Cardiotocography
| Cardiotocography | |
|---|---|
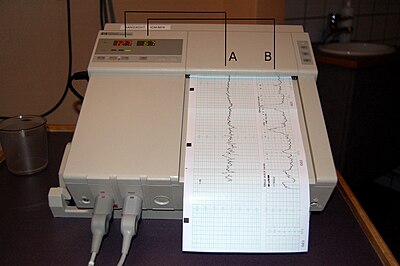
 A cardiotocograph recording fetal heart rate and uterine contractions | |
| ICD-9-CM | 75.32 |
| MeSH | D015148 |
In medicine (obstetrics), cardiotocography (CTG) is a technical means of recording the fetal heartbeat and the uterine contractions during pregnancy. The machine used to perform the monitoring is called a cardiotocograph, more commonly known as an electronic fetal monitor (EFM).
Fetal monitoring was invented by Doctors Alan Bradfield, Orvan Hess and Edward Hon. A refined (antepartal, non-invasive, beat-to-beat) version (cardiotocograph) was later developed for Hewlett Packard by Konrad Hammacher.
CTG monitoring is widely used to assess fetal wellbeing (how happy the unborn baby is).[1] A review found that in the antenatal period (before labour) there is no evidence to suggest that monitoring women with high-risk pregnancies benefits the mother or baby although research around this is old and should be interpreted with caution.[2] The same review found that computerised CTG machines resulted in lower numbers of baby deaths than the traditional CTG machines (as shown in picture). More up-to-date research is needed to provide more information around this practise.[3]
CTG monitoring can sometimes lead to medical interventions which are not necessarily needed.[4] Fetal vibroacoustic stimulation (sound played to the unborn baby through the mother’s abdomen) has been used to provoke the baby into being more active.[5] This can improve their CTG monitoring so that the mother does not have to be monitored for as long.[6] However the safety of this technique has not been fully assessed; hearing impairment, stress reactions and other effects should be investigated before this technique is used widely.[7]
Method
External cardiotocography- for continuous or intermittent monitoring The fetal heart rate and the activity of the uterine muscle are detected by two transducers placed on the mother’'s abdomen (one above the fetal heart and the other at the fundus). Doppler ultrasound provides the information which is recorded on a paper strip known as a cardiotocograph (CTG).[8]
Internal cardiotocography- uses an electronic transducer connected directly to the fetal scalp. A wire electrode is attached to the fetal scalp through the cervical opening and is connected to the monitor. This type of electrode is sometimes called a spiral or scalp electrode. Internal monitoring provides a more accurate and consistent transmission of the fetal heart rate than external monitoring because factors such as movement do not affect it. Internal monitoring may be used when external monitoring of the fetal heart rate is inadequate, or closer surveillance is needed.[9]
| Fetal Heart Rate monitoring | Uterine Contraction monitoring | |
|---|---|---|
| External | In this method, your health care provider straps an ultrasound transducer over your abdomen that will pick up the baby's heartbeat. The heartbeat will be recorded continuously on a paper strip. There may be another device strapped on top of your abdomen—a pressure gauge that measures the frequency of your contractions. The combination of these two measurements will provide detailed information as to how your baby is doing during labor. | The pressure-sensitive contraction transducer, called a tocodynamometer (toco) has a flat area that is fixated to the skin by a band around the belly. The pressure required to flatten a section of the wall correlates with the internal pressure, thereby providing an estimate of it.[10] |
| Internal | This method can only be used if membranes (fore-waters) and your cervix have ruptured either spontaneously or artificially.
An electrode is placed on the baby’s scalp to directly monitor the fetal heart rate. An electrode is called a fetal scalp electrode (FSE) |
To gauge the strength of your contractions,a small catheter (Intrauterine pressure catheter or IUPC) is placed in your uterus. Combined with an internal fetal monitor, an IUPC may give a more precise reading of the baby's heart rate and your contractions. |
A typical CTG reading is printed on paper and/or stored on a computer for later reference. A variety of systems for centralized viewing of CTG have been installed in a large number of maternity hospitals in industrialised countries, allowing simultaneous monitoring of multiple tracings in one or more locations. Display of maternal vital signs, ST signals and an electronic partogram are available in the majority of these systems. A few of them have incorporated computer analysis of cardiotocographic signals or combined cardiotocographic and ST data analysis.[11]
Interpretation

In the US, the Eunice Kennedy Shriver National Institute of Child Health and Human Development sponsored a workshop to develop a standardized nomenclature for use in interpreting intrapartum fetal heart rate and uterine contraction patterns. This nomenclature has been adopted by the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN), the American College of Obstetricians and Gynecologists (ACOG), and the Society for Maternal-Fetal Medicine.[15]
The Royal College of Obstetricians and Gynaecologists[16] and the Society of Obstetricians and Gynaecologists of Canada[17] have also published consensus statements on standardized nomenclature for fetal heart rate patterns.
Interpretation of a CTG tracing requires both qualitative and quantitative description of:
- Uterine activity (contractions)
- Baseline fetal heart rate (FHR)
- Baseline FHR variability
- Presence of accelerations
- Periodic or episodic decelerations
- Changes or trends of FHR patterns over time.
Uterine activity
There are several factors used in assessing uterine activity.
- Frequency- the amount of time between the start of one contraction to the start of the next contraction.
- Duration- the amount of time from the start of a contraction to the end of the same contraction.
- Intensity- a measure of how strong a contraction is. With external monitoring, this necessitates the use of palpation to determine relative strength. With an IUPC, this is determined by assessing actual pressures as graphed on the paper.
- Resting Tone- a measure of how relaxed the uterus is between contractions. With external monitoring, this necessitates the use of palpation to determine relative strength. With an IUPC, this is determined by assessing actual pressures as graphed on the paper
- Interval- the amount of time between the end of one contraction to the beginning of the next contraction.
The NICHD nomenclature[15] defines uterine activity by quantifying the number of contractions present in a 10-minute window, averaged over 30 minutes. Uterine activity may be defined as:
- Normal- less than or equal to 5 contractions in 10 minutes, averaged over a 30-minute window
- Tachysystole- more than 5 contractions in 10 minutes, averaged over a 30-minute window
Baseline fetal heart rate
The NICHD nomenclature[15] defines baseline fetal heart rate as: The baseline FHR is determined by approximating the mean FHR rounded to increments of 5 beats per minute (bpm) during a 10-minute window, excluding accelerations and decelerations and periods of marked FHR variability (greater than 25 bpm). There must be at least 2 minutes of identifiable baseline segments (not necessarily contiguous) in any 10-minute window, or the baseline for that period is indeterminate. In such cases, it may be necessary to refer to the previous 10-minute window for determination of the baseline. Abnormal baseline is termed bradycardia when the baseline FHR is less than 110 bpm; it is termed tachycardia when the baseline FHR is greater than 160 bpm.
Baseline FHR variability
The NICHD nomenclature[15] defines baseline FHR variability as: Baseline FHR variability is determined in a 10-minute window, excluding accelerations and decelerations. Baseline FHR variability is defined as fluctuations in the baseline FHR that are irregular in amplitude and frequency. The fluctuations are visually quantitated as the amplitude of the peak-to-trough in bpm. Using this definition, the baseline FHR variability is categorized by the quantitated amplitude as:
- Absent- undetectable
- Minimal- greater than undetectable, but less than or equal to 5 bpm
- Moderate- 6-25 bpm
- Marked- greater than 25 bpm
Accelerations
The NICHD nomenclature[15] defines an acceleration as a visually apparent abrupt increase in FHR. An abrupt increase is defined as an increase from the onset of acceleration to the peak in less than or equal to 30 seconds. To be called an acceleration, the peak must be greater than or equal to 15 bpm, and the acceleration must last greater than or equal to 15 seconds from the onset to return to baseline.[18] A prolonged acceleration is greater than or equal to 2 minutes but less than 10 minutes in duration. An acceleration lasting greater than or equal to 10 minutes is defined as a baseline change. Before 32 weeks of gestation, accelerations are defined as having a peak greater than or equal to 10 bpm and a duration of greater than or equal to 10 seconds.
Periodic or episodic decelerations
Periodic refers to decelerations that are associated with contractions; episodic refers to those not associated with contractions. There are four types of decelerations as defined by the NICHD nomenclature, all of which are visually assessed.[15]
- Early Deceleration: Usually symmetrical, gradual decrease and return of FHR associated with a uterine contraction. A 'gradual' deceleration has onset to nadir of 30 seconds or more. The nadir of the deceleration occurs at the same time as the peak of the contraction. In most cases the onset, nadir, and recovery of the deceleration are coincident with the beginning, peak, and ending of the contraction, respectively
- Late Deceleration: Usually symmetrical gradual decrease and return of the FHR, associated with a uterine contraction. A 'gradual' deceleration has onset to nadir of 30 seconds or more. The deceleration is delayed in timing, with nadir occurring after the peak of the contraction. As with early decelerations, the onset, nadir, and recovery of the deceleration occurs after the beginning, peak, and ending of the contraction, respectively.
- Variable Deceleration: Abrupt decrease in FHR, defined as from onset of the deceleration to the beginning of the FHR nadir of less than 30 seconds. The decrease in FHR is calculated from the onset to the nadir of the deceleration. The decrease in FHR is greater than or equal to 15 beats per minute, lasting greater than or equal to 15 seconds, and less than 2 minutes in duration. When variable decelerations are associated with uterine contractions, their onset, depth, and duration commonly vary with successive uterine contractions.
- Prolonged Deceleration: Decrease in FHR from baseline greater than or equal to 15 bpm, lasting greater than or equal to 2 minutes, but less than 10 minutes. A deceleration greater than or equal to 10 minutes is a baseline change.
Additionally decelerations can be recurrent or intermittent based on their frequency (more or less than 50% of the time) within a 20 min window.[15]
FHR pattern classification
The NICHD workgroup proposed terminology of a three-tiered system to replace the older undefined terms "reassuring" and "nonreassuring".[15]
- Category I (Normal): Tracings with all these findings present are strongly predictive of normal fetal acid-base status at the time of observation and the fetus can be followed in a standard manner:
- Baseline rate 110-160 bpm,
- Moderate variability,
- Absence of late, or variable decelerations,
- Early decelerations and accelerations may or may not be present.
- Category II (Indeterminate): Tracing is not predictive of abnormal fetal acid-base status, but evaluation and continued surveillance and reevaluations are indicated.
- Bradycardia with normal baseline variability
- Tachycardia
- Minimal or Marked baseline variability of FHR
- Accelerations: Absence of induced accelerations after fetal stimulation
- Periodic or Episodic decelerations: Longer than 2min but shorter than 10min; Recurrent late decelerations with moderate baseline variability
- Variable decelerations with other characteristics such as slow return to baseline, overshoots of "shoulders" seen (humps on either side of deceleration)
- Category III (Abnormal): Tracing is predictive of abnormal fetal acid-base status at the time of observation; this requires prompt evaluation and management:
- Absence of baseline variability with recurrent late or variable decelerations or bradycardia; or
- Sinusoidal fetal heart rate
See also
References
- ^ Grivell, RM; Alfirevic, Z; Gyte, GM; Devane, D (12 September 2015). "Antenatal cardiotocography for fetal assessment". The Cochrane database of systematic reviews. 9: CD007863. PMID 26363287.
- ^ Grivell, RM; Alfirevic, Z; Gyte, GM; Devane, D (12 September 2015). "Antenatal cardiotocography for fetal assessment". The Cochrane database of systematic reviews. 9: CD007863. PMID 26363287.
- ^ Grivell, RM; Alfirevic, Z; Gyte, GM; Devane, D (12 September 2015). "Antenatal cardiotocography for fetal assessment". The Cochrane database of systematic reviews. 9: CD007863. PMID 26363287.
- ^ Grivell, RM; Alfirevic, Z; Gyte, GM; Devane, D (12 September 2015). "Antenatal cardiotocography for fetal assessment". The Cochrane database of systematic reviews. 9: CD007863. PMID 26363287.
- ^ Tan, KH; Smyth, RM; Wei, X (7 December 2013). "Fetal vibroacoustic stimulation for facilitation of tests of fetal wellbeing". The Cochrane database of systematic reviews. 12: CD002963. PMID 24318543.
- ^ Tan, KH; Smyth, RM; Wei, X (7 December 2013). "Fetal vibroacoustic stimulation for facilitation of tests of fetal wellbeing". The Cochrane database of systematic reviews. 12: CD002963. PMID 24318543.
- ^ Tan, KH; Smyth, RM; Wei, X (7 December 2013). "Fetal vibroacoustic stimulation for facilitation of tests of fetal wellbeing". The Cochrane database of systematic reviews. 12: CD002963. PMID 24318543.
- ^ [1]. By Alfirevic Z, Devane D, Gyte GML, 2013.
- ^ [2] External and Internal Heart Rate Monitoring of the Fetus
- ^ Tocodynamometer. By Malcolm C Brown, 2000.
- ^ http://www.degruyter.com/view/j/jpme.2013.41.issue-1/jpm-2012-0067/jpm-2012-0067.xml
- ^ http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD006066.pub2/pdf
- ^ http://pennmedicine.adam.com/content.aspx?productId=14&pid=14&gid=000138
- ^ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1676479/pdf/bmj00006-0005.pdf
- ^ a b c d e f g h Macones GA, Hankins GD, Spong CY; et al. (2008). "The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring:update on definitions, interpretation, and research guidelines". Obstet Gynecol. 112: 661–666.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ NICE Guideline Intrapartum care: management and delivery of care to women in labour
- ^ SOGC Fetal health Surveillance: antepartum and intrapartum Consensus Guideline
- ^ Bailey, R. E. (2009). "Intrapartum fetal monitoring". American family physician. 80 (12): 1388–1396. PMID 20000301.
