Echocardiography
| Echocardiography | |
|---|---|
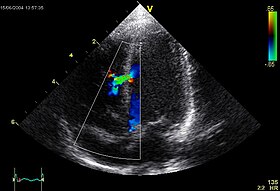 An abnormal echocardiogram: Image shows a midmuscular ventricular septal defect. The trace in the lower left shows the cardiac cycle and the red mark the time in the cardiac cycle when the image was captured. Colors are used to represent the velocity and direction of blood flow. | |
| ICD-9-CM | 88.72 |
| MeSH | D004452 |
| OPS-301 code | 3-052 |
| MedlinePlus | 003869 |


An echocardiogram, often referred to as a cardiac echo or simply an echo, is a sonogram of the heart. (It is not abbreviated as ECG, because that is an abbreviation for an electrocardiogram.) Echocardiography uses standard two-dimensional, three-dimensional, and Doppler ultrasound to create images of the heart.
Echocardiography has become routinely used in the diagnosis, management, and follow-up of patients with any suspected or known heart diseases. It is one of the most widely used diagnostic tests in cardiology. It can provide a wealth of helpful information, including the size and shape of the heart (internal chamber size quantification), pumping capacity, and the location and extent of any tissue damage. An echocardiogram can also give physicians other estimates of heart function, such as a calculation of the cardiac output, ejection fraction, and diastolic function (how well the heart relaxes).
Echocardiography can help detect cardiomyopathies, such as hypertrophic cardiomyopathy, dilated cardiomyopathy, and many others. The use of stress echocardiography may also help determine whether any chest pain or associated symptoms are related to heart disease. The biggest advantage to echocardiography is that it is not invasive (does not involve breaking the skin or entering body cavities) and has no known risks or side effects.
Not only can an echocardiogram create ultrasound images of heart structures, but it can also produce accurate assessment of the blood flowing through the heart by Doppler echocardiography, using pulsed- or continuous-wave Doppler ultrasound. This allows assessment of both normal and abnormal blood flow through the heart. Color Doppler, as well as spectral Doppler, is used to visualize any abnormal communications between the left and right sides of the heart, any leaking of blood through the valves (valvular regurgitation), and estimate how well the valves open (or do not open in the case of valvular stenosis). The Doppler technique can also be used for tissue motion and velocity measurement, by tissue Doppler echocardiography.
Echocardiography was also the first ultrasound subspecialty to use intravenous contrast. (See Contrast echocardiography)
Echocardiography is performed by cardiac sonographers, cardiac physiologists (UK), or physicians trained in echocardiography.
Recognized as the “Father of Echocardiography”, the Swedish physician Inge Edler (1911-2001), a graduate of Lund University, was the first of his profession to apply in diagnosing cardiac disease ultrasonic pulse echo imaging technique, which the acoustical physicist Floyd Firestone had developed to detect defects in metal castings. In fact, Dr. Edler in 1953 produced the first echocardiographs using an industrial Firestone-Sperry Ultrasonic Reflectoscope. In developing echocardiography, Edler worked with the physicist Carl Hellmuth Hertz, the son of the Nobel laureate Gustav Hertz and grandnephew of Heinrich Rudolph Hertz.[1][2]
Indications
Health societies recommend the use of echocardiography for initial diagnosis when a change in the patient's clinical status occurs and when new data from an echocardiogram would result in the physician changing the patient's care.[3] Health societies do not recommend routine testing when the patient has no change in clinical status or when a physician is unlikely to change care for the patient based on the results of testing.[3]
A common example of overuse of echocardiography when not indicated is the use of routine testing in response to a patient diagnosis of mild valvular heart disease.[4] In this case, patients are often asymptomatic for years before the onset of deterioration and the results of the echocardiogram would not result in a change in care without other change in clinical status.[4]
Transthoracic echocardiogram
A standard echocardiogram is also known as a transthoracic echocardiogram, or cardiac ultrasound. In this case, the echocardiography transducer (or probe) is placed on the chest wall (or thorax) of the subject, and images are taken through the chest wall. This is a noninvasive, highly accurate, and quick assessment of the overall health of the heart.
Transesophageal echocardiogram
This is an alternative way to perform an echocardiogram. A specialized probe containing an ultrasound transducer at its tip is passed into the patient's esophagus. This allows image and Doppler evaluation from a location directly behind the heart. This is known as a transœsophageal echocardiogram. Transesophageal echocardiograms are most often used when transthoracic images are suboptimal and when a more clear and precise image is needed for assessment. This test is performed in the presence of a cardiologist, registered nurse, and ultrasound technician. Conscious sedation and/or localized numbing medication may be used to make the patient more comfortable during the procedure.
Stress echocardiography
A stress echocardiogram, also known as a stress echo, uses ultrasound imaging of the heart to assess the wall motion in response to physical stress. First, images of the heart are taken "at rest" to acquire a baseline of the patient's wall motion at a resting heart rate. The patient then walks on a treadmill or uses another exercise modality to increase the heart rate to his or her target heart rate, or 85% of the age-predicted maximum heart rate (220 − patient's age). Finally, images of the heart are taken "at stress" to assess wall motion at the peak heart rate. A stress echo assesses wall motion of the heart; it does not, however, create an image of the coronary arteries directly. Ischemia of one or more coronary arteries could cause a wall motion abnormality which could indicate coronary artery disease. The gold standard test to directly create an image of the coronary arteries and directly assess for stenosis or occlusion is a cardiac catheterization. A stress echo is not invasive and is performed in the presence of a licensed medical professional, such as a cardiologist, and a cardiac sonographer.
Three-dimensional echocardiography

Three-dimensional echocardiography (also known as four-dimensional echocardiography when the picture is moving) is now possible, using a matrix array ultrasound probe and an appropriate processing system. This enables detailed anatomical assessment of cardiac pathology, particularly valvular defects,[5] and cardiomyopathies.[6] The ability to slice the virtual heart in infinite planes in an anatomically appropriate manner and to reconstruct three-dimensional images of anatomic structures make it unique for the understanding of the congenitally malformed heart.[7] Real-time three-dimensional echocardiography can be used to guide the location of bioptomes during right ventricular endomyocardial biopsies, placement of catheter-delivered valvular devices, and in many other intraoperative assessments.[8] The 3D Echo Box developed by the European Association of Echocardiography offers a complete review of three-dimensional echocardiography.
Three-dimensional echocardiography technology may feature anatomical intelligence, or the use of organ-modeling technology to automatically identify anatomy based on generic models. All generic models refer to a dataset of anatomical information that uniquely adapts to variability in patient anatomy to perform specific tasks. Built on feature recognition and segmentation algorithms, this technology can provide patient-specific three-dimensional modeling of the heart and other aspects of the anatomy, including the brain, lungs, liver, kidneys, rib cage, and vertebral column.[9]
Contrast echocardiography
Contrast echocardiography, or Contrast-enhanced ultrasound is the addition of ultrasound contrast medium, or imaging agent, to traditional ultrasonography. The ultrasound contrast is made up of tiny microbubbles filled with a gas core and protein shell. This allows the microbubbles to circulate through the cardiovascular system and return the ultrasound waves creating a highly reflective image. The most commonly used types of ultrasound contrast are known as: Definity® (definityimaging.com) and Optison® (optisonimaging.com). Both have been approved by the FDA. There are multiple applications in which contrast-enhanced ultrasound can be useful. The most commonly used application is in the enhancement of LV endocardial borders for assessment of global and regional systolic function. Contrast may also be used to enhance visualization of wall thickening during stress echocardiography, for the assessment of LV thrombus, or for the assessment of other masses in the heart. Contrast echocardiography has also been used to assess blood perfusion throughout myocardium in the case of coronary artery disease. The Contrast Echo Box developed by the European Association of Echocardiography, and the American Society of Echocardiography Contrast Zone both offer a complete review of Contrast Echocardiography.
Accreditation
Accreditation varies by country.
This section needs expansion. You can help by adding to it. (November 2014) |
Australia
Australia has high standards for imaging practices through Accreditation organizations where policies of the Echo practice need to be submitted and approved. All sonographers involved in echo need to be highly trained and registered.
Europe
At European level [10] individual and laboratory accreditation is provided by the European Association of Echocardiography (EAE). Three subspecialties for individual accreditation: Adult Transthoracic Echocardiography (TTE), Adult Transesophageal Echocardiography (TEE) and Congenital Heart Disease Echocardiography (CHD).
UK
In the UK, accreditation is regulated by the British Society of Echocardiography. Accredited radiographers, sonographers, or other professionals must complete a logbook and pass an exam.[11]
United States
The "Intersocietal Accreditation Commission for Echocardiography” (IAC) sets standards for echo labs across the US. Cardiologists and sonographers who wish to have their laboratory accredited by IAC must comply with these standards. The purpose of accreditation is to maintain quality and consistency across echocardiography labs in the United States. Accreditation is offered in adult and pediatric transthoracic and transesophageal echocardiography, as well as adult stress and fetal echo. Accreditation is a two part process; first each facility will conduct a detailed self-evaluation, paying close attention to the IAC standards and Guidelines. The facility will then complete the application and submit actual case studies to the board of directors for review. Once all requirements have been met, the lab will receive IAC certification. IAC certification is a continual process and must be maintained by the facility, this may include audits or site visits by the IAC. There are several states in which Medicare and/or private insurance carriers are requiring either the accreditation of the laboratory and/or sonographer credentialing, for reimbursement of echocardiograms.[3]
Sonographer credentialing
There are two credentialing bodies in the United States for sonographers, the Cardiovascular Credentialing International (CCI) Established in 1968 and the American Registry for Diagnostic Medical Sonography (ARDMS) Established in 1975. Both CCI and ARDMS have earned the prestigious ANSI-ISO 17024 accreditation for certifying bodies from the International Organization for Standardization (ISO). Accreditation is granted through the American National Standards Institute (ANSI). Recognition of ARDMS programs in providing credentials has also earned the ARDMS accreditation with the National Commission for Certifying Agencies (NCCA). The NCCA is the accrediting arm of the National Organization for Competency Assurance (NOCA). Established in 1977 as a nonprofit organization, NOCA is a leader in setting.
Under both credentialing bodies sonographers must first document completion of prerequisite requirements which contain both didactic and hands on experience in the field of ultrasound. Applicants must then take a comprehensive exam demonstrating knowledge in both the physics of ultrasound and the clinical competency related to their specialty. Credentialed sonographers are then required to maintain competency in their field by obtaining a certain number of Continuing Medical Education credits, or CME’s.
In 2009, New Mexico and Oregon became the first two states to require licensure of sonographers.
Australia requires all sonographers to be registered with ASAR. This is reviewed and accepted providing the sonographer gains points every 3 years for ongoing education.
Physician credentialing
In the US physicians are required to be credentialed by the National Board of Echocardiography (NBE) in order to read or perform echocardiograms. The purpose of the NBE is to assess the level of knowledge of a practitioner in echocardiography, maintain a high level of standard in the field, and serve the public by maintaining a high level of patient care. Similar to sonographer credentialing, physicians are required to document specialized training in cardiovascular disease, and specifically echocardiography, as well as taking a comprehensive exam demonstrating knowledge in the field. Certification is available in Transthoracic, Transesophageal, and Stress echocardiography. Physicians are also required to maintain their credentials by taking a recertification exam.
American Society of Echocardiography
The American Society of Echocardiography (ASE) is a professional organization made up of physicians, sonographers, nurses, and scientists involved in the field of echocardiography. Echocardiography was invented by Milton R. Hejtmancik, MD, from which he was awarded the AMA Billings Gold Medal in 1972 for his research. The Society was founded in 1975 and is the largest international organization for cardiac imaging. The American Society of Echocardiography is an organization from which sonographers and physicians may obtain Continuing Medical Education Credits, as well as interact with other health professionals from across the country and the world. The ASE is committed to maintaining and improving the profession of cardiac ultrasound through education, advocacy, research, and innovation. The first president of the ASE was Harvey Feigenbaum, MD in 1975. The ASE produces a monthly circulation known as the Journal of the American Society of Echocardiography (JASE) which highlights important educational and research advances in the field of echocardiography. The ASE not only focuses on improving the profession of echocardiography in the US, but also focuses on bringing echocardiography to the world through ASE Global. The ASE currently has educational/humanitarian activities in China, India, Japan, Korea, Australia and New Zealand, Europe, Canada, and South and Central America. The American Society of Echocardiography also supports current and future sonographers and physicians by awarding grants and scholarships to deserving individuals. The funding for these awards is provided by the ASE Foundation. One of the most important rolls that the ASE plays is providing their recommendations through the ASE Guidelines and Standards. ASE guideline documents may be accessed at www.asecho.org/guidelines. These documents provide recommendations for image acquisition and interpretation based on the gathered opinions of experts in the field. These documents provide a resource and educational opportunities for sonographers and physicians in the field, so that they may maintain excellent quality and consistency in their echocardiograms.
See also
References
- ^ Batohi, Bhavna; Sidhu, Paul S. (2014). "The Development of Ultrasound for Clinical Use". In Thompson, Gilbert (ed.). Pioneers of Medicine Without a Nobel Prize. World Scientific. pp. 141–159. ISBN 978-1-78326-386-8. Retrieved 23 September 2016.
- ^ Singh, Siddharth; Goyal, Abha (2007). "The origin of echocardiography: A Tribute to Inge Edler". Tex Heart Inst J. 34 (4): 431–438. PMC 2170493.
- ^ a b Douglas, P. S.; Garcia, M. J.; Haines, D. E.; Lai, W. W.; Manning, W. J.; Patel, A. R.; Picard, M. H.; Polk, D. M.; Ragosta, M.; Ward, R. P.; Douglas, R. B.; Weiner, R. B.; Society for Cardiovascular Angiography Interventions; Society of Critical Care Medicine; American Society of Echocardiography; American Society of Nuclear Cardiology; Heart Failure Society of America; Society for Cardiovascular Magnetic Resonance; Society of Cardiovascular Computed Tomography; American Heart Association; Heart Rhythm Society (2011). "ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography". Journal of the American College of Cardiology. 57 (9): 1126–1166. doi:10.1016/j.jacc.2010.11.002. PMID 21349406.
- ^ a b American College of Cardiology, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, American College of Cardiology, retrieved August 17, 2012
- ^ Poh KK, Levine RA, Solis J, Shen L, Flaherty M, Kang YJ, Guerrero JL, Hung J. (2008). "Assessing aortic valve area in aortic stenosis by continuity equation: a novel approach using real-time three-dimensional echocardiography". J 29 (20): 2526–35. doi:10.1093/eurheartj/ehn022. PMC 2721715. PMID 18263866.
- ^ Goland S, Czer LS, Luthringer D, Siegel RJ. (2008). "A case of arrhythmogenic right ventricular cardiomyopathy". Can J Cardiol 24 (1): 61–2. doi:10.1016/S0828-282X(08)70551-8. PMC 2631252. PMID 18209772.
- ^ Impact of Multiplanar Review of Three-Dimensional Echocardiographic Data on Management of Congenital Heart Disease. Ann. Thorac. Surg., September 2008; 86: 875–881)
- ^ Comparison of Fluoroscopic versus Real Time Three-Dimensional Transthoracic Echocardiographic Guidance of Endomyocardial Biopsies. D Platts, M Brown, G Javorsky, C West, N Kelly, D Burstow. European Journal of Echocardiography (2010) doi:10.1093/ejechocard/jeq036
- ^ Rodriguez,Gall.“Innovations Revolutionaize Medical Imaging”.NEMA electroindustry
- ^ [1] ESCardio
- ^ [2] BSEcho - Exam
External links
- American Society of Echocardiography
- British Society of Echocardiography
- An interactive learning site for 3D Echocardiography
- International Society of Cardiovascular Ultrasound
- European Association of Echocardiography
- VIRTUAL TEE – online self-study and teaching resource
- VIRTUAL Transthoracic Echocardiography - online self-study and teaching resource
- Echobasics – free online echocardiography tutorial
- Algorithms and System for Digital Echocardiogram Video Indexing and Su
- CT2TEE – transesophageal echocardiography simulator
- Wikiecho – Free Echocardiography encyclopedia by the European Association of Cardiovascular Imaging (EACVI)
- Basic ultrasound, echocardiography and Doppler for clinicians
