience of herself and 27 of her friends, who found that when they removed all artificial nightlighting their menstrual cycles began to occur in rhythm with the lunar cycle. She dubbed the technique Lunaception.[11] Later studies in both humans[12] and animals[13] have found that artificial light at night does influence the menstrual cycle in humans and the estrus cycle in mice (cycles are more regular in the absence of artificial light at night), though none have duplicated the synchronization of women's menstrual cycles with the lunar cycle. One author has suggested that sensitivity of women's cycles to nightlighting is caused by nutritional deficiencies of certain vitamins and minerals.[14]
Some have suggested that the fact that other animals' menstrual cycles appear to be greatly different from lunar cycles is evidence that the average length of humans' cycle is most likely a coincidence.[15][16]
Menstrual products
While some women allow their menses to flow freely, most women prefer to use some external means to absorb or catch their menses to prevent soiling their clothes. There are a number of different methods available.
Disposable items:
- Sanitary napkins (Sanitary towels) or pads - Somewhat rectangular pieces of material worn in the underpants to absorb menstrual flow, often with "wings," pieces that fold around the panties, and/or an adhesive backing to hold the pad in place. Disposable synthetic pads are made of wood pulp or synthetic products, usually with a plastic lining and bleached. Some sanitary napkins, particularly older styles, are held in place by a belt-like apparatus, instead of adhesive or wings.
- Tampons - Disposable wads of treated rayon/cotton blends or all-cotton fleece, usually bleached, that are inserted into the vagina to absorb menstrual flow.
- Padettes - Disposable wads of treated rayon/cotton blend fleece that are placed within the inner labia to absorb menstrual flow.
- Disposable menstrual cups -- A firm, flexible cup-shaped device worn inside the vagina to catch menstrual flow. Disposable cups are made of soft plastic (like Instead).
Reusable items:
- Reusable cloth pads are made of cotton (often organic), terrycloth, or flannel, and may be handsewn (from material or reused old clothes and towels) or storebought.
- Menstrual cups - A firm, flexible bell-shaped device worn inside the vagina to catch menstrual flow. Reusable versions include rubber or silcone cups (like the Keeper, DivaCup, Lunette, and Mooncup).
- Sea sponges - Natural sponges, worn internally like a tampon to absorb menstrual flow.
- Padded panties - Reuseable cloth (usually cotton) underwear with extra absorbent layers sewn in to absorb flow. (like Lunapads)
- Blanket, towel - Large reuseable piece of cloth, most often used at night, placed between legs to absorb menstrual flow.
In addition to products to contain the menstrual flow, pharmaceutical companies likewise provide products — commonly non-steroidal anti-inflammatory drugs (NSAIDs) — to relieve menstrual cramps. Some herbs, such as dong quai, raspberry leaf and crampbark, are also claimed to relieve menstrual pain.[17]
Culture and menstruation
Many religions have menstruation-related traditions. These may be bans on certain actions during menstruation (such as intercourse in orthodox Judaism and Islam), or rituals to be performed at the end of each menses (such as the mikvah in Judaism and the ghusl in Islam).
Menstruation in other mammals
A regular menstrual cycle as described here only occurs in the great apes. Menstrual cycles vary in length from an average of 29 days in orangutans to an average of 37 days in chimpanzees.
Females of other mammalian species go through certain episodes called "estrus" or "heat" in each breeding season. During these times, ovulation occurs and females become receptive to mating, a fact advertised to males principally in some way presumably mediated by pheromones. If no fertilisation takes place, the uterus reabsorbs the endometrium: no menstrual bleeding occurs. Significant differences exist between the estrus and the menstrual cycle. Some animals, such as domestic cats and dogs do produce a very short and mild menstrual flow. However, due to its small amount (and personal cleanliness in cats) it passes pet owners largely unnoticed.
References
- Gangestad SW, Simpson JA, Cousins AJ, Garver-Apgar CE, Christensen PN (2004). "Women's preferences for male behavioral displays change across the menstrual cycle". Psychol Sci. 15 (3): 203–7. PMID 15016293.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
Notes
- ^ "At what age does a girl get her first period?," from Menstruation and the Menstrual Cycle, National Women's Health Information Center (accessed June 11, 2005)
- ^ Mikkelson, Barbara (2004-07-21). "Youngest Mother". Snopes.com. Retrieved 2006-07-02.
{{cite web}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ >The National Women's Health Information Center (November 2002). "What is a typical menstrual period like?". U.S. Department of Health and Human Services. Retrieved 2005-06-11.
{{cite web}}: CS1 maint: year (link) - ^ David L Healy (2004-11-24). "Menorrhagia Heavy Periods - Current Issues". Monash University. ABN 12 377 614 012.
{{cite web}}: CS1 maint: year (link) - ^ Navarrete-Palacios E, Hudson R, Reyes-Guerrero G, Guevara-Guzman R (2003). "Lower olfactory threshold during the ovulatory phase of the menstrual cycle". Biol Psychol. 63 (3): 269–79. PMID 12853171.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ball M (1976). "A prospective field trial of the "ovulation method" of avoiding conception". Eur J Obstet Gynecol Reprod Biol. 6 (2): 63–6. PMID 985763.
- ^ Dr Evelyn Billings & Ann Westmore (2005). "Trials of The Billings Ovulation Method". Retrieved 2005-11-03.
- ^ Sinha G, Sinha A (1993). "A field trial of Billings' ovulation method for spacing and limitation of birth". J Indian Med Assoc. 91 (10): 255–6. PMID 8308307.
- ^ Stern K, McClintock MK (1998). "Regulation of ovulation by human pheromones". Nature. 392 (6672): 177–9. PMID 9515961.
- ^ Maguire, J.L. . . . and I. Mody. (2005). "Ovarian cycle-linked changes in GABAA receptors mediating tonic inhibition alter seizure susceptibility and anxiety". Nature Neuroscience. 8 (June): 797–804.
{{cite journal}}: External link in|title= - ^ Lacey, Louise. Lunaception: A Feminine Odyssey into Fertility and Contraception. New York: Coward, McCann & Geoghegan, 1975.
- ^ Singer, Katie. "[http://www.westonaprice.org/women/fertility.html Fertility Awareness, Food, and Night-Lighting]". Wise Traditions in Food, Farming and the Healing Arts, Spring 2004. See section on Night-Lighting.
- ^ Harder, Ben. Bright nights kindle cancers in mice. Science News, Week of Aug. 28, 2004; Vol. 166, No. 9 , p. 141.
- ^ Shannon, Marilyn. Fertility, Cycles, and Nutrition. Cincinnati, Ohio: The Couple to Couple League International, 2001. pp. 71-72.
- ^ As cited by Adams, Cecil, "What's the link between the moon and menstruation?" (accessed 6 June 2006): Abell, George O. (1983). Science and the Paranormal: Probing the Existence of the Supernatural. Scribner Book Company. ISBN 0-684-17820-6.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Cutler WB. Lunar and menstrual phase locking. Am J Obstet Gynecol. 1980 Aug 1;137(7):834-9. PMID: 7405975.
Friedmann E. Menstrual and lunar cycles. Am J Obstet Gynecol. 1981 Jun 1;140(3):350. PMID: 7246643
Law SP. The regulation of menstrual cycle and its relationship to the moon. Acta Obstet Gynecol Scand. 1986;65(1):45-8. PMID: 3716780
Zimecki M. The lunar cycle: effects on human and animal behavior and physiology. Postepy Hig Med Dosw (Online). 2006;60:1-7. Review. PMID: 16407788 - ^ "Herbs For Premenstrual Syndrome". HerbalRemedies.com. 2004. Retrieved 2006-08-08.
External links
- Museum of Menstruation and Women's Health
- Leslie Botha-Williams, Women's Health Educator: A Woman's Guide to Understanding Her Hormone Cycle
- An Islamic answer for the question "What is the wisdom behind the prohibition on having intercourse with one's wife when she is menstruating or bleeding following childbirth?"
- Menstrual Suppression With Birth Control Pills
- On The Rag: Everything you need to know about your fertility cycles and menstruation...period - Article on the menstrual cycle by notable sex activist and educator Heather Corinna
- Menopause and Menstrual Cycles - WomensHealthChannel
- Early 70s Educational Film
- Patient Queries - Menstrual Cycle Queries related to Menstrual Cycle answered by Obstetricians & Gynaecologists
Hygiene products
- Love Your Blood: An info-zine on menstrual products and their alternatives
- The rags: paraphernalia of menstruation
- Eight Myths About Washable Menstrual Pads Dispelled
- Tampaction and The Bloodsisters Project- Menstrual activism against chlorine bleaching, excessive packaging, and negative attitudes toward menstruation in the West
